[box type=”bio”] What to Learn from this Article?[/box]
When a periprosthetic patellar fracture occurs without any trauma, it suggests that there’s a poor blood supply to the patella with a high risk of non-union, especially in case of a supplementary disruption of the vascular network around the patella caused by a re-intervention (ORIF).
Case Report | Volume 6 | Issue 2 | JOCR April-June 2016 | Page 89-91| Karim Masmoudi, Yamen Grissa, Sofien Benzarti, Hassen Cheikhrouhou, Zied Mensi DOI: 10.13107/jocr.2250-0685.452
Authors: Karim Masmoudi[1], Yamen Grissa[1], Sofien Benzarti[1], Hassen Cheikhrouhou[1], Zied Mensi[1]
[1] Department of Orthopedic Surgery, Sahloul University Hospital, Sousse, Tunisia.
Address of Correspondence
Dr. Masmoudi Karim,
Sahloul University Hospital, Hammam Sousse, 4011 Sousse, Tunisia.
E-mail: mkfms@yahoo.fr
Abstract
Introduction: Periprosthetic patellar fracture after total knee arthroplasty (TKA) is a rare complication. Their management can be very challenging with unpredictable results. Literature analysis showed few articles about this complication, but no publication has described the management of open patella fracture around total knee arthroplasty.
Case Presentation: We report a unique case of an open patellar fracture above a total knee arthroplasty, sustained by a 56-year-old female patient.
Conclusion: Despite the poor outcome of operative management in patellar periprosthetic fracture, this approach should be considered for acute and post traumatic fractures in young patients with a good remaining bone stock.
Keywords: Periprosthetic fracture, patellar fracture, open, total knee replacement.
Introduction
The demographic changes with a high rate of aging and active population, as well as the improved life expectancy during the last decades have led to an increase in the number of total knee arthroplasties (TKA) [1, 2, 3, 4], and consequently a raise of post-operative complications. Among these complications, periprosthetic fracture after TKA is the most frequent cause of post-operative pain, and revision surgery [5]. They may occur in the supracondylar region of the femur, followed by the patella, then the proximal tibia [1, 2, 3, 4, 5, 6, 7]. The rate of periprosthetic patellar fracture is ranging from 0.5 to 3% after TKA [8]. This entity can be very challenging to manage, with unpredictable and poor outcome, especially for displaced fracture or in cases with implant loosening [1, 2, 3, 4, 5, 8]. In this article, we report a unique case of an open periprosthetic patellar fracture that was managed with operative treatment. It also involves a literature analysis with description of the risk factors and treatment options of this uncommon entity.
Case Presentation
A 56-year-old female underwent a cemented postero-stabilized condylar TKA with fixed tibial plateau through an antero-medial approach, in our department. She had severe osteo-arthritis of the left knee with a major stiffness (irreducible flexum at 25°). (Fig. 1, 2) Initial (1) and post operative(2) Knee radiographs before, and after the arthroplasty.Three weeks later, the patient tripped and fell off with all her standing height striking the anterior aspect of the left knee with hyper flexion. She was taken to the emergency room with left knee pain and a large skin wound. Physical examination showed a large, deep and longitudinal wound measuring 15 cm in length due to a total breakdown of the suture line (the antero-medial approach performed during the TKA) (Fig. 3, 4).
Fig 3. A clinical picture showing the open patellar fracture
Fig 4. Lateral Knee radiograph showing the patellar fracture above a total knee arthroplasty, without any signs of implants loosening.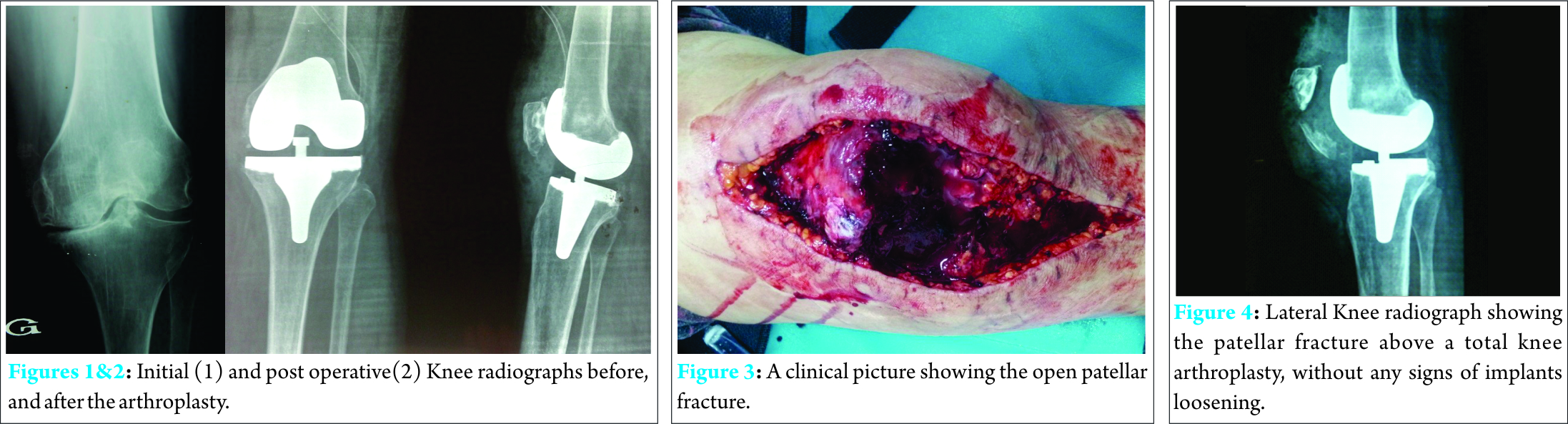
The knee radiographs showed a short oblique fracture at the inferior pole of the patella without any loosening of the implants or dislocation of the knee: this fracture is classified as type I according to Ortigueraet D.J. Berry classification [8][9] (a stable implant without disruption of the extensor mechanism).
The patient was transferred to the orthopaedic surgery department. She urgently received intravenous antibiotic (augmentin, gentamicin), as well as tetanus vaccination. Her fracture was temporarily stabilized in a long-leg plaster splint before she was transported to the operating room.
She underwent wound irrigation, debridement of non-viable soft tissue from the wound, open reduction and fixation with a figure-eight cerclage wiring, without any revision of the implants. The wound was closed without any skin tension, after placing an intra-articular drain. Complementary immobilization with a removable knee pad at full extension, for six weeks was prescribed.
Post-operative knee radiographs showed a satisfactory reduction of the patellar fracture.
(Fig. 5, 6). Post operative Knee radiographs
She received intra venous antibiotics: augmentin for 2 weeks associated with gentamicin during the first five days, as well as subcutaneous heparin. The drain was removed at the third post-operative day. Her wound was clean, dry, and without erythema. The patient was afebrile with a normal leukocyte count. She was discharged from the hospital after she was instructed to remain non-weight bearing with a follow-up in 2 weeks.
Results
At 6 months follow-up, physical examination did not reveal any signs of local or deep infection. Her knee was pain free and she was able to walk without crutches, but she had a mild stiffness: the knee range of motion was 0°/60°.
No antero-posterior or frontal laxities were noted.
(Fig. 7-9). Clinical pictures at last follow-up showing a clean and dry wound (7), and knee range of motion (8, 9)
The patient achieved union of the fracture: knee radiographs showed a healed patellar fracture, with hardware in place.
(Fig. 10). Lateral Knee radiograph at last follow-up.
Discussion
Since the late 1960s, total knee arthroplasty has been the most effective treatment for knee osteoarthritis, providing good functional outcomes and improvement in the patient’s quality of life [5].
Constant advances in the joint replacement surgery, and especially the total knee arthroplasties have led to an increase in the number of complications following this type of surgery, such as periprosthetic fractures. [1, 2, 3, 4]
This entity is very challenging to treat even for the most skilled and experienced surgeons [7, 8, 10]. The femur is the most frequent fracture site, followed by the patella and the tibia [1, 2, 3, 4, 5, 6, 7].
Patella fracture after TKA can occur after trauma, or result from a stress fracture due to patella osteonecrosis, which is the most common cause of this type of fracture [1, 2, 3, 4, 5, 8, 10, 11].
Chalidis et al (2007) have reported in a systematic review of a 752 periprosthetic patella fracture that in 88.3% of the cases, the fracture was not associated with a traumatic event, asymptomatic, and discovered during routine follow-up[5].
Many risk factors of these stress fractures have been described in the previous literature [1, 2, 3, 4, 5, 7, 8, 9, 10, 11] including:
Poor blood supply for patella after TKA especially for antero-medial approach, and in case of lateral release or unwarranted fat pad removal: knee replacement surgery is likely to cause disruption of the vascular peri-patellar network especially the medial and the superior lateral genicular arteries.
Mal-alignment of the femoral and tibial implants
Patella resurfacing arthroplasties
An excessive (thickness <15 mm) or asymmetric bone resection during patella resurfacing
Osteonecrosis due to bone cement polymerization : the heat of polymerization of the polymethylmethacrylate may exceed the coagulation temperature, causing thermal necrosis of the bone
The use of large central fixation peg designs for patellar implant, instead of small peripheral peg design.
Revision surgery
Osteoporosis and bone loss
Hyperflexion of the knee
Rhumatoïd arthritis
Open patellar fracture above a total knee arthroplasty is a very uncommon injury, and challenging to treat. To our knowledge, no publication in the literature has reported such lesion. Gulotta et al. reported a unique case of patellar fracture associated with open knee dislocation after a total knee arthroplasty. It was treated with open reduction and internal fixation of the patella with band tension wiring [10]. Greco et al, reported an open tibial shaft fracture below an ipsilateral TKA, managed with intramedullary nailing [12].
Some factors should be considered to succeed in the management of this type of fracture such as displacement of the fracture, function of the extensor mechanism, stability of the patellar implant, remaining bone stock [1, 2, 3, 4, 5, 8, 9, 10, 11, 13]. It includes immobilization by a brace locked in full extension or a cylinder cast in case of non-operative treatment; open reduction and internal fixation, implant revision in case of loosening, partial or total patellectomy, repair of the quadriceps tendon or patellar ligament in case of surgical treatment [4, 5, 7, 8].
The periprosthetic patellar fractures are usually managed by a non-operative treatment especially for type I and II, because of the high infectious risk of open reduction and internal fixation [13, 14], and consequently a high risk of arthroplasty failure.
Literature analysis showed that conservative or non-operative treatment was more successful for the management of non-displaced patella fracture with stable implant and an intact extension mechanism. Ortiguera and Berry reported good results in 37 out of 38 peri-prosthetic patellar fractures managed with conservative treatment [9]. Dennis reported a complication rate of 39% of operative treatment (in a series of thirty one patients who sustained a peri-prosthetic patellar fracture) [7]. Chalidis’s systematic review has shown that open reduction and internal fixation failed in 92% of the cases [5].
In this particular case, we were forced to opt for an internal fixation with a cerclage wiring after intensive wound irrigation, debridement and soft tissue repair.
Although no conclusion can be established from a single case report, we think that the successful result in our case can be explained by the relative young age of the patient (56 years old), the good bone stock, the acute and post-traumatic characteristics of the fracture, the early and adequate management necessary to avoid infectious complication.
The surgical management may reduce the ability of patella to heal because of the evacuation of peri-fractural hematoma as well as the supplementary disruption of the vascular network around the patella after a knee replacement surgery. Nevertheless, the high failure rate of the operative treatment in the patellar peri-prosthetic fracture can be explained by:
The high proportion of stress, atraumatic fracture (88%) due to osteonecrosis which suggests a poor remaining bone stock.
The stress fracture, unlike the acute and post traumatic ones, has a higher risk of non-union.
The poor outcome of partial or complete patellectomy, which is a type of operative treatment.
In our point of view, the post traumatic fractures in young patients are more likely to heal than stress fractures in the elderly.
Conclusion
Peri-prosthetic patella fracture is a very uncommon entity, and challenging to treat, especially the open ones, because of the high risk of infectious complications.
Although several previous studies report a high rate of failure and unpredictable results of open reduction for periprosthetic patellar fracture, this approach (especially the internal fixation with a strong and dynamic construct) should be considered in young patients with a good remaining bone stock, who sustained an open or a displaced fracture after a high energy trauma.
Clinical Message
Orthopaedic surgeons should consider open reduction and internal fixation as a good management alternative for periprosthetic patellar fracture, in case of a post traumatic and acute fracture in young patients with a good bone stock. Operative treatment can lead to satisfactory outcome with an adequate selection of patients.
References
1. Sarmah SS, Patel S, Reading G, El-Husseiny M, Douglas S, Haddad FS. Periprosthetic fractures around total knee arthroplasty. Ann R Coll Surg Engl. 2012; 94:302-07. [PMID:22943223].
2. Jae Doo Yoo and Nam Ki Kim.Periprosthetic Fractures Following Total Knee Arthroplasty. Knee Surg Relat Res 2015;27(1):1-9.[PMID:25750888].
3. Gordon M C, Khan W and Johnstone D. Recent Advances and Developments in Knee Surgery: Principles of Periprosthetic Knee Fracture Management. The Open Orthopaedics Journal. 2012;6(2):301-304.
4. MÄRDIAN S, WICHLAS F, SCHASER K-D, MATZIOLIS G, FÜCHTMEIER B, PERKA C., SCHWABEP. Periprosthetic Fractures around the Knee: Update on Therapeutic Algorithms for Internal Fixation and Revision Arthroplasty. ACTA CHIRURGIAE ORTHOPAEDICAE ET TRAUMATOLOGIAE ČECHOSL. 2012;79:297-306.
5. Chalidis B E, Tsiridis E, Tragas A Aa, Stavrou Z, Giannoudis P V. Management of periprosthetic patellar fractures; A systematic review of literature. Injury, Int. J. Care Injured. 2007;38:714—724.[PMID: 17477924].
6. Agarwal S, Sharma R K, Jain J. Periprosthetic fractures after total knee arthroplasty. Journal of Orthopaedic Surgery. 2014; 22(1):24-9.[PMID: 24781608].
7. Dennis D A. Periprosthetic Fractures Following Total Knee Arthroplasty. American Academy of Orthopaedic Surgeons : J Bone and Joint Surg. 2001; 83(A):120-130.
8. Sheth NP, Pedowitz DI, Lonner JH. Periprosthetic patellar fractures. J Bone Joint Surg Am . 2007, Vols. 89 : 2285-96.[PMID: 17908909]
9. Ortiguera C J, Berry D J. Patellar Fracture After Total Knee Arthroplasty. J Bone and Joint Surg. 2002; 84(A).
10. Gulotta L V et al. Periprosthetic Patellar Fracture after an Open Knee Dislocation. Clinical Orthopaedics And Related Research. 2005; 436: 265–269.[PMID: 15995451].
11. Chun K A, Ohashi K, Bennett D L, El-Khoury G Y. Patellar Fractures After Total Knee Replacement. AJR 2005; 185:655–660.[PMID: 16120913].
12. Greco N, Goyal K, and Tarkin I. Intragrade Intramedullary Nailing of an Open Tibial Shaft Fracture in a Patient With Concomitant Ipsilateral Total Knee Arthroplasty. The American Journal of Orthopedics 2015;81-86.[PMID: 25750957].
13. Keating EM, Haas G, Meding JB. Patella fracture after post total knee replacements. Clin Orthop Relat Res. 2003;416:93-7.[PMID: 14646745].
14. Trousdale R T. Infection after an open supracondylar fracture above a total knee arthroplasty treated with the supracondylar nail. Am J Orthop (Belle Mead NJ) 1995;24(8):625-9.[PMID: 17982818].
| How to Cite This Article: Masmoudi K, Grissa Y, Benzarti S, Cheikhrouhou H, Mensi Z. Open Periprosthetic Patellar Fracture after Total Knee Replacement. Journal of Orthopaedic Case Reports 2016 April – June;6(2): 89-91. Available from: https://www.jocr.co.in/wp/2016/04/01/2250-0685-452-fulltext/ |
[Full Text HTML] [Full Text PDF] [XML]
[rate_this_page]
Dear Reader, We are very excited about New Features in JOCR. Please do let us know what you think by Clicking on the Sliding “Feedback Form” button on the <<< left of the page or sending a mail to us at editor.jocr@gmail.com