PHILOS plating has a good functional outcome. However, proper patient selection, thorough knowledge of the anatomy, and biomechanical principles are the pre-requisites for a successful surgery.
Dr. Setu Kaneria, Department of Orthopaedic Surgery, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Dr D. Y. Patil University, Pimpri, Pune, Maharashtra, India. E-mail: setu.kaneria141@gmail.com
Introduction: The purpose of the study was to assess the functional outcome of proximal humerus fractures (2 part, 3 part, and 4 part) managed with a proximal humerus internal locking system (PHILOS).
Materials and Methods: This retrospective study included 27 cases of proximal humerus fractures managed surgically between February 2021 and February 2022 with a proximal humerus internal locking system (PHILOS) plate. NEER classification was used to categorize the fractures. Functional assessment was done using Constant Murley’s shoulder score and disabilities of the arm, shoulder, and hand. Subjects having metastatic and pathological fractures; associated fractures in the ipsilateral limb; having major nerve injury and cases of open fracture were excluded from this study.
Results: The mean age was 55.63 ± 10.37 years. Of the total 27 cases of proximal humerus fractures, functional outcome was excellent (score 85–100) in 3.70% (n = 1) cases, good (score 71–85) in 81.49% (n = 22) cases, moderate (score 56–70) in 14.81% (n = 4), and poor (score 0–55) in none of the (n = 0) cases. In 92.60% of cases, follow-up showed no complications. Varus collapse and subacromial impingement, both occurring in 3.70% (n = 1) of the subjects, were noted in this study.
Conclusion: Based on the findings of this retrospective study, it can be opined that PHILOS plating appears to be a secure option for proximal humerus fracture cases. It offers solid fixation, prompt mobilization, and excellent functional outcomes as observed in this study. In addition, very few post-operative complication rates again support our conclusion.
Keywords: PHILOS, proximal humerus fracture, elderly individuals, disabilities of the arm, shoulder, and hand score, osteosynthesis.
Proximal humerus fracture is the third most common fracture occurring in elderly individuals. Displaced and comminuted fractures of the proximal humerus pose difficult management problems for the orthopedic surgeon. There is different consensus concerning the best treatment option for each patient, either by non-operative management, internal fixation or by prosthetic replacement.[1] Open reduction and internal fixation of displaced proximal humerus fractures is indicated in patients with 2- and 3-part fractures with significant displacement, and in some 4-part fractures, especially in younger patients.[2] Short-term results after the treatment of displaced proximal humerus fractures with a new design of stable angle plate have been promising on the whole, but longer-term outcome reports are still lacking.[3] According to Neer, displaced three- and 4-part fractures, especially those with dislocation of the humeral head, are difficult to treat appropriately.[4] Various techniques from open or closed reduction and fixation by nailing or plating to primary hemiarthroplasty and reversed shoulder arthroplasty exist to address the individual characteristics in each case, attributed by the fracture’s morphology (e.g., pattern, medial hinge, vascular supply), the patient’s specifics (e.g., age, gender, and general bone quality), and the surgeon’s personal experience and preference.[5] The purpose of the current study was to assess the functional outcome on long-term functional outcomes on patients treated by locking plates for proximal humeral fractures.
[1] Sproul et al., “A Systematic Review of Locking Plate Fixation of Proximal Humerus Fractures.”
[2] Sproul et al.
[3] Regazzoni and Gross, “Clinical Longer-Term Results After Internal Fixation of Proximal Humerus Fractures With a Locking Compression Plate (PHILOS).”
[4] Neer, “Displaced Proximal Humeral Fractures.”
[5] Ockert et al., “Long-Term Functional Outcomes (Median 10 Years) after Locked Plating for Displaced Fractures of the Proximal Humerus.”
Study design
Between February 2021 and February 2022, 27 subjects having proximal humerus fracture underwent MIPO through a “deltoid pectoral” technique using the Philos® system. In the modern-day have a look at, this cohort became approached and analyzed again to reap long-term final results on these patients. The disabilities of the arm, shoulder, and hand (DASH) rating become used as a basic score to measure functional outcome at 12-month follow-up. It is 30-object, self-record, survey form designed to assess physical pastime and signs and symptoms in patients with several musculoskeletal issues of the upper limb. It is composed of sections: The incapacity/symptom phase and the optional game/song or work phase, all sprint rating levels from zero to 100, with zero being the high-quality viable score. Constant Murley’s shoulder (CMS) score was also used additionally for the assessment of functional outcome of shoulder function. The CMS is classified into four sections: pain (15 points), activities of daily living (20 points), strength (25 points), and range of motion (40 points); the higher the score, the higher the quality of the function, for a maximum score of 100 points scale [1]. Normal Murley’s shoulder (CMS) score is graded as poor (0–55), fair (56–70), good (71–85), and excellent (86–00). Radiographs were collected at each follow-up to assess bone healing and record complications such as fractures, recession, varus, and valgus angulation. Screw removal, plate fracture/removal, malunion, non-union, or avascular necrosis of the humeral was considered failure.
Inclusion criteria for the study included
Proximal humerus fractures due to trauma (NEER’s type 2-part, 3-part, and 4-part fracture)
Patients greater than equal to 40 years of age
At least 12-month follow-up.
Pathological conditions, rehabilitation after other primary treatments, contralateral shoulder injuries, and conditions such as stroke or cognitive impairment that prevented participation in subsequent treatments were excluded from the study. The proposed document was approved by the Regional Ethics Committee.
Baseline evaluations
The average age of the 27 patients included in this study was 55.63 ± 10.37 years and 40.74% were women. At the time of surgery, eight patients had a known history of hypertension, and four patients were diagnosed with diabetes. None of the patients had cancer and no patients had been diagnosed with dementia at the time of participation in the study.
Operative procedure
Evidence for operative treatment was a varus displacement of >20°, a valgus displacement of >40°, an improved reclination>30°, a lateral displacement of >½ diaphyseal diameter, and/or displacement of the greater and/or lesser tubercle of >5–10 mm [2]. The surgery is performed by an experienced senior surgeon, with the patient under anesthesia and lying on the radiolucent table and beach chair. Interscalene blockade was applied as standard perioperative analgesia unless the patient refused. All patients received prophylactic intravenous antibiotics immediately before surgery. Deltopectoral approach was used for the fixation of fractures (open reduction and internal fixation). Humeral excursion and position of the greater and lesser tubercles were restored. No bone graft was used to support fixation. During surgery, the rotator cuff is evaluated for a full-thickness rotator cuff tear. Proximal humerus internal locking system (PHILOS) was used for all patients. The screw is carefully inserted into the subchondral layer without penetrating the bone. During the entire surgical procedure, bone reduction and screw accuracy are checked using multiplanar fluoroscopy. In addition, humeral rotation was performed using a radiography machine to check whether the subchondral position of the screws was correct. When required, screws are replaced to acquire the favored function of the screw tip relative to the subchondral bone. The post-operative rehabilitation protocol includes monitoring a passive and lively variety of movement from the 1st day after surgical treatment. For the primary 6 weeks, abduction and flexion as much as 60 without pressured external rotation had been permitted. Thereafter, energetic physical activities with a complete variety of motion were commenced.
Follow-ups
Patients were prospectively observed from the time of operation and longitudinally followed up at 6 weeks, 3 months, 6 months, and 12 months. During follow-up, patients were examined and interviewed in accordance with the standard manner. Physical examination includes shoulder movement, strength, constant score, and radiographs taken in two planes (anterior-posterior and Neer view). All patients were assessed with shoulder function using the DASH questionnaire at a final follow-up visit[1].
[1] Hudak, Amadio, and Bombardier, “Development of an Upper Extremity Outcome Measure.”
This study included data from all 27 cases of proximal humerus fracture treated surgical with PHILOS plating. Of the 27 cases, they were divided according to 2 age groups, 20–45 years (n = 9, 33.34%) and 46–80 years (n = 18, 66.66%), with mean age of 55.63 ± 10.37. Gender wise male (n = 16, 59.26%) outnumbered the female (n = 11, 40.74%). The ratio between male and female was 16:9. Demographic details of the study are shown in Table 1. Incidence of fracture and mechanism of injury was found to be almost equally on both sides, left (n = 14, 51.85%) and right (n = 13, 48.15%), RTA (n = 14, 51.85%), and fall (n = 13, 48.15%). Neer pattern 3 part fractures were the most common fractures in our study population, accounting for 55.56% (15/27) of patients, while 2 part fractures comprised 33.34% (9/27) and 4 part fractures comprising 11.10% (3/27) as shown in Fig. 1.
An assessment of the range of motion was done and the following observations were made. At 6 weeks, 62.96% of the patients (17 of 27) had flexion below 60°, and 62.96% in 6 months (17 of 27) were in 90–120° range. At 12 months, 74% (20 of 27) were in the range of 120–180 as shown in Table 2. Therefore, we found that bending increased over time was significant (P < 0.05 using the Chi-square test). At 6 weeks, abduction was <60° in 66.67% (18 of 27) patients. At 3 months, 59.26% (16 of 27 patients) had incontinence in the range of 60–90°. 59.26% (16 of 27) patients at 6 months were in the range of 90–120°. At 12 months, 7037% (19 of 27) were in the range of 120–180°, as shown in Table 3 (P < 0.05 using Chi-square test). At 6 weeks, 15 of 27 patients had 30–60° of external rotation; at 3 months, 22 of 27 patients had 30–60° of external rotation; and finally, at 12 months, 26 patients had external rotation. It was concluded that there was an improvement in the degree of external rotation at 12 months as shown in Table 4 and the results were significant (P < 0.05 using Chi-square test). At 6 weeks, 15 of 27 patients had 30–60° of internal rotation; at 3 months, 21 of 27 patients had 30–60° of internal rotation; and at 6 months, 17 patients had internal rotations. 17 of 27 patients had 60–90° internal rotation at 6 months and at 12 months, 22 of 27 patients had an internal rotation of 60–90° of internal rotation as shown in Table 5, thus showing improvement in the range of internal rotation in our study with time (P < 0.05 using the Chi-square test). Among 27 patients who underwent operations, follow-up revealed no complication in 92.60% of cases (n = 25), and post-operative complication seen was subacromial impingement in 3.70% (n = 1) and varus collapse in 3.70% (n = 1) subjects (Table 6).
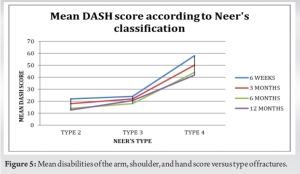
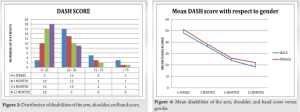
The data showed that in the study population, the increase in constant Murley shoulder scores from 6 weeks to 3 months and from 3 months to 6 months corresponded to the significant effect at 12 months, as shown in Table 7 (P < 0.05 using Chi-square test). The CMS at ≥12 months was reported, and the mean was 75.6 ± 6.64. According to the CMS, functional outcome was noted as excellent (score 85–100) in 3.70% (n = 1) cases, good (score 71–85) in 81.49% (n = 22) cases, moderate (score 56–70) in 14.81% (n = 4), and poor (score 0–55) in none of the (n = 0) cases as shown in Table 8 and Fig. 2. The DASH score at ≥1 year was mentioned by 16 studies, and the mean was 20.5 points as shown in Figs. 3, 4, 5. (95% C.I. 16.6–24.3 points) [3].






In our series of 27 patients who presented to a non-randomly selected center and underwent surgical treatment of displaced and unstable proximal humeral fractures using a proximal humerus locking plate, we found that the outcomes of most patients were comparable to other patients. In their study, Buecking et al. found that the operating time was lower when compared to our study (94 ± 10.2 min) using the fixed-effect model [4], blood loss (149.7 ± 18.95) mL almost similar when compared to Liu et al. (150.2 ± 48.9) [5]. Although surgery times are longer in some cases than others depending to the bone type, the difference in surgery time between the groups is not significant. Of the 27 patients, 14 (51.85%) had a history of traffic accident and 13 (48.15%) had a history of falling. The mean CMS at 12 months was reported at 75.6 ± 6.64. According to the study Sproul et al., the average Murley shoulder score is 74 [6]. When a locking plate was used to repair a fracture in the proximal humerus, patient’s mean CMS absolute CS (95% confidence interval [CI], 9.8–10.1) at 10-year follow-up was 75.3 [7]. According to this study, CS was excellent (86–100) in 44% of cases, good (71–85) in 19% of cases, moderate (56–70) in 21% of cases, and poor (0–55) in 16% of cases [7]. In this study, the complications were varus collapse and subacromial impingement, both occurring in 3.70% (n = 1) of the subjects which were less when compared to outcomes of the study conducted by Sproul et al. [6] In this 16.3% of cases, the authors noted varus malunion and subacromial impingement in 4.8% [6]. In another review, Thanasas et al. addressed an incidence of 5.5% in a comprehensive review of 12 articles on humeral bone [8]. Proper plate placement is equally important for good clinical outcome in these fractures. Unlike non-locking plates, these plates are anatomically pre-designed, so even the slightest change will cause shoulder impingement. According to AO – OTA principles, the best position of the uppermost part of the plate is 5 mm–8 mm distal to the greater tubercle. Mean DASH score of the study was 26.1, and the standard deviation is approximately 15.0. When compared to Ockert et al., the mean DASH score at 10 years of follow-up was 23.8 (95% CI, 15.4–32.1), suggesting there was not much difference between both studies [7]. The DASH score was also used in five of the studies with an average score of 26.6 [9-13]. In our study, the two most used scores were CMS and DASH: The CMS at ≥12 months was reported, the mean was 75.6 ± 6.64 points, and the second had mean of 26.1, and the standard deviation is approximately 15 which was compared to a systematic review and meta-analysis by Oldrini et al. which showed CMS mean as 70.8 points and DASH score at ≥1 year was mentioned by 16 studies, and the mean was 20.5 points (95% C.I. 16.6–24.3 points) [3].
3 part and 4 part fractures according to Neer’s classification, in elderly patients population can be effectively fixed by PHILOS plating with optimal surgical long-term outcomes. If proper surgical technique used, complications can be minimized. PHILOS plating provides stable and over fixation of humerus fractures which allow early rehabilitation and range of motion exercise in patients. We propose to have a study with a larger group of patients to look at long-term results.
Angular stability achieved using PHILOS plating in elderly population along with early post-operative mobilization helps the patient to attain better shoulder range of motion and return to activity faster.
References
- 1.Constant CR, Gerber C, Emery R, Søjbjerg J, Gohlke F, Pascal B. A review of the Constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg 2008;17:355-61. [Google Scholar]
- 2.Neer CS 2nd. Displaced proximal humeral fractures: PART II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am 1970;52:1090-103. [Google Scholar]
- 3.Oldrini LM, Feltri P, Albanese J, Marbach F, Filardo G, Candrian C. PHILOS synthesis for proximal humerus fractures has high complications and reintervention rates: A systematic review and meta-analysis. Life (Basel) 2022;12:311. [Google Scholar]
- 4.Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures? Clin Orthop Relat Res 2014;472:1576-85. [Google Scholar]
- 5.Liu B, Wang X, Wang C, Jiao Z, Chen W. Displaced proximal humerus fractures treated with ORIF via the deltoid interfascicular approach vs the deltopectoral approach: A prospective case-control study. Medicine (Baltimore) 2022;101:e29075. [Google Scholar]
- 6.Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury 2011;42:408-13. [Google Scholar]
- 7.Ockert B, Siebenbürger G, Kettler M, Braunstein V, Mutschler W. Long-term functional outcomes (median 10 years) after locked plating for displaced fractures of the proximal humerus. J Shoulder Elbow Surg 2014;23:1223-31. [Google Scholar]
- 8.Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: A systematic review. J Shoulder Elbow Surg 2009;18:837-44. [Google Scholar]
- 9.Rouleau DM, Laflamme GY, Berry GK, Harvey EJ, Delisle J, Girard J. Proximal humerus fractures treated by percutaneous locking plate internal fixation. Orthop Traumatol Surg Res 2009;95:56-62. [Google Scholar]
- 10.Helwig P, Bahrs C, Epple B, Oehm J, Eingartner C, Weise K. Does fixed-angle plate osteosynthesis solve the problems of a fractured proximal humerus? Acta Orthop 2009;80:92-6. [Google Scholar]
- 11.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures [corrected]. J Bone Joint Surg Am 2008;90:233-40. [Google Scholar]
- 12.Howard L, Berdusco R, Momoli F, Pollock J, Liew A, Papp S, et al. Open reduction internal fixation vs non-operative management in proximal humerus fractures: A prospective, randomized controlled trial protocol. BMC Musculoskelet Disord 2018;19:299. [Google Scholar]
- 13.Shahid R, Mushtaq A, Northover J, Maqsood M. Outcome of proximal humerus fractures treated by PHILOS plate internal fixation. Experience of a district general hospital. Acta Orthop Belg 2008;74:602-8. [Google Scholar]