Combined posterior convergent elbow dislocation is a very rare scenario, as this is third reported case from world literature and first case from India in adult patients. High index of suspicion required to identify the case in post elbow reduction X-ray to avoid further complications.
Dr. Akash Nagnath Mane, Department of Orthopedic Surgery, Deenanath Mangeshkar Hospital and Research Center, Pune, Maharashtra, India. E-mail: dr.akashmane54@gmail.com
Introduction: Elbow dislocations are commonly encountered by orthopedic surgeons all over. Management is straightforward and the result is generally satisfactory. However, in a small subset, associated injuries like convergent or divergent dislocations at superior radioulnar joints are present. These associated injuries are often missed initially leading to their delayed treatment and suboptimal elbow function. We report one such rare case of Convergent dislocation at the elbow. Although reported from other parts of the world till date, there has been none reported from India. It is extremely rare in adults. Twenty-three cases in children and only two in adults stand reported so far in world literature. Thus, our reporting it could be the first report of convergent dislocation at the elbow from India. To the best of our knowledge, it is only the third reported adult case in world literature.
Case Report: We describe a 68-year-old male visiting a local hospital with a history of fall from a two-wheeler. An initial radiograph revealed an obvious posterior dislocation of the elbow. Closed reduction was performed, and posterior above elbow slab was given. Patient presented to us 10 days later with persistent pain. Evaluation with radiographs confirmed reduction of ulno-humeral joint but translocation of the radius and ulna which is combined posterior and convergent elbow dislocation.
Conclusion: Combined posterior and convergent elbow dislocation is a rare scenario. The rarity of these associated injuries is the reason for lack of awareness. We suggest careful scrutiny of pre-reduction anteroposterior radiographic view or 3D CT in suspected cases as well as X-ray/Carm anteroposterior view in extended position of elbow on the operation table immediately after reduction before slab application in every case of elbow dislocation. Significant difficulty was encountered in open reduction in our case. This could be attributed to buttonholing of the radial head through insertion of brachialis fibers. The reporting of this surgical difficulty is important because it will help the surgeon know it beforehand and the awareness would make the surgeon take appropriate measures well in time.
Keywords: Convergent elbow dislocation, superior radioulnar joint, buttonholing.
Elbow dislocations are commonly encountered by orthopedic surgeons all over. Management is straight forward and the result is generally satisfactory. However, in a small subset, associated injuries like convergent or divergent dislocations at superior radioulnar joints are present. These associated injuries are often missed initially leading to their delayed treatment and suboptimal elbow function. Convergent dislocation at the elbow is a rare injury [1,2,3]. It is extremely rare in adults. In convergent dislocation, superior radioulnar joint is disrupted with anterior crossover of the radius over ulna and always occurs in association with posterior ulnohumeral dislocation. Only two cases in adults and 23 in children have been reported in literature. Our case is the third one to be reported in adults, but the first case in India in adults. In our case, significant surgical difficulty was encountered because of buttonholing of the radial head in brachialis muscle.
A 68-year-old male visited a local hospital with a history of fall from a two-wheeler. An initial radiograph revealed an obvious posterior dislocation of the elbow as shown in Fig. 1. Closed reduction was performed and posterior above elbow slab was given (Fig. 2).  Patient presented to us 10 days later with persistent pain. Evaluation with radiographs confirmed reduction of ulno-humeral joint but translocation of the radius and ulna as shown in Fig. 3. The range of movement was 90° of flexion, limitation of terminal 10° extension, supination 20°, and pronation 60°. Patient did not have any neurovascular compromise. Patient was taken to the operation theater after due preparation and consent for possible open reduction was obtained beforehand. Closed reduction was attempted but was not successful. Open reduction was then performed using lateral approach to elbow. The radial head was found to be dislocated from the notch and was transposed to the anteromedial side of the ulna.
Patient presented to us 10 days later with persistent pain. Evaluation with radiographs confirmed reduction of ulno-humeral joint but translocation of the radius and ulna as shown in Fig. 3. The range of movement was 90° of flexion, limitation of terminal 10° extension, supination 20°, and pronation 60°. Patient did not have any neurovascular compromise. Patient was taken to the operation theater after due preparation and consent for possible open reduction was obtained beforehand. Closed reduction was attempted but was not successful. Open reduction was then performed using lateral approach to elbow. The radial head was found to be dislocated from the notch and was transposed to the anteromedial side of the ulna.  Reduction of the radial head was attempted. It was noted that buttonholing of radial head through brachialis fibers prevented reduction as shown in Fig. 4. Gradual release of brachialis fibers close to its insertion allowed reduction of radial head as shown in Fig. 5. Majority of fibers of brachialis had to be released to achieve reduction. The radial head showed an osteochondral defect involving about <1/5 posterior articular surface. Reduction was stable with elbow flexed beyond 40° but was unstable when flexion was <40°. Two transarticular radiocapitellar joint K-wires of 2 mm diameter passed with elbow in 90° of flexion and neutral forearm rotation as shown in intraoperative and position was confirmed on image intensifier as shown in Fig. 6.
Reduction of the radial head was attempted. It was noted that buttonholing of radial head through brachialis fibers prevented reduction as shown in Fig. 4. Gradual release of brachialis fibers close to its insertion allowed reduction of radial head as shown in Fig. 5. Majority of fibers of brachialis had to be released to achieve reduction. The radial head showed an osteochondral defect involving about <1/5 posterior articular surface. Reduction was stable with elbow flexed beyond 40° but was unstable when flexion was <40°. Two transarticular radiocapitellar joint K-wires of 2 mm diameter passed with elbow in 90° of flexion and neutral forearm rotation as shown in intraoperative and position was confirmed on image intensifier as shown in Fig. 6.  Annular ligament was found irreparable (friable) and elbow was reduced and stable with K wire fixation so annular ligament reconstruction was avoided. The wound was closed in layers. Post-operative posterior slab was applied. Post-operative radiographs confirmed congruent reduction of the olecranon and trochlea with the restoration of the radiocapitellar and radioulnar joints as shown in Fig. 7. Posterior above the elbow slab continued for 4 weeks with two K wires in situ as shown in Fig. 8.
Annular ligament was found irreparable (friable) and elbow was reduced and stable with K wire fixation so annular ligament reconstruction was avoided. The wound was closed in layers. Post-operative posterior slab was applied. Post-operative radiographs confirmed congruent reduction of the olecranon and trochlea with the restoration of the radiocapitellar and radioulnar joints as shown in Fig. 7. Posterior above the elbow slab continued for 4 weeks with two K wires in situ as shown in Fig. 8.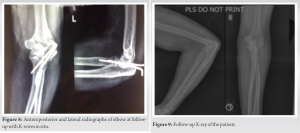 At 4 weeks, K wires and slab were removed and physiotherapy initiated. Patient visited us every month for 18 months. At the time of 18-month follow-up, X-ray of the patient was done Fig. 9 and patient had joined work as shopkeeper and was doing all activities that he was doing prior to injury including two-wheeler driving which is the main mode of transportation in this city. The range of movement at 18-month follow up was good, movement being 110° of flexion, fixed flexion deformity of 10°, supination 90°, and pronation 70° as shown in Fig. 10. The Mayo elbow performance score for affected side at 18-month follow-up was 95/100.
At 4 weeks, K wires and slab were removed and physiotherapy initiated. Patient visited us every month for 18 months. At the time of 18-month follow-up, X-ray of the patient was done Fig. 9 and patient had joined work as shopkeeper and was doing all activities that he was doing prior to injury including two-wheeler driving which is the main mode of transportation in this city. The range of movement at 18-month follow up was good, movement being 110° of flexion, fixed flexion deformity of 10°, supination 90°, and pronation 70° as shown in Fig. 10. The Mayo elbow performance score for affected side at 18-month follow-up was 95/100.
Literature review
Normally elbow dislocation is classified as simple elbow dislocation (without fracture) and complex elbow dislocation (associated with fracture). Another way of classification of elbow dislocation is according to direction of dislocation of ulna-posterior, posterolateral, posteromedial, lateral, medial, or divergent. Isolated dislocation of the radius at the elbow has been reported. It may be not diagnosed, it may be over-diagnosed as total dislocation of the elbow, or it may be belatedly diagnosed as a congenital dislocation of the radial head [4]. Many divergent fracture dislocations of the elbow have been reported [5,6]. Delee was first to report a case of transverse divergent dislocation of the elbow. Afshar in 2007 reported only 16 cases of divergent dislocation in English literature. Surprisingly mechanism of injury appears axial thrust and pronation, same as for convergent dislocation [7]. For convergent dislocations, there seems to be confusion about numbers reported so far. Lippe and Williams in an article in 2005 reported one case in adults and mentioned 10 cases of children reported in earlier literature [8]. However, as recently as 2007 Wodeci et al. in their case report mentioned five other cases (only) of this type and stated the diagnostic and therapeutic difficulties [9]. This confusion may be at least partly due to differing nomenclature adopted. MacSween first reported this condition in 1979 and named it transposition of radius and ulna. Closed reduction was possible in his case. Harvey and Tchélébi in 1979 reported this condition in a 7-year-old girl primarily treated for dislocation of the elbow and called it proximal radioulnar translocation. There was delay in diagnosis by 5 weeks and osteotomy of proximal ulna was required for reduction. 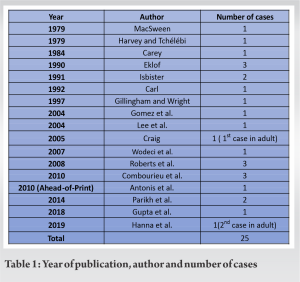 He also proposed that the condition is iatrogenic as a result of pronation during reduction of elbow dislocation. Subsequently Carey in 1984 reported two children of elbow dislocation with proximal radioulnar injury, for one he coined the term “convergent dislocation.” Another was termed a transverse divergent dislocation. He believed this to be the first case of convergent dislocation. Open reduction was required. Eklof in 1990 reported three cases from Sweden. He stressed that the clue to diagnosis is the reversed position of the bones of the proximal forearm. That is in the anteroposterior projection the radial head articulates with the trochlea and the ulna with the capitellum and that this unexpected anatomic relationship is easily overlooked. Isbister in 1991 described two cases and challenged the view that this injury is iatrogenic. Carl in 1992 reported a case, open reduction was required. Gillingham and Wright in 1997 reported a case in which a 6-year-old girl went undiagnosed for more than 2 weeks [10]. Definitive treatment required open reduction and use of a radiocapitellar pin to stabilize the proximal radius. Gomez et al. in 2004 reported neglected convergent dislocation in a 9-year-old boy, open reduction was required [11]. Lee et al. in 2004 reported a case in 10-year-old girl, stated that closed reduction was possible in his case which was only second instance of successful closed reduction after MacSween [12]. Lippe and Williams in 2005 reported first case in adult in a 35-year-old lady who presented with history of fall off a porch. Open reduction was required which was performed through lateral approach. Wodeci et al. in 2007 in his report of a 6-year-old child mentioned surgical reduction through medial approach. Roberts et al. in 2008 [13], Combourieu et al. in 2010 and Antonis et al. in 2010 reported more cases; closed reduction was possible in some [14,15]. Parikh et al. [16] in 2014 reported two cases of convergent elbow dislocation and Gupta et al. [17] in 2018 reported one case of convergent elbow dislocation in children. In 2019, second cases of convergent elbow dislocation reported by Hanna et al. [18] in adults. Hence, it appears that there are 25 confirmed cases, 23 being children. Only two cases are reported in adults. The reason for its extreme rarity in adults is not clear. Comparative weakness of annular ligament in children and hyperextension at elbow perhaps explains the difference. Table 1.
He also proposed that the condition is iatrogenic as a result of pronation during reduction of elbow dislocation. Subsequently Carey in 1984 reported two children of elbow dislocation with proximal radioulnar injury, for one he coined the term “convergent dislocation.” Another was termed a transverse divergent dislocation. He believed this to be the first case of convergent dislocation. Open reduction was required. Eklof in 1990 reported three cases from Sweden. He stressed that the clue to diagnosis is the reversed position of the bones of the proximal forearm. That is in the anteroposterior projection the radial head articulates with the trochlea and the ulna with the capitellum and that this unexpected anatomic relationship is easily overlooked. Isbister in 1991 described two cases and challenged the view that this injury is iatrogenic. Carl in 1992 reported a case, open reduction was required. Gillingham and Wright in 1997 reported a case in which a 6-year-old girl went undiagnosed for more than 2 weeks [10]. Definitive treatment required open reduction and use of a radiocapitellar pin to stabilize the proximal radius. Gomez et al. in 2004 reported neglected convergent dislocation in a 9-year-old boy, open reduction was required [11]. Lee et al. in 2004 reported a case in 10-year-old girl, stated that closed reduction was possible in his case which was only second instance of successful closed reduction after MacSween [12]. Lippe and Williams in 2005 reported first case in adult in a 35-year-old lady who presented with history of fall off a porch. Open reduction was required which was performed through lateral approach. Wodeci et al. in 2007 in his report of a 6-year-old child mentioned surgical reduction through medial approach. Roberts et al. in 2008 [13], Combourieu et al. in 2010 and Antonis et al. in 2010 reported more cases; closed reduction was possible in some [14,15]. Parikh et al. [16] in 2014 reported two cases of convergent elbow dislocation and Gupta et al. [17] in 2018 reported one case of convergent elbow dislocation in children. In 2019, second cases of convergent elbow dislocation reported by Hanna et al. [18] in adults. Hence, it appears that there are 25 confirmed cases, 23 being children. Only two cases are reported in adults. The reason for its extreme rarity in adults is not clear. Comparative weakness of annular ligament in children and hyperextension at elbow perhaps explains the difference. Table 1.
It seems that all cases of primarily posterior elbow dislocations are common but its association with convergent dislocations is rare. In routine radiographs of such cases, posterior elbow dislocation is obvious. However, the convergent dislocation component may not be obvious as the elbow is held in flexion and true anteroposterior view of the elbow in extension may not be obtained. It is only after closed reduction of posterior elbow dislocation that the other component that is convergent dislocation may become apparent and that this component has been missed in many cases for varying periods. In posterior elbow dislocations, careful observation of pre reduction anteroposterior view may offer a clue to the true nature of injury. Scrutiny of post reduction radiographs/Carm images with elbow extended is mandatory as is the need for awareness of this entity. The rarity of this condition is the reason for lack of awareness. In most cases, open reduction was required. Therefore, it appears that this continues to be a diagnostic as well as therapeutic problem. Our patient had no other associated bony injury except a marginal osteochondral fracture. The persistence of radiographic evidence of radial shortening in post-ulnohumeral reduction X-ray was mentioned as a possible clue to diagnosis by Lippe and Williams. In our case, there was no radial shortening seen in post-ulnohumeral reduction X-ray. Case reported by Lippe and Williams in adults had an ipsilateral intra articular distal radius fracture, probably that was the reason for radial shortening in his case. Our patient had no nerve injury nor myositis ossificans though ulnar nerve injury and myositis ossificans have been described in literature. In our case, closed reduction was not successful for convergent dislocation and we had to resort to open reduction. However, we wish to stress that open reduction also was difficult in our case because of buttonholing of the radial head through the brachialis insertion fibers and only after releasing the buttonholing, we were able to get a reduction. This contrasts with the previously reported case in adults wherein no specific surgical difficulty is mentioned during open reduction. Pre-operative MRI scan perhaps would have helped us to anticipate this buttonholing. In our case, the annular ligament was irreparable (friable). Radio capitellar pin was required for stability. This fixation method was earlier described by Gillingham and Wright in 1997 in his case. Our patient had a good functional result at 18 months and no complications despite a delay of 10 days in performing open reduction.
Translocation of the proximal radioulnar joint so called convergent dislocation is an extremely rare injury. Twenty-three cases in children and two cases in adults have been reported so far. Ours is the third case in adults to be reported in world literature, and first case reported from India. In contrast to the previous cases in adults, we encountered significant difficulty in open reduction because of button holing of radial head through brachialis insertion fibers and this has not been previously reported. Awareness of this surgical difficulty will save precious time during surgery.
This injury is frequently missed. We suggest careful scrutiny of pre-reduction anteroposterior radiographic view or 3D CT in suspected cases as well as X-ray/Carm anteroposterior view in extended position of elbow on the operation table immediately after reduction before slab application in every case of elbow dislocation. This precaution may help minimize instances of missing this injury.
References
- 1.MacSween WA. Transposition of radius and ulna associated with dislocation of the elbow in a child. Injury 1979;10:314-6. [Google Scholar | PubMed]
- 2.Harvey S, Tchélébi H. Proximal radio-ulnar translocation. A case report. J Bone Joint Surg Am 1979;61:447-9. [Google Scholar | PubMed]
- 3.Carey RP. Simultaneous dislocation of the elbow and the proximal radio-ulnar joint. J Bone Joint Surg Br 1984;66:254-6. [Google Scholar | PubMed]
- 4.Noyez JF. Isolated traumatic posterior dislocation of radial head: Report of two cases. Acta Orthop Belg 1996;62:148-50. [Google Scholar | PubMed]
- 5.Nanno M, Sawaizumi T, Ito H. Transverse divergent dislocation of the elbow with ipsilateral distal radius fracture in a child. J Orthop Trauma 2007;21:145-9. [Google Scholar | PubMed]
- 6.Altuntas AO, Balakumar J, Howells RJ, Graham HK. Posterior divergent dislocation of the elbow in children and adolescents: A report of three cases and review of the literature. J Pediatr Orthop 2005;25:317-21. [Google Scholar | PubMed]
- 7.Afshar A. Divergent dislocation of elbow in an 11-year-old child. Arch Iran Med 2007;10:413-6. [Google Scholar | PubMed]
- 8.Lippe CN, Williams DP. Combined posterior and convergent elbow dislocations in an adult. A case report and review of the literature. J Bone Joint Surg Am 2005;87:1597-600. [Google Scholar | PubMed]
- 9.Wodeci P, Maiza D, Rozenblum B. Elbow dislocation in children associated with proximal radioulnar translocation. Rev Chir Orthop Reparatrice Appar 2007;93:190-4. [Google Scholar | PubMed]
- 10.Gillingham BL, Wright JG. Convergent dislocation of the elbow. Clin Orthop Relat Res 1997;340:198-201. [Google Scholar | PubMed]
- 11.Gomez JG, Sancho FG, Adrian JG. Elbow dislocation with proximal radioulnar translocation. Rev Espan Cir Osteoarticul 2004;39:N217. [Google Scholar | PubMed]
- 12.Lee BJ, Lee SR, Shin DH. Proximal radioulnar translocation associated with elbow dislocation. Case report. J Korean Orthop Assoc 2004;39:5825. [Google Scholar | PubMed]
- 13.Roberts C, Lee TS, Rooney J, Jovanovic A, Creer R. Convergent dislocation of the elbow: Report of three cases. J Shoulder Elbow Surg 2008;17:e9-13. [Google Scholar | PubMed]
- 14.Combourieu B, Thevenin-Lemoine C, Abelin-Genevois K, Mary P, Damsin JP, Vialle R. Pediatric elbow dislocation associated with proximal radioulnar translocation: A report of three cases and a review of literature. J Bone Joint Surg Am 2010;92:1780-5. [Google Scholar | PubMed]
- 15.Antonis K, Leonidou OA, Sbonias G, Fligger I. J Pediatr Orthop B 2010. [Google Scholar | PubMed]
- 16.Parikh SN, Lykissas MG, Mehlman CT, Sands S, Herrera- Soto J, Panchal A et al. Convergent and divergent dislocation of the pediatric elbow: Two case reports and comprehensive review of literature. J Pediatr Orthop B 2014;23:158-67. [Google Scholar | PubMed]
- 17.Gupta G, Makadia AS, Shah MM. An unreported variant of convergent dislocation of elbow. J Orthop Case Rep 2018;8:79-81. [Google Scholar | PubMed]
- 18.Hanna WA, Laier P, Müller CA. Combined convergent elbow dislocation with posterior luxation of the humeroulnar joint and radial head comminuted fracture in adults. Unfallchirurg 2019;122:736-743. [Google Scholar | PubMed]