Symptomatic Fishtail deformities can occur in minimally displaced supracondylar humerus fractures.
Dr. Ethan Sawyer, Department of Orthopedics, University of Toledo Medical Center, Toledo, Ohio, USA. E-mail: ethan.sawyer@utoledo.edu
Introduction: Supracondylar humerus fractures are one of the most common fractures in children and have been reported to represent up to 16% of all pediatric fractures. While most fractures heal uneventfully with appropriate treatment, there are several known complications that can occur including loss of motion, malunion, and neurovascular injury. One uncommon, yet significant, complication is termed the “Fishtail” deformity. This is represented radiographically with apparent proximal migration of the trochlea, which is thought to be secondary to avascular necrosis and resulting growth arrest.
Case Report: This case describes a 11-year-old male who developed a fishtail deformity at age 5, 5 months after percutaneous pinning of a Type II supracondylar humerus fracture. Initially demonstrating a tolerable loss of elbow range of motion (ROM) and being lost to follow-up, he returned 7-years postoperatively, demonstrating diffuse elbow degenerative changes and worsening mechanical symptoms secondary to a loose body which necessitated arthroscopic debridement and loose body removal.
Conclusion: This case illustrates the rare fishtail deformity in a Type II supracondylar humerus fracture with acute onset mechanical symptoms of the elbow secondary to a large loose body. Patients with history of supracondylar humerus fractures can develop acute or worsening changes in elbow ROM secondary to the development of osteochondral loose bodies even in the setting of previously known motion deficits secondary to fishtail deformities.
Keywords: Fishtail deformity, supracondylar humerus, gartland Type II.
Supracondylar humerus fractures are one of the most common fractures in children and have been reported to represent up to 16% of all pediatric fractures [1]. While most fractures heal uneventfully with appropriate treatment, there are several known complications that can occur including loss of motion, malunion, and neurovascular injury [2,3]. One uncommon, yet significant, complication is termed the “Fishtail” deformity. This is represented radiographically with apparent proximal migration of the trochlea, which is thought to be secondary to avascular necrosis and resulting growth arrest [4]. This complication is typically seen following significantly displaced fractures [5] and few case reports exist in minimally, or non-displaced fractures [6,7]. Given the infrequent identification of this finding following supracondylar humerus fractures, little is written about the sequelae of this condition, or its management [8]. This case report illustrates the clinical progression a 11-year-old male who developed a fishtail deformity after routine closed reduction and percutaneous pinning (CRPP) as a 4 year old following a Gartland Type II (Type II) supracondylar humerus fracture, followed by late-onset mechanical symptoms and the development of a loose body 7-years postoperatively.
This patient initially presented to our emergency department at 4 years, 7 months of age after an injury to the left elbow while wrestling at home. He was found to have a Gartland Type II supracondylar humerus fracture (Fig. 1). 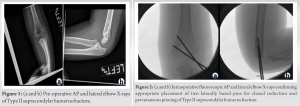 At that time, he underwent uncomplicated CRPP with two laterally based pins (Fig. 2). He underwent routine post-operative management and pins were removed 4-week postoperatively. He was seen 6 weeks after pin removal for clinical check, had full range of motion (ROM) of his elbow, and was at that time released for follow-up on an as needed basis. He returned for reevaluation 5-months postoperatively after sudden, non-painful inability to extend his elbow past 30°. Radiographs were obtained which demonstrated early signs of a fishtail deformity (Fig. 3) with central growth arrest of the distal humerus.
At that time, he underwent uncomplicated CRPP with two laterally based pins (Fig. 2). He underwent routine post-operative management and pins were removed 4-week postoperatively. He was seen 6 weeks after pin removal for clinical check, had full range of motion (ROM) of his elbow, and was at that time released for follow-up on an as needed basis. He returned for reevaluation 5-months postoperatively after sudden, non-painful inability to extend his elbow past 30°. Radiographs were obtained which demonstrated early signs of a fishtail deformity (Fig. 3) with central growth arrest of the distal humerus.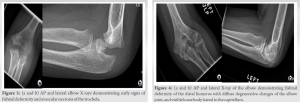 At the time of evaluation, his loss of motion had improved spontaneously, and a course of physical therapy was prescribed with a plan for continued observation of the deformity; however, he was lost to follow-up at that time. Several years later, he represented to our clinic, now at the age of 11 years, 5 months, approximately 7 years postoperatively, complaining of acute onset locking of his elbow with limitations in both extension to 30° and in flexion to 95°. In the interval between his previous visits, he noted occasional locking events of his elbow some of which required passive “unlocking” of his elbow but overall had good function of the elbow. As this was his non-dominant arm, these symptoms did not prevent him from participating in recreational sporting activities such as basketball or baseball. Radiographs were obtained, which revealed worsening of the fishtail deformity with chronic appearing degenerative changes of the elbow with a resultant loose body, osteophytosis, and deformities of the trochlea, capitellum, and olecranon (Fig. 4). A CT scan of the elbow was also obtained which further characterized the fishtail deformity of the distal humerus with central growth arrest, proximal migration of the trochlea, and ulnotrochlear joint derangement.
At the time of evaluation, his loss of motion had improved spontaneously, and a course of physical therapy was prescribed with a plan for continued observation of the deformity; however, he was lost to follow-up at that time. Several years later, he represented to our clinic, now at the age of 11 years, 5 months, approximately 7 years postoperatively, complaining of acute onset locking of his elbow with limitations in both extension to 30° and in flexion to 95°. In the interval between his previous visits, he noted occasional locking events of his elbow some of which required passive “unlocking” of his elbow but overall had good function of the elbow. As this was his non-dominant arm, these symptoms did not prevent him from participating in recreational sporting activities such as basketball or baseball. Radiographs were obtained, which revealed worsening of the fishtail deformity with chronic appearing degenerative changes of the elbow with a resultant loose body, osteophytosis, and deformities of the trochlea, capitellum, and olecranon (Fig. 4). A CT scan of the elbow was also obtained which further characterized the fishtail deformity of the distal humerus with central growth arrest, proximal migration of the trochlea, and ulnotrochlear joint derangement. 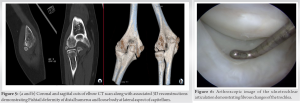 This also demonstrated a large loose body located at the posterolateral aspect of the capitellum (Fig. 5 and 6). Due to the worsening mechanical symptoms of in the setting of a loose body, diagnostic arthroscopy of the elbow with removal of the loose body was performed. Although the preoperative imaging showed proximal migration of the bony trochlea, we found that there was a fibrous anlage articulating with the proximal ulna (Fig. 7). The capitellum was found to be irregular, likely representing the donor site of the known loose osteochondral fragment. The loose body measured 1.5 cm × 1 cm (Fig. 8) and was excised through a posterolateral incision. Examination under anesthesia was performed after loose body excision which showed improvement in ROM from 30° to 95° preoperatively to 0–120° (Fig. 9).
This also demonstrated a large loose body located at the posterolateral aspect of the capitellum (Fig. 5 and 6). Due to the worsening mechanical symptoms of in the setting of a loose body, diagnostic arthroscopy of the elbow with removal of the loose body was performed. Although the preoperative imaging showed proximal migration of the bony trochlea, we found that there was a fibrous anlage articulating with the proximal ulna (Fig. 7). The capitellum was found to be irregular, likely representing the donor site of the known loose osteochondral fragment. The loose body measured 1.5 cm × 1 cm (Fig. 8) and was excised through a posterolateral incision. Examination under anesthesia was performed after loose body excision which showed improvement in ROM from 30° to 95° preoperatively to 0–120° (Fig. 9). 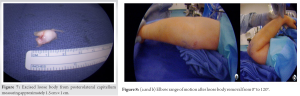 Postoperatively, he was placed in a hinged elbow brace to allow for a progressive ROM protocol. By 10-weeks postoperatively, he was pain free and had regained his baseline ROM and was allowed to begin returning to sport like activities. No further loose body symptoms were noted.
Postoperatively, he was placed in a hinged elbow brace to allow for a progressive ROM protocol. By 10-weeks postoperatively, he was pain free and had regained his baseline ROM and was allowed to begin returning to sport like activities. No further loose body symptoms were noted.
Central physeal arrest, or fishtail deformity, secondary to avascular necrosis of the trochlea, is a rare complication of supracondylar humerus fractures [5,7]. There are few case reports in the literature reporting this complication, with the majority being Type III fractures [7]. Even fewer examples exist of this complication in Type I and Type II fractures [7]. One potential contributing factor to developing this complication is the watershed area of intraosseous vascularity in between the condyles and humeral shaft distally. This vascular insufficiency can be further exacerbated by fractures and internal fixation [9]. Considering this, avascular necrosis of the trochlea and resultant fishtail deformity has the potential to occur in any pediatric distal humerus fracture. As such, it has been described as complications of both medial and lateral condyle fractures, distal humeral physeal separations, T-type condylar distal humerus fractures, and supracondylar fractures [6]. Though rare, the possibility of subsequent deformity at the elbow should be discussed with parents upon initiation of treatment even in non or minimally displaced fractures. Of the existing reports of fishtail deformities after supracondylar humerus fractures, the diagnosis is typically made years after the injury [5,6]. Given the infrequent identification of this finding following supracondylar humerus fractures, there is little written about the sequelae of this complication, or its management [6]. Furthermore, many children who develop a fishtail are asymptomatic for years and may not develop symptoms from early degenerative elbow arthrosis until adulthood [10]. The most common complaints associated with these deformities are pain, decreased ROM and crepitus [7]. There are a range of operative options available which include: Open or arthroscopic debridement with capsulotomy, revascularization by bone drilling, prevention of deformity progression by hemiepiphysisodesis of remaining open physis medially and laterally [7,10]. However, there is little long-term outcome data available regarding the ability to alleviate symptoms in the short-term or preventing future degenerative sequelae. Our patient developed symptoms with decreased ROM as early as 5 months post-injury with early radiographic evidence of a fishtail deformity. However, these early symptoms improved spontaneously, and he was lost to follow-up. On representation at 7-years post-injury, the patient had acute worsening of his elbow ROM and mechanical symptoms, and a CT scan demonstrating diffuse degenerative changes of the elbow joint with reactive osteophytosis and development of a large loose body. Our hypothesis is that the fibrous trochlear anlage that was encountered during arthroscopy, allowed for varus/valgus instability of the ulnotrochlear joint with subsequent overloading of the radiocapitellar joint. In this patient, we suspect that this led him to develop an unstable capitellar osteochondritis dissecans (OCD) lesion. OCD, which is thought to be due to repetitive mechanical loading of an at-risk articular surface, is a common cause of loose osteochondral bodies in young people [11]. Intraoperative ROM was vastly improved in the operating room on excision of the loose body, which confirmed our suspicion that this was the cause of his block to motion. This case report illustrates a rare case of rapid development of a fishtail deformity after undergoing routine CRPP and post-operative management for a minimally displaced Type II supracondylar humerus fracture and developed mechanical symptoms as soon as 5-months postoperatively, was lost to follow-up, then subsequently went onto develop a symptomatic loose body 7-years postoperatively. Given the fact that many of these deformities may be asymptomatic initially [7], it is likely they are underdiagnosed, as most patients are not followed radiographically beyond 1 month from surgery, once callus formation has been identified [12]. In the author’s practice, routine post-operative management after CRPP of supracondylar humerus fractures includes obtaining radiographs before pulling the pins at 3–4-week postoperatively and subsequent follow-up to evaluate elbow ROM [12,13]. Previous studies have shown that 94% of patients reached elbow ROM equal to the contralateral arm by 6 months postoperatively [13]. In light of this, and the possibility of developing a fishtail deformity as early as 5-months postoperatively, a sudden decrease in elbow ROM years after even minimally displaced supracondylar humerus fractures may warrant further investigation. This case demonstrates not only the possibility of rapidly developing a fishtail deformity after a minimally displaced Type II supracondylar humerus fracture, but also that a mechanically symptomatic loose body can be a reason for late presentation of these deformities.
This case illustrates the rare fishtail deformity in a Type II supracondylar humerus fracture with acute onset mechanical symptoms of the elbow secondary to a large loose body. Patients with history of supracondylar humerus fractures can develop acute or worsening changes in elbow ROM secondary to the development of osteochondral loose bodies even in the setting of previously known motion deficits secondary to fishtail deformities.
Sequalae from fishtail deformities might be considered on the differential diagnoses for patients with decreased elbow range of motion and a history of even nondisplaced supracondylar humerus fractures.
References
- 1.Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups: A study of 3,350 children. J Orthop Trauma 1993;7:15-22. [Google Scholar | PubMed]
- 2.Tomaszewski R, Pethe K, Kler J, Rutz E, Mayr J, Dajka J. Supracondylar fractures of the humerus: Association of neurovascular lesions with degree of fracture displacement in children – A retrospective study. Children (Basel) 2022;9:308. [Google Scholar | PubMed]
- 3.Azzam W, Catagni MA, Ayoub MA, El-Sayed M, Thabet AM. Early correction of malunited supracondylar humerus fractures in young children. Injury 2020;51:2574-80. [Google Scholar | PubMed]
- 4.Howard A, Mulpuri K, Abel MF, Braun S, Bueche M, Epps H, et al. The treatment of pediatric supracondylar humerus fractures. J Am Acad Orthop Surg 2012;20:320-7. [Google Scholar | PubMed]
- 5.Bronfen CE, Geffard B, Mallet JF. Dissolution of the trochlea after supracondylar fracture of the humerus in childhood: An analysis of six cases. J Pediatr Orthop 2007;27:547-50. [Google Scholar | PubMed]
- 6.Glotzbecker MP, Bae DS, Links AC, Waters PM. Fishtail deformity of the distal humerus: A report of 15 cases. J Pediatr Orthop 2013;33:592-7. [Google Scholar | PubMed]
- 7.Ott N, Hackl M, Leschinger T. Predictors of avascular necrosis of the trochlea after pediatric supracondylar humerus fractures. Obere Extremität 2020;15:301-6. [Google Scholar | PubMed]
- 8.Yamaga T, Horii E, Koh S, Sugiura H. Osteochondritis dissecans of the capitellum secondary to fishtail deformity treated with osteochondral autograft. JSES Open Access 2018;2:126-8. [Google Scholar | PubMed]
- 9.Kimball JP, Glowczewskie F, Wright TW. Intraosseous blood supply to the distal humerus. J Hand Surg Am 2007;32:642-6. [Google Scholar | PubMed]
- 10.Nwakama AC, Peterson HA, Shaughnessy WJ. Fishtail deformity following fracture of the distal humerus in children: Historical review, case presentations, discussion of etiology, and thoughts on treatment. J Pediatr Orthop B 2000;9:309-18. [Google Scholar | PubMed]
- 11.Chau MM, Klimstra MA, Wise KL, Ellermann JM, Tóth F, Carlson CS, et al. Osteochondritis dissecans: Current understanding of epidemiology, etiology, management, and outcomes. J Bone Joint Surg Am 2021;103:1132-51. [Google Scholar | PubMed]
- 12.Garg S, Bloch N, Cyr M, Carry P. Routine radiographs at time of pin removal after closed reduction and percutaneous pinning for type 2 supracondylar humerus fractures do not change management: A retrospective cohort study. J Child Orthop 2016;10:329-33. [Google Scholar | PubMed]
- 13.Zionts LE, Woodson CJ, Manjra N, Zalavras C. Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin Orthop Relat Res 2009;467:2007-10. [Google Scholar | PubMed]








