We report a mallet finger of non-traumatic origin secondary to a villonodular synovitis which was only suspected intraoperatively and which required surgical treatment with a good prognosis despite the uncertainty of the management of this pathology.
Dr. Otman Benabdallah, Department of Orthopaedics and Traumatology, Centres Hospitaliers de Tanger, Tangier, Morocco. E-mail: otman.benabdallah@homail.com
Introduction: Mallet finger is a frequent lesion. It represents 2% of sports emergencies and is the most common closed tendon injury seen in contact sports or in work environment. It occurs always after a traumatic etiology. Our case is atypical and exceptional, because it is caused by a villonodular synovitis, condition which has been never reported in the literature.
Case Report: A 35-year-old woman presented for a mallet finger deformity of the second right finger. When questioned, the patient did not recall any trauma; she reported that the deformation had developed gradually over a period of more than 20 days preceding the definitive deformation of the finger into a classic mallet finger. She reported experiencing mild pain before the deformation, with burning sensations at the third finger phalanx. On palpation, we noted the presence of nodules at the level of the distal interphalangeal joint and on the dorsal face of the second phalanx of the concerned finger. The X-ray examination showed the classic mallet finger deformity, with no bone associated lesion. The diagnosis of pigmented villonodular synovitis (PVNS) was suspected intraoperatively by the presence of hemosiderin into the tendon sheath and distal articulation. The excision of the mass with tenosynovectomy and reinsertion of the tendon was the essential elements of the treatment.
Conclusion: A mallet finger caused by a villonodular tumor is an exceptional condition with local aggressivity and uncertain prognosis. A meticulous surgical procedure could achieve an excellent result. Complete tenosynovectomy, tumor surgical resection, and tendon reinsertion were the mainstay of treatment for a long-lasting excellent result.
Keywords: Non-traumatic mallet finger, villonodular tumor of extensor tendon sheat, pigmented villonodular tenosynovitis, extensor tendon injury, finger deformity.
Mallet finger is a frequent lesion which most commonly affects long fingers, especially those on the ulnar edge of the hand. This lesion was described by Segond in 1880 [1]. It represents 2% of sports emergencies [2]and is the most common closed tendon injury seen in contact sports [2,3,4,5], with a predominance of male patients, and with the dominant hand more frequently affected (60%) [3]. It is considered to be chronic when the lesion is over than 3 weeks old. It can be also the result of a minor trauma or occurs in work environment [4,5,6,7]. The usual cause of mallet finger is a violent flexion or laceration of the dorsum of the finger at the distal interphalangeal joint (DIPJ) [5,6,7].
Otherwise, according to the literature [8], the joint most affected by villonodular synovitis is the knee (representing 63–75% of cases). Next are the hips and ankles, which represent the majority of the remaining cases. Exceptionally, damage to the temporomandibular joints, spine, sternoclavicular joints, or fingers have been reported. Villonodular synovitis of the tendon sheath, or tenosynovial giant cell tumor, is benign lesions arising from the tendon sheath, joint synovium, or bursae.
Our case was atypical and exceptional because this case of mallet finger was caused by a villonodular synovitis involving the distal joint (DIPJ) of the right hand second finger, which eroded the tendon insertion until it ruptured. When questioned about the origin of the condition, the patient did not recall any causative trauma; she reported that the deformation had developed gradually over a period of more than 20 days preceding the latest aspect finger deformation into a classic mallet finger. The diagnosis was not suspected before surgery, it was incidentally suggested intraoperatively, and of course confirmed by histology. Tenosynovectomy, surgical resection of the articular mass, and tendon reinsertion were the essential treatment [9,10,11,12,13,14]. The prognosis [4,5,10,12,13,14,15] of the treatment was uncertain, but a meticulous surgical procedure achieved an excellent result. Our patient had no recurrence at a recent follow-up of 8 years. Symptoms were completely relieved after surgery. Based on the Crawford classification [16], the result could be classified as good, or even excellent and exceptional with no pain and full range of motion; only a minor flexum of <10° persisted. To the best of our knowledge, there is no prior study in the literature reporting a case of mallet finger caused by villonodular synovitis.
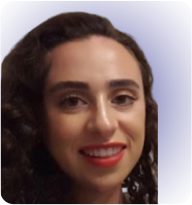
A 35-year-old woman presented for a mallet finger deformity of the second right finger. When questioned, the patient did not recall any trauma; she reported that the deformation had developed gradually over a period of more than 20 days preceding the definitive deformation of the finger in to a classic mallet finger. She reported experiencing mild pain before the deformation, with burning sensations at the third finger phalanx. On palpation, we noted the presence of nodules at the level of the DIPJ and on the dorsal face of the second phalanx of the concerned finger. The X-ray examination showed the classic mallet finger deformity, with no bone associated lesion. The diagnosis of pigmented villonodular synovitis (PVNS) was suspected intraoperatively by the presence of hemosiderin into the tendon sheath and distal articulation. The excision of the mass with tenosynovectomy and reinsertion of the tendon was the essential elements of the treatment.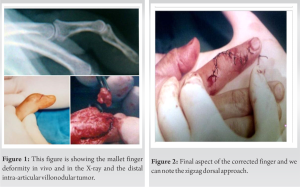
Treatment-management: The patient (Fig. 1) was operated under locoregional anesthesia. We performed a zigzag dorsal incision of the middle and distal phalanges (P1 and P2) of the Index finger (Fig. 2). After exposure of the tendon, we immediately noticed the bone desinsertion of the tendon, the presence of an intra-articular tumor of the DIPJ; the entire sheath of the tendon was affected (Fig. 3). 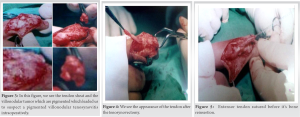 From the appearance of the tumor, villonodular tenosynovitis was suspected. The tumor was excised in block, the sheath of the entire tendon was resected, and all the affected areas were thoroughly cleaned (Figs. 4 and 5).
From the appearance of the tumor, villonodular tenosynovitis was suspected. The tumor was excised in block, the sheath of the entire tendon was resected, and all the affected areas were thoroughly cleaned (Figs. 4 and 5).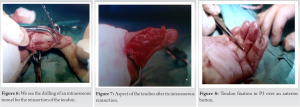 We, then, proceeded to the transosseous reinsertion of the tendon on P3 (Figs. 6 and 7) which was fixed over a button onto the palmar face of the distal (P3) finger (Fig. 8) for 8 weeks and immobilized with a finger splint.
We, then, proceeded to the transosseous reinsertion of the tendon on P3 (Figs. 6 and 7) which was fixed over a button onto the palmar face of the distal (P3) finger (Fig. 8) for 8 weeks and immobilized with a finger splint.
Mallet fingers are common injuries and involve disruption of the terminal extensor mechanism overlying the DIPJ. Usually, mallet finger injuries occur in the work environment or during sports. Our case is exceptional because the etiology of the extensor tendon lesion is a villonodular tenosynovitis. Our case is atypical in several respects: this mallet finger was spontaneous, it did not have any traumatic origin; the deformity occurred gradually; the mallet finger was chronic, and neglected by the patient. The cause was a villonodular tenosynovitis with intra-articular and extra-articular involvement and with the dorsal and palmar tendon sides damage [17,18]. In our case, the mechanism is totally different (no traumatic incident); the tendon was disrupted by a villonodular tumor in the distal joint (DIPJ), in which condition is known by its aggressivity [8,11,12,13,17,19,20]; the tumor has eroded the bone insertion of the tendon until it ruptured. The diagnosis was not suspected beforehand but was suggested incidentally intraoperatively and of course confirmed by histology. Macroscopically, the examination involved a mass of firm consistency, brownish, and rust colored. Histologically, it is characterized by medium-sized round cells with regular nuclei and associated with multinucleated giant cells and several siderophages. These cells are arranged in several layers and nodules separated from each other by a dense fibrous tissue. No signs of malignancy were found. Our case has similar anatomopathological characteristics described in the literature: Localized nodular tenosynovitis or diffuse PVNS involves an active proliferation of histiocyte-like cells (foamy macrophages and hemosiderin-laden cells) and multinucleated giant cells. PVNS lesions are more hypercellular and have fewer multinucleated giant cells [15,18,19]. In our case, the entire extensor tendon was affected intra-articularly and extra-articularly which can be classified as a diffuse type pigmented villonodular synovitis (PVNS). Usually, the lesion occurs along the volar aspect of the fingers, but dorsal involvement is not uncommon. In our case, in addition to the involved joint, the dorsal tendon side was more affected than the volar side. Until now, the etiology of villonodular synovitis is unknown. Several theories have been proposed to explain the pathogenesis including trauma, vascular disturbances, inflammation, and others. Probably, the most accepted theory is that of reactive or regenerative hyperplasia associated with inflammatory process as proposed by Jaffe et al. [19]. The treatment was laborious involving a tenosynovectomy with complete surgical excision of the articular mass and cleaning of both faces of the tendon before its reinsertion into the bone. Although villonodular tenosynovitis is benign, they have a substantial risk of recurrence (incidence 8–44%) [8,11,12,15,17]. The most common cause of recurrence is an incomplete excision. Our patient had no recurrence at a recent follow-up of 8 years. Hopefully, symptoms were completely relieved after surgery. A distal joint dysfunction can result from a missed diagnosis or inappropriate treatment. According to Schweitzer et al. [6] lengthening of the terminal extensor tendon by 1 mm results in 25° of extension lag, by 2 mm it results in 36° of extension lag and by 3 mm it results in 49° of extension lag, so this adaptative hyperextension which occurs can lead to a more or less marked swan neck deformity. Based on Crawford classification [16], the result was good and even excellent with no pain and full range of motion; a minor deformity of <10° persisted (Figs. 9, 10, 11). A review of literature in Google Scholar and a PubMed search was carried out but did not yield any reported case of mallet finger caused by a nodular tenosynovitis. We believe that this is the first instance of this exceptional case to be reported on.
A mallet finger caused by a villonodular tumor is an exceptional condition with local aggressivity and uncertain prognosis. A meticulous surgical procedure could achieve an excellent result. Complete tenosynovectomy, tumor surgical resection, and tendon reinsertion were the mainstay of treatment for a long-lasting excellent result.
The mallet finger that we report is an atypical case; it is not of traumatic origin but secondary to villonodular tenosynovitis. Our case was diagnosed intraoperatively and histologically, not by antelation. It should therefore be remembered that:
• The mallet finger may have a non-traumatic etiology secondary to a villonodular tumor or chronic inflammation or infection
• The diagnosis must be based on a good history, a good examination looking for non-classical signs (such as multiple nodules or a generous intra-articular tumefaction), a biological and radiological assessment, eventually a Magnetic Resonance Imaging.
References
- 1.Moss JG, Steingold RF. The long term results of mallet finger injury. A retrospective study of one hundred cases. Hand 1983;15:151-4. [Google Scholar | PubMed]
- 2.Simpson D, McQueen MM, Kumar P. Mallet deformity in sport. J Hand Surg Br 2001;26:32-3. [Google Scholar | PubMed]
- 3.Stern PJ, Kastrup JJ. Complications and prognosis of treatment of mallet finger. J Hand Surg Am 1988;13:329-34. [Google Scholar | PubMed]
- 4.Yee J, Waseem M. Mallet finger injuries. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar | PubMed]
- 5.Lamaris GA, Matthew MK. The diagnosis and management of mallet finger injuries. Hand (N Y) 2017;12:223-8. [Google Scholar | PubMed]
- 6.Schweitzer TP, Rayan GM. The terminal tendon of the digital extensor mechanism: Part II, kinematic study. J Hand Surg Am 2004;29:903-8. [Google Scholar | PubMed]
- 7.Alla SR, Deal ND, Dempsey IJ. Current concepts: Mallet finger. Hand (N Y) 2014;9:138-44. [Google Scholar | PubMed]
- 8.Court S, Nissen MJ, Gabay C. La synovite villonodulaire. Rev Med Suisse 2014;10:609-15. [Google Scholar | PubMed]
- 9.Jabłecki J, Syrko M. Zone 1 extensor tendon lesions: Current treatment methods and a review of literature. Ortop Traumatol Rehabil 2007;9:52-62. [Google Scholar | PubMed]
- 10.Valdes K, Naughton N, Algar L. ICF components of outcome measures for mallet finger: A systematic review. J Hand Ther 2016;29:388-95. [Google Scholar | PubMed]
- 11.Mane SA, Bansode AS, Karande CS, Wahegaonkar AL. Arthroscopic excision of localized nodular tenosynovitis of carpometacarpal joint of thumb: A case report and review of literature. J Wrist Surg 2021;9:533-5. [Google Scholar | PubMed]
- 12.Lv Z, Liu J. Giant cell tumor of tendon sheath at the hand: A case report and literature review. Ann Med Surg (Lond) 2020;9:143-6. [Google Scholar | PubMed]
- 13.Kerfant N, Bardin T, Roulot E. Multiple giant cell tumors of the tendon sheath: Separate volar and dorsal lesions involving three digits of the same hand following repetitive trauma. J Hand Microsurg 2015;7:233-5. [Google Scholar | PubMed]
- 14.Garberman SF, Diao E, Peimer CA. Mallet finger: Results of early versus delayed closed treatment. J Hand Surg Am 1994;19:850-2. [Google Scholar | PubMed]
- 15.Moore JR, Weiland AJ, Curtis RM. Localized nodular tenosynovitis: Experience with 115 cases. J Hand Surg Am 1984;3:412-7. [Google Scholar | PubMed]
- 16.Crawford GP. The molded polythene splint for mallet finger deformities. J Hand Surg Am 1984;9:231-7. [Google Scholar | PubMed]
- 17.Kotwal P, Gupta V, Malhotra R. Giant-cell tumor of the tendon sheath: Is radiotherapy indicated to prevent recurrence after surgery? J Bone Joint Surg 2000;82:571-3. [Google Scholar | PubMed]
- 18.Reilly KE, Stern PJ, Dale JA. Recurrent giant cell tumors of the tendon sheat. J Hand Surg Am 1999;24:1298-302. [Google Scholar | PubMed]
- 19.Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis, and tenosynovitis. Arch Pathol 1941;31:731-65. [Google Scholar | PubMed]
- 20.Karasick D, Karasick S. Giant cell tumor of tendon sheath: Spectrum of radiologic findings. Skeletal Radiol 1992;4:219-24. [Google Scholar | PubMed]