Terrible triad elbow management should focus on bony as well as soft-tissue components.
Dr. Dheeraj Attarde, Department of Orthopedics, Sancheti Institute of Orthopaedics and Rehabilitation, Pune, Maharashtra, India. E-mail: dheerajattarde@yahoo.co.in
Introduction: The “terrible triad” injury of the elbow, consisting of fractures of the coronoid process and radial head along with posterolateral elbow dislocation and refractory instability, has historically led to poor functional outcomes. Traditional treatment focused on bony injuries, but it is now recognized that soft-tissue injuries must also be addressed. Surgical management aims to restore bony and soft-tissue stabilizers, including fixation of the coronoid process and radial head, repair of ligament complexes, and reduction of elbow dislocation. Studies emphasize the importance of early reduction and tailored treatment. This study discusses means and methods of treating this complex injury, highlighting the significance of addressing both bony and soft-tissue injuries for better functional outcomes.
Materials and Method: This is a prospective study conducted at a single center and involved 27 consecutive patients diagnosed with terrible triad injuries around the elbow. The objective was to evaluate functional outcomes and complications associated with surgical treatment of terrible triad injuries around the elbow. From July 2017 to October 2018, 27 patients with terrible triad injuries around the elbow were operated on and evaluated for a minimum of 1 year in terms of functional results using the mean elbow performance score (MEPS) and VAS score. The surgical protocol included coronoid fixation or repair of the anterior capsule, radial head fixation or arthroplasty, and repair of the lateral collateral ligament (LCL) in a sequential manner. The medial collateral ligament was repaired if the elbow remained unstable. On follow-up, mean MEPS scores improved significantly. The final mean range of motion of the operated upper limb was as follows: 28.5° of extension deficit (standard deviation [SD] 9.07, range, 10°–40°), 117.5° of flexion (SD 13.18, range, 90°–130°), 70.9° of supination (SD 10.19, range, 40°–85°), and 65.5° of pronation (SD 9.54, range, 40°–80°) at the end of 1 year. A total of 12 patients had complications. Out of the 12 patients, three had elbow arthritis, two had heterotopic ossification, three had radial nerve neuropraxia, two patients had elbow stiffness, and two patients suffered from ulnar nerve neuropathy.
Conclusion: Surgical intervention in terrible triad injuries around the elbow in the form of coronoid fixation, radial head fixation, or arthroplasty and soft-tissue repair around the elbow gives satisfactory results at the end of 1 year. Addressing each and every component of fracture in a sequential and step-wise manner is associated with good functional outcomes at the end of 1 year.
Keywords: Terrible triad injuries around the elbow, coronoid process fracture, radial head fracture, elbow instability, lateral collateral ligament, complications.
Hotchkiss [1] first introduced the term “terrible triad” to describe fractures of the coronoid process and radial head along with posterolateral elbow dislocation and refractory instability. The name was coined as most of these injuries led to poor functional outcomes. Conventionally, treatment of this terrible triad injury (TTI) complex focused on the pattern of the bony injuries, but it has become apparent that equal attention should also be paid to soft-tissue injuries [2]. Chen [3] et al. concluded that the traditional non-operative methods have very poor results because of recurrent instability and long-term fixation-induced stiffness. The principle of surgical management is based on two main objectives: Restoration of bony stabilizers (radial head and coronoid process) and soft-tissue stabilizers (radial collateral ligament) reconstruction [4]. Miyazaki et al. [5] concluded that the stable fixation of the coronoid process; restoring the anatomy of the radial head by means of fixation of the fracture or radial head replacement, obtaining lateral stability through repairing the lateral ligament complex, repairing the medial collateral ligament (MCL) if the instability still persists as the key to prevent residual instability. Broberg and Morrey [6] concluded that in view of the poor prognosis, the injury should be treated with early reduction of the elbow dislocation and treatment of radial head and coronoid fracture according to its type. The objective of our study was to report the means and methods of treating this difficult condition and to discuss the functional outcomes obtained and complications associated with it. Significantly good outcomes can be obtained if each component is addressed in a sequential manner and by giving equal attention to restoring the bony as well as soft-tissue injuries.
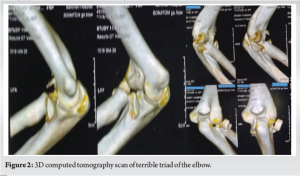
A prospective study was performed after obtaining approval from the Institutional Ethical Review Board of our institution and appropriate consent. Twenty-seven patients with TTI around the elbow were included in this study. Patients above 18 years of age with terrible triad injuries around the elbow managed surgically were included in this study while exclusion criteria were patients with cases with previous infection around the elbow, any associated fractures of the upper limb interfering with the assessment, and pediatric elbow fractures. Out of 27 patients, 17 (63%) were males and 10 (37%) were females. The mean age of presentation was 41.33 years (standard deviation [SD] ± 15.72, range 20–73 years). The most common mode of injury was due to motor vehicle accidents involving two-wheelers in 55.5% of our subjects followed by slip and fall in 22.2%, fall from height in 14.8%, and finally blunt trauma in 7.4%. All patients were assessed with radiographs – anteroposterior and lateral views also computer tomographic scans with 3D reconstruction done to asses fracture patterns and to facilitate pre-operative planning. The selected patients were classified as per Regan–Morrey classification for coronoid fractures and Mason–Johnston classification for radial head fractures
All patients were operated in a supine position with the operated arm resting over the hand table. Examination under anesthesia was performed before starting surgery in all patients. Laterally, radial head fractures were exposed through Kocher’s or posterolateral approach to the elbow. Through this approach tip of the coronoid process, lateral collateral ligament (LCL) and radial head are addressed in that order. Radial head replacement is preferred over fixation if the radial head fracture is comminuted. If the coronoid fracture fragment is not visualized through the posterolateral approach, a separate anteromedial approach is carried out. If the elbow is still found to be unstable, the MCL is repaired through the same anteromedial approach. LCL was repaired in all patients, whereas MCL repair was decided after on valgus stress test under fluoroscopy for instability. If the elbow is still found to be unstable after ligament and bony reconstruction, then a hinged external fixator is applied to achieve stability of the elbow (Table 1). Out of 27 cases, coronoid fixation was done in 21 patients, whereas six patients were not operated for coronoid fractures because of small coronoid chip fractures not amenable to fixation. Twenty-two patients had radial head communication and therefore underwent radial head replacement; in three patients, radial head open reduction and internal fixation were performed as these were amenable to fixation, and in one patient, hinged elbow external fixator was applied whereas in one patient, no treatment of radial head fracture was done. LCL was repaired in all patients; in 23 patients, LCL was repaired with sutures; and in four patients, suture anchors were used because the LCL tear was associated with bony avulsion. Fourteen patients were operated on for MCL injury as these elbows were unstable after LCL repair whereas 13 patients underwent no treatment as these patients showed stability after LCL repair. Among the 14 patients operated on for MCL injury, in 11 patients, suture anchors were used as they had bony avulsion whereas in three patients, MCL suturing was done. Postoperatively above elbow back slab was applied for 2 weeks to allow wound healing. Sutures and slab removal were done on the 14th post-operative day. At the end of 2 weeks, active and passive gentle elbow range of motion exercises started. Follow-up was done at 3-week, 3-month, 6-month, and 12-month post-operation. They were assessed clinically, radiographically, and functionally with VAS scores and mean elbow performance score (MEPS) postoperatively at 3 months, 6 months, and 12 months. Pro forma was filled on each visit and the data obtained was tabulated and conclusions were drawn after assessing the data.
Follow-up mean MEPS scores improved significantly from 72.03 (SD ± 12.19, range 45–90) at 3 months to 84 (SD ± 13.39, range 50–100) at 6 months postoperatively to 98.56 (SD ± 13.06, range 55–100) at 1 year postoperatively. As per MEPS grading, postoperatively 3 months in 27 patients, 3.70% (n = 1) patients had excellent outcomes, 62.96% (n = 17) had good outcomes, 14.81% (n = 4) had fair outcomes, and 18.51% (n = 5) patients had poor outcomes. The MEPS grading postoperatively 6 months after surgery in 25 patients were as follows: 64% (n = 16) patients had excellent outcomes, 16% (n = 4) had good outcomes, 12% (n = 3) had fair outcomes, and 8% (n = 2) patients had poor outcomes. MEPS grading postoperatively 12 months in 25 patients showed that 80% (n = 20) patients had excellent outcomes, 16% (n = 4) had good outcomes, and 4% (n = 1) patients had poor outcomes. The final mean range of motion of operated upper limb was as follows: 28.5° of extension deficit (SD 9.07, range, 10°–40°), 117.5° of flexion (SD 13.18, range, 90°–130°), 70.9° of supination (SD 10.19, range, 40°–85°), and 65.5° of pronation (SD 9.54, range, 40°–80°). The final mean range of motion of the opposite normal upper limb was as follows: 6° of extension (SD 1.25, range 0–15), 136.54° of flexion (SD 4.80, range 125–145), 83.5° of supination (SD 10.19, range 75–90), and 78.62° of pronation (SD 9.54, range 70–85). The percentage deficit range of motion in the operated limb as compared to the normal upper limb was as follows: 7.4% deficit in extension, 16.2% flexion deficit, 17.77% deficit in supination, and 20% deficit in pronation. On radiological assessment, no elbow instability was seen in any elbow X-rays postoperatively assessed by a radiocapitellar line made by passing through the middle of the radius shaft which should pass through the capitellum on lateral elbow radiographs in any degree of elbow flexion. Out of 27 – 12 had complications, out of those 12 – three had elbow arthritis which is managed with symptomatic treatment with analgesics, they showed considerable relief of symptoms after 1 year, and two had heterotopic ossification for which supervised active elbow physiotherapy given along with tablet indomethacin, they attained a functional range of motion of the elbow, that is, 30–130° of elbow flexion at end of 1 year, three had radial nerve neuropraxia which recovered at end of 1 year, two patient’s had elbow stiffness and showed improved range of motion of elbow after 1-year follow-up and two patients suffering from ulnar nerve neuropathy which resolved on its own after 1-year follow-up. No other surgical intervention is required in any patient for any of the complications mentioned (Fig. 1-5).


The aim of this study is to find a step-wise protocol used in terrible triad elbow injuries which relies on biomechanical principles of the anatomy of the elbow and how it relates to post-operative stability. Terrible triad injuries of the elbow have historically been challenging injuries to treat and although initial treatment protocols were limited because of small sample sizes and high complication rates, recent studies have shown more predictable results [7-9]. A small type I or type II coronoid fragment is seen commonly with a TTI. It was once believed that the small type I coronoid fractures did not require fixation, but now even these small fragments are fixed because they provide important stability with their attachment to the anterior capsule [10-13]. In our study of 27 subjects, 16 subjects (59.25%) were of Regan–Morrey type 1 coronoid fracture, that is, coronoid process tip fracture. In our study, out of 27 cases, coronoid fixation was done in 21 patients. The basis for appropriate treatment of the terrible triad of the elbow is an appropriate restoration of the bone as well as ligamentous structures so as to provide the elbow with enough stability to start exercising early movements of the elbow [14-16]. In our study, equal importance is given to both bony (coronoid and radial head fractures) and ligamentous reconstruction (MCL and LCL) to provide good stability to the elbow. Repair of LCL complex (LCL) was performed in all cases in our study. MCL repair was required in 14 cases (51.85%) in view of instability persisting after the LCL repair. In unstable elbows associated with fractures of the coronoid, the stabilizing function of the radial head should be preserved whenever possible, either by means of reconstruction or through replacement by a prosthesis. Resection arthroplasty is not recommended in the terrible triad of elbow cases, because of the risk of instability and arthrosis [17,18]. Watters et al. [19] concluded that radial head arthroplasty afforded the ability to obtain elbow stability with comparable overall outcomes when compared to fixation. No resection of the radial head was performed in any patient in our study. Management of radial head fractures in the form of fixation or arthroplasty should be decided based on the communication of radial head fractures [20]. Functional results from this study show that an average flexion-extension arc of 90° and a supination-pronation arc of 136.4° can be achieved with no secondary operative procedure required in any case for stiffness and instability. Other published results similarly demonstrate an average flexion-extension arc of 100–119° and a supination-pronation arc of 128–141° [21, 22]. The supination-pronation arc in this study was comparable to other literature, but the mean flexion-extension arc achieved was less due to the late presentation of some cases after injury, non-compliance to physiotherapy protocols, and high incidence of post-operative complication rates seen in our study. Previous reports show that the most common complications with these injuries include stiffness, instability, heterotopic ossification, and ulnar neuropathy [23, 24]. In our study, a total of 12 patients (44.44%) suffered from complications. Three had elbow arthritis, two had heterotopic ossification, three had radial nerve neuropraxia, two patients had elbow stiffness for which extensive elbow physiotherapy and rehabilitation were done, and two patients suffered from ulnar nerve neuropathy. No reoperation was required to manage these complications. All these complications were tackled with regular follow-ups and supervised physiotherapy protocol. However, there were certain limitations to this study. First, it included only short-term follow-ups up to 1 year. We observed a high percentage of MCL repair compared to other studies that need to be studied on a larger number of cases. Second, a larger sample size and long-term follow-ups are necessary to establish the superiority of one modality over the other (Table 1).
To solve the TTI puzzle, every component of fracture and soft tissue injuries needs to be tackled in a sequential and step-wise manner to achieve good functional outcomes at the end of 1 year. Even after addressing each and every component of the injury, high complication rate persists attributed to the complexity of TTI which is manageable with dedicated post-operative elbow physiotherapy and rehabilitation.
Terrible trial injuries are complex and well-planned surgical treatment along with rehabilitation can provide satisfactory results. The soft-tissue component is often ignored, focusing on which can result in better stability and functional results.
References
- 1.Hotchkiss RN. Fractures and dislocations of the elbow. In: Rockwood and Green’s Fractures in Adults. Philadelphia, PA: Lippincott-Raven; 1996. p. 929-1024. [Google Scholar]
- 2.Hildebrand KA, Patterson SD, King GJ. Acute elbow dislocations: Simple and complex. Orthop Clin North Am 1999;30:63-79. [Google Scholar]
- 3.Chen HW, Liu GD, Ou S, Fei J, Zhao GS, Wu LJ, et al. Operative treatment of terrible triad of the elbow via posterolateral and anteromedial approaches. PLoS One 2015;10:e0124821. [Google Scholar]
- 4.Armstrong AD. The terrible triad injury of the elbow. Curr Opin Orthop 2005;16:267-70. [Google Scholar]
- 5.Miyazaki AN, Checchia CS, Fagotti L, Fregonez M, Santos PD, da Silva LA, et al. Evaluation of the results from surgical treatment of the terrible triad of the elbow. Rev Bras Ortop 2014;49:271-8. [Google Scholar]
- 6.Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Related Res 1987;216:109-19. [Google Scholar]
- 7.Forthman C, Henket M, Ring DC. Elbow dislocation with intra-articular fracture: The results of operative treatment without repair of the medial collateral ligament. J Hand Surg Am 2007;32:1200-9. [Google Scholar]
- 8.Leigh WB, Ball CM. Radial head reconstruction versus replacement in the treatment of terrible triad injuries of the elbow. J Shoulder Elbow Surg 2012;21:1336-41. [Google Scholar]
- 9.Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: Current concepts. J Am Acad Orthop Surg 2009;17:137-51. [Google Scholar]
- 10.Pugh DM, McKee MD. The “terrible triad” of the elbow. Tech Hand Up Extrem Surg 2002;6:21-9. [Google Scholar]
- 11.Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban EM, Larrainzar-Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop 2011;35:851-60. [Google Scholar]
- 12.Bohn K, Ipaktchi K, Livermore M, Cao J, Banegas R. Current treatment concepts for “terrible triad” injuries of the elbow. Orthopedics 2014;37:831-7. [Google Scholar]
- 13.Chan K, King GJ, Faber KJ. Treatment of complex elbow fracture-dislocations. Curr Rev Musculoskeletal Med 2016;9:185-9. [Google Scholar]
- 14.Chen NC, Ring D. Terrible triad injuries of the elbow. J Hand Surg Am 2015;40:2297-303. [Google Scholar]
- 15.McKee MD, Pugh DM, Wild LM, Schemitsch EH, King GJ. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical technique. J Bone Joint Surg Am 2005;87:22-32. [Google Scholar]
- 16.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am 2002;84:547-51. [Google Scholar]
- 17.Pugh DM, Wild LM, Schemitsch EH, King GJ, McKee MD. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am 2004;86:1122-30. [Google Scholar]
- 18.Gomide LC, de Oliveira Campos D, Ribeirode Sá JM, de Sousa MR, do Carmo TC, Andrada FB. Terrible triad of the elbow: Evaluation of surgical treatment. Rev Bras Ortop 2011;46:374-9. [Google Scholar]
- 19.Watters TS, Garrigues GE, Ring D, Ruch DS. Fixation versus replacement of radial head in terrible triad: Is there a difference in elbow stability and prognosis? Clin Orthop Relat Res 2014;472:2128-35. [Google Scholar]
- 20.Egol KA, Immerman I, Paksima N, Tejwani N, Koval KJ. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis 2007;65:263-70. [Google Scholar]
- 21.Lindenhovius AL, Jupiter JB, Ring D. Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg 2008;33:920-6. [Google Scholar]
- 22.Zeiders GJ, Patel MK. Management of unstable elbows following complex fracture-dislocations--the “terrible triad” injury. J Bone Joint Surg Am 2008;90:75-84. [Google Scholar]
- 23.O’Driscoll SW, Morrey BF, Korinek SA, An KN. Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop Relat Res 1992;280:186-97. [Google Scholar]
- 24.Ring D. Fractures of the coronoid process of the ulna. J Hand Surg 2006;31:1679-89. [Google Scholar]













