It may be useful to attach bridging external fixation to prevent a collapse of the lunate with osteoid osteoma.
Dr. Kiyohito Naito, Department of Orthopaedics, Faculty of Medicine, Juntendo University, 2-1-1 Hongo, Bunkyo-ku, Tokyo 113-8421, Japan. E-mail: knaito@juntendo.ac.jp
Introduction: We report a patient with osteoid osteoma that developed in the lunate.
Case Report: The patient was a healthy 28-year-old male who had the right wrist joint pain and osteosclerosis of the lunate was noted on plain radiography. Kienböck’s disease was considered at the first examination, but a nidus was observed on computed tomography, suggesting osteoid osteoma in the lunate. The resection of the bone lesion and bridging external fixation to prevent post-operative collapse of the lunate was performed. Histopathological diagnosis was also osteoid osteoma in the lunate. At 3 years after surgery, no recurrence of the lesion or progression of collapse of the lunate has occurred.
Conclusion: As the development of osteoid osteoma in the lunate is a markedly rare pathology and there are many differential diseases, the time to diagnosis may be prolonged. Moreover, it may be useful to attach bridging external fixation to prevent a collapse of the lunate.
Keywords: Osteoid osteoma, lunate, nidus, Kienböck disease, bridging external fixation.
Osteoid osteoma is an osteogenic benign bone tumor that accounts for approximately 14% of all cases of bone tumors [1]. Normally, the nidus is visualized as a 1-cm or smaller round to oval lesion with a clear boundary on plain radiography and computed tomography (CT), and reactive bone formation accompanies the lesion in many cases [1]. This tumor frequently develops in 10–20-year-old males and its development after 40 years old is rare [1]. The frequent development site is the diaphysis of long bones in the lower limbs such as the femur and tibia [2]. The rate of osteoid osteoma developing in the carpal bones is 0.14%, being rare, and the development in the lunate has been reported to be markedly rare [3]. We report a patient with osteoid osteoma that developed in the lunate. The lunate is a carpal bone receiving axial pressure loads of the wrist joint and collapse of the lunate may occur after resection of the lesion. In this patient, in addition to pain relief of osteoid osteoma, surgical treatment to prevent postoperative collapse of the lunate was performed.
The patient was a healthy 28-year-old male, right-handed and a cook. The swelling and pain of the right wrist joint were appeared from more than 1 year and 6 months before visiting our hospital. The wrist joint pain was increased when the wrist joint was extended. The range of motion of the right wrist joint was as follows: Flexion, 5°; extension, 10°; forearm pronation, 80°; and forearm supination, 80°. The grip strength was 6 kg (relative to the healthy side: 13%), the visual analog scale (VAS) score was 4/10, the quick disabilities of the arm, shoulder, and hand (Q-DASH) score was 38.64/100, and the Mayo wrist score was 60/100. On plain radiography, a radiolucent zone was noted in the lunate in the frontal view and osteosclerosis was present (Fig. 1a). In the lateral view, osteoarthritic (OA) changes were noted on the radiocarpal joint surface (Fig. 1b). Magnetic resonance imaging (MRI) was performed under the initial suspicion of Kienböck’s disease. On MRI short tau inversion recovery imaging, the lunate demonstrated low intensity, whereas the scaphoid, pisiform, and distal radius exhibited high intensity (Fig. 1c). The MRI findings were similar to those of wrist arthritis and were not typical of Kienböck’s disease. Therefore, in addition to Kienböck’s disease, collagen diseases, such as rheumatoid arthritis, tuberculosis, atypical mycobacterial disease, and bacterial infection-induced arthritis, were included as differential diseases, and blood testing and CT were performed. On blood testing, all inflammatory markers, such as the white blood cell count, C-reactive protein, erythrocyte sedimentation rate, and procalcitonin were negative. Mycobacterium tuberculosis INF-γ measurement and anti-mycobacterium antibody titer were also negative. All autoantibodies were also negative. Therefore, infection and collagen disease were excluded from the study. On CT, a low-density area was present in a region in the lunate contacting the radiocarpal joint surface, which accompanied osteosclerosis (Fig. 1d). Based on these findings, osteoid osteoma accompanied by a nidus was considered and treatment was initiated.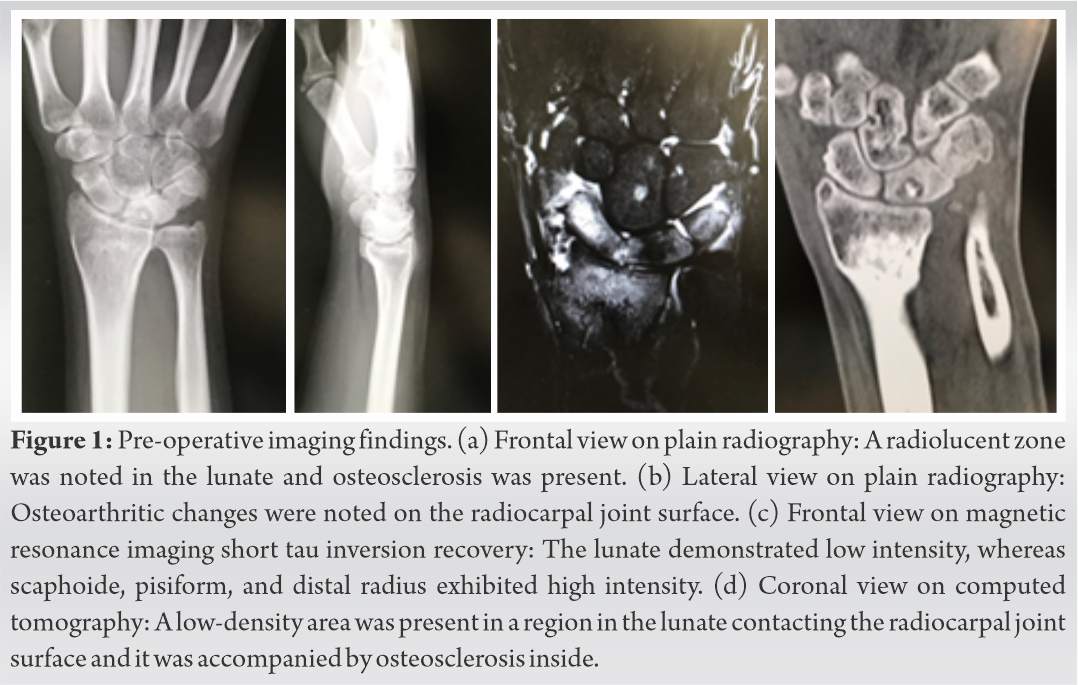
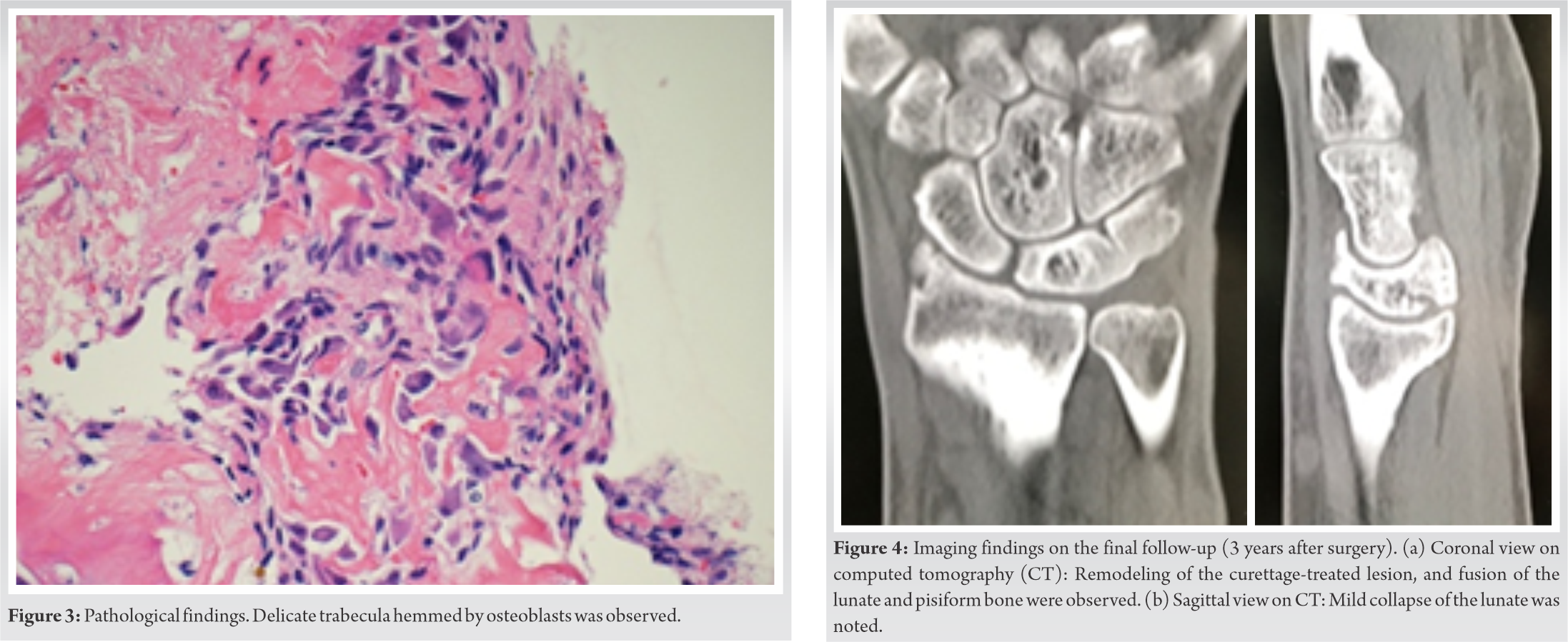
Conservative treatment with immobilization aiming at rest of the wrist joint and oral non-steroidal anti-inflammatory drugs (NSAIDs) was performed. NSAIDs temporarily relieved pain in especially at night. Moreover, inconvenience in daily life continued due to the restriction of the range of motion of the wrist joint. Thus, surgical treatment was selected. As the lesion expanded close to the radiocarpal joint, arthroscopic observation of the lunate joint surface, and resection of the bone lesion and bridging external fixation were performed aiming at reducing the load of wrist joint axial pressure on degenerated cartilage. Surgical treatment was done by the experienced specialist (YS). First, 3–4 and 4–5 portals were prepared and the radiocarpal joint was observed by wrist arthroscopy. The synovitis was occurred in the radiocarpal joint, especially between the navicular bone and lunate, and the synovial membrane was resected. The joint cartilage of the lunate right below the lesion was softened (Fig. 2a). Then, the wrist joint was exposed through the dorsal approach and the lunate lesion was resected from the dorsal side (Fig. 2b and c). As a bone defect was produced due to curettage of the lesion, to prevent a collapse of the lunate, bridging external fixation was attached for 4 weeks after surgery (Fig. 2d). Several small tissue fragments were submitted for pathological examination. Histologically, a delicate trabecula partially hemmed by osteoblasts was observed (Fig. 3). Based on the above pathological findings, the bone lesion was diagnosed with osteoid osteoma developed in the lunate. The pain on the wrist joint was reduced 1 week after surgery. The range of motion of the right wrist at 4 weeks after surgery (after removal of external fixation) was as follows: Flexion, 15°; extension, 20°; forearm pronation, 85°; and forearm supination, 85°; the grip strength was 18 kg (relative to the healthy side: 45%), VAS score was 1/10, Q-DASH was 9.09/100, and the Mayo wrist score was 70/100. The patient was able to return to his work 4 months after surgery at a level similar to that before surgery without pain during work. At the final follow-up (3 years after surgery), the range of motion of the right wrist joint was as follows: Flexion, 40°; extension, 50°; forearm pronation, 85°; and forearm supination, 85°; the grip strength was 31 kg (relative to the healthy side: 70%), VAS score was 0/10, Q-DASH was 0/100, and the Mayo wrist score was 90/100. No recurrence has been noted on CT, but remodeling of the lesion treated by curettage, mild lunate collapse, and fusion of the lunate and pisiform bone was noted (Fig. 4a, b). At the final observation, the patient had no inconvenience in work and had the same daily life as before the development of symptoms.
 />
/>
Osteoid osteoma was initially reported in 1935 as an osteogenic benign bone tumor [4]. The main symptoms of osteoid osteoma developing in the carpal bones are swelling and pain of the wrist joint. Pain increases at night in many cases and is relieved by NSAIDs, being characteristic [5]. In general, it is diagnosed based on the presence of diffuse osteosclerosis and a nidus consistent with its center on plain radiography [3]. However, some cases of osteoid osteoma developing in the carpal bones are overlooked on plain radiography alone and the usefulness of CT for diagnosis has been reported [3]. On the other hand, edema is noted in the bone marrow and soft tissue around the lesion on MRI, and these are similar to findings of infection and malignant disease. Thus, MRI is inferior to CT as a diagnostic tool for this disease [2]. In the past studies, a long time was spent diagnosing osteoid osteoma that developed in the lunate due to the difficulty in differentiating Kienböck’s disease, OA changes of the lunate, collagen disease, such as rheumatoid arthritis, tuberculosis, atypical mycobacterial disease, and bacterial infection-induced arthritis [1,2,3]. In the present patient, diagnosis and treatment were proceeded considering Kienböck’s disease from the first examination, because, first, the main symptoms of the two pathologies are similar. The patient visited our hospital for swelling and pain of the wrist joint. Many Kienböck’s disease patients also visit hospitals for similar complaints. Second, osteosclerosis was noted in the lunate on plain radiography without bone collapse. Arnaiz et al. reported that osteosclerosis is present in the lunate on plain radiography in Lichtmann classification stage II Kienböck’s disease [6]. The plain radiography findings of our patient were similar to those of Kienböck’s disease. In addition, there is a large deviation in the prevalence between Kienböck’s disease and osteoid osteoma developing in the lunate. According to one report, the prevalence of Kienböck’s disease is 1.9% [7], whereas that of osteoid osteoma developing in motor organs accounts for approximately 12% of cases of benign tumors developing in motor organs. Of the 12%, osteoid osteoma developing in the hand and carpal bones was reported to account for 8 and 0.14%, respectively [3]. According to the past case reports of osteoid osteoma that developed in the lunate, development in the lunate is rare; thus, no doubt may be left for practitioners in routine medical practice, that is, the frequency of encountering Kienböck’s disease is high in general medical practice, and the symptoms and imaging findings are similar, Kienböck’s disease was considered, delaying the diagnosis in this patient. This refection point is a task of routine medical practice that orthopedists should be aware of in the future.
Normally, surgical treatment for osteoid osteoma is nidus resection [3]. When nidus resection is incomplete, there is a risk of residual pain and recurrence; therefore, complete nidus resection is the goal to be achieved in surgical treatment [3]. The lunate is a carpal bone receiving axial pressure loads and the force transmitting to the lunate increases when the wrist joint extends [8]. When the lunate is collapsed, OA changes in the radiocarpal joint and midcarpal joint occur [6]. Therefore, complete resection of a nidus that developed in the lunate may be a risk factor for the collapse of the lunate. Thus, we decided to concomitantly apply bridging external fixation (Fig. 2d). As bridging external fixation adds traction of the wrist joint in the long axis direction, it prevents collapse of the lunate. In addition, traction is expected to promote revascularization in the lunate, aiding in the maintenance of the shape of the lunate [9]. Gabl et al. reported that they concomitantly applied bridging external fixation in addition to vascularized bone graft in a clinical case of Kienböck’s disease, and it was useful to prevent collapse of the lunate [10]. In the past case reports of osteoid osteoma that developed in the lunate, concomitant non-vascularized bone grafting from the radius and ilium to the bone defect in the lunate produced after nidus resection was performed to prevent postoperative collapse of the lunate [1,3]. Saidi et al. reported that large bone defects require filling with autologous bone [3], whereas Cheah and Fields reported that autologous bone grafting is not necessary for 6-mm bone defects [2], demonstrating that the viewpoints on the necessity of autologous bone graft or the bone defect range requiring autologous bone graft have not yet been unified. In the present patient, a 6-mm bone defect was produced in the lunate after nidus resection and treated by traction using bridging external fixation, but bone grafting was not performed to prevent collapse of the lunate and remodeling. Bridging external fixation was attached for 4 weeks and range of motion training of the wrist joint was started after removal of the bridging external fixation. As of 3 years after surgery, no recurrence of the lesion or progression of collapse of the lunate has occurred, and the VAS score was 0/10, Q-DASH was 0/100, and the Mayo wrist score was 90/100, achieving a favorable clinical outcome.
We treated a patient with osteoid osteoma that developed in the lunate causing chronic pain of the wrist joint. As the development of osteoid osteoma in the lunate is a markedly rare pathology and there are many differential diseases, the time to diagnosis may be prolonged. The main treatment for osteoid osteoma that developed in the lunate is resection of the lesion, but it has a risk for collapse of the lunate by axial pressure loads of the wrist joint. In this patient, collapse of the lunate was prevented by concomitant bridging external fixation.
As the development of osteoid osteoma in the lunate is a markedly rare pathology and there are many differential diseases, the time to diagnosis may be prolonged. Moreover, it may be useful to attach bridging external fixation to prevent a collapse of the lunate.
References
- 1.Breitenfeldt N, Liodaki ME, Mailänder P, Stang F. An unusual presentation of an osteoid osteoma in the lunate bone. Plast Reconstr Surg Glob Open 2017;5:e1410. [Google Scholar | PubMed]
- 2.Cheah JT, Fields TR. Persistent wrist monarthritis: Down to the bone. BMJ Case Rep 2018;2018:bcr2017222939. [Google Scholar | PubMed]
- 3.Saidi H, El Bouanani A, Ayach A, Fikry T. Osteoid osteoma of the lunate: Case report. Chir Main 2007;26:173-5. [Google Scholar | PubMed]
- 4.Jaffe HL. Osteoid osteoma: A benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg 1935;31:709-28. [Google Scholar | PubMed]
- 5.Aynaci O, Turgutoglu O, Kerimoglu S, Aydin H, Cobanoglu U. Osteoid osteoma with a multicentric nidus: A case report and review of the literature. Arch Orthop Trauma Surg 2007;127:863-6. [Google Scholar | PubMed]
- 6.Arnaiz J, Piedra T, Cerezal L, Ward J, Thompson A, Vidal JA, et al. Imaging of Kienböck disease. AJR Am J Roentgenol 2014;203:131-9. [Google Scholar | PubMed]
- 7.Mennen U, Sithebe H. The incidence of asymptomatic Kienböck's disease. J Hand Surg Eur Vol 2009;34:348-50. [Google Scholar | PubMed]
- 8.Genda E, Horii E. Theoretical stress analysis in wrist joint-neutral position and functional position. J Hand Surg Br 2000;25:292-5. [Google Scholar | PubMed]
- 9.Büchler U. The small AO external fixator in hand surgery. Injury 1994;25 Suppl 4:S-D55-63. [Google Scholar | PubMed]
- 10.Gabl M, Lutz M, Reinhart C, Zimmerman R, Pechlaner S, Hussl H, et al. Stage 3 Kienböck's disease: Reconstruction of the fractured lunate using a free vascularized iliac bone graft and external fixation. J Hand Surg Br 2002;27:369-73. [Google Scholar | PubMed]










