Clinicians must be aware about tuberculosis of pubic symphysis and its recurrence. They must also obtain biopsy in recurrence cases to rule out resistance to Anti Tubercular Therapy.
Dr. Nitish Kumar, Department of Orthopedics, All India Institute of Medical Sciences, Gorakhpur, Uttar Pradesh, India. E-mail: nitishaiims@gmail.com
Introduction: Tuberculosis (TB) of pubic symphysis is an extremely uncommon condition accounting <1% of all musculoskeletal TB. Further recurrence of TB of symphysis pubis is a rare clinical scenario requiring a high level of suspicion for diagnosing the condition. Recurrence of tuberculosis can occur either be due to relapse of the original infection or reinfection due to exogenous Mycobacterium tuberculosis strain. There have only been nine case reports on TB of the pubic symphysis in the last three decades and only 40 patients were identified in English language medical literature so to the best of our knowledge this is the first case report on the recurrence of TB of pubic symphysis.
Case Report: A 26-year-old female patient presented with pain over symphyseal area for 2 months. Laboratory and radiological investigations were suggestive of TB of symphysis pubis. She was started on oral, category I anti-tubercular therapy (ATT) from DOTS center. Patient on improvement in symptoms discontinued taking ATT after 6 months. About 7 months after stopping ATT, she again presented with pain over symphyseal area and difficulty in walking. Laboratory, radiological investigation, and biopsy were obtained to rule out multidrug-resistant (MDR) TB. The patient improved on 12 months’ oral daily ATT regime (HRZES2+HRZE4+HRE6). She was followed up for another 1 year with clinical examination and laboratory investigation after stopping ATT. At present, she is asymptomatic with no signs of recurrence after 1 year of completion of treatment.
Conclusion: ATT intake should be continued for 12 months for musculoskeletal TB for preventing recurrence. The biopsy needs to be taken from the affected region in recurrence TB to rule out MDR.
Keywords: Recurrence, tuberculosis, pubic symphysis.
With increasing incidence of immunodeficiency disorders and use of tumor necrosis factor-α-antagonist patients are predisposed to tuberculosis which can involve uncommon sites of the body. Pubic bone tuberculosis (TB) accounts for <1% of all musculoskeletal TB [1]. The clinicians need to have a high degree of suspicion in patients at risk of presenting with groin or adductor pain and waddling or antalgic gait. Initially, the patient may be asymptomatic with an abscess or swelling in hypogastric, perineal, mid-thigh, and ischio-rectal area [1]. Lack of awareness with varied clinical presentation may hamper early diagnosis of advanced disease. Moreover, a recurrence of the disease after early intervention presents the challenge to the clinicians about the management of the disease [2].
A 26-year-old female presented with chief complaints of pain over lower abdomen and difficulty in walking for 2 months. The pain was present over symphyseal area, which was insidious in onset, gradually progressive and aggravated with walking. She had a history of intermittent fever associated with loss of appetite but no significant weight loss. She had no gynecological or urogenital complaints. On examination, there was tenderness over symphyseal region which gets aggravated by attempting pelvic compression and distraction test. There was associated tenderness in the proximal thigh over medial aspect on right side. Examination of bilateral iliac crest, bilateral ischial tuberosity, and bilateral hip joints were normal. There was no lymphadenopathy in the inguinal region and bilateral iliac fossa. A plain anteroposterior (AP) radiograph of the pelvis with bilateral hip joint showed a lytic area in the symphysis pubis with suspicion of widening of the symphysis pubis (Fig. 1).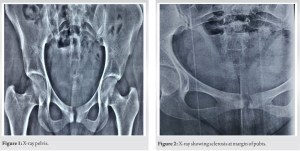 Her erythrocyte sedimentation rate (ESR) was 90 mm 1st h, qualitative C-reactive protein (CRP) was raised, total leucocyte count (TLC) and other blood parameters were normal. Plain magnetic resonance imaging (MRI) of pelvis showed subtle focal cortical erosion in the right pubic bone with signal alteration just lateral to pubic symphysis along with ill-defined T1 hypo and T2 and STIR hyperintense collection within a proximal medial compartment of the right thigh along with surrounding soft tissue edema suggestive of infective etiology in favor of tuberculosis. Based on clinicoradiological findings and supportive evidence of hematological investigations, she was diagnosed as a case of tubercular infection of the symphysis pubis. She was started on first-line anti-tubercular therapy (ATT) from DOTS Centre along with pelvic binder support. She received four tablets of fixed-dose H/R/Z/E combination containing 75 mg/150 mg/400 mg/275 mg for 2 months and then four tablets of fixed-dose H/R/E combination containing 75 mg/150 mg/275 mg for 4 months. At the end of 6 months, her pain had subsided, tenderness was absent, gait had improved and there was no pain while walking. The ESR and CRP were normal. X-ray pelvis AP view showed sclerosis of the margins (Fig. 2). She was advised to continue ATT for 6 more months, which she was not compliant and stopped her ATT after total 6 months of treatment (2HRZE+4HRE) against advice. Around 7 months after discontinuing ATT intake, she again presented with complaints of pain in symphyseal region with difficulty in walking. Her ESR and CRP were raised. Other hematological investigations including HIV, Blood sugar, TLC, etc. were normal. X-ray pelvis with bilateral hip AP view showed regional osteopenia along with gross bony destruction of symphysis pubis with pubic diastasis (Fig. 3).
Her erythrocyte sedimentation rate (ESR) was 90 mm 1st h, qualitative C-reactive protein (CRP) was raised, total leucocyte count (TLC) and other blood parameters were normal. Plain magnetic resonance imaging (MRI) of pelvis showed subtle focal cortical erosion in the right pubic bone with signal alteration just lateral to pubic symphysis along with ill-defined T1 hypo and T2 and STIR hyperintense collection within a proximal medial compartment of the right thigh along with surrounding soft tissue edema suggestive of infective etiology in favor of tuberculosis. Based on clinicoradiological findings and supportive evidence of hematological investigations, she was diagnosed as a case of tubercular infection of the symphysis pubis. She was started on first-line anti-tubercular therapy (ATT) from DOTS Centre along with pelvic binder support. She received four tablets of fixed-dose H/R/Z/E combination containing 75 mg/150 mg/400 mg/275 mg for 2 months and then four tablets of fixed-dose H/R/E combination containing 75 mg/150 mg/275 mg for 4 months. At the end of 6 months, her pain had subsided, tenderness was absent, gait had improved and there was no pain while walking. The ESR and CRP were normal. X-ray pelvis AP view showed sclerosis of the margins (Fig. 2). She was advised to continue ATT for 6 more months, which she was not compliant and stopped her ATT after total 6 months of treatment (2HRZE+4HRE) against advice. Around 7 months after discontinuing ATT intake, she again presented with complaints of pain in symphyseal region with difficulty in walking. Her ESR and CRP were raised. Other hematological investigations including HIV, Blood sugar, TLC, etc. were normal. X-ray pelvis with bilateral hip AP view showed regional osteopenia along with gross bony destruction of symphysis pubis with pubic diastasis (Fig. 3). MRI revealed area of destruction and altered marrow edema in bilateral pubic symphysis with adjacent soft tissue component in the anterior pelvis with pubic diastasis (Fig. 4). It also showed two sinuses, one present on right side extending from right pubic symphysis into the right upper thigh around obturator muscle and another sinus is seen from the posterior cortex of right pubic symphysis extending from 3 cm and terminating 0.4 cm from vaginal vault. A fluoroscopic-guided biopsy was done (Fig. 5) under local anesthesia. The patient was taken supine on a radiolucent table after emptying her bladder. Cleaning and draping were done as per standard sterile protocol.
MRI revealed area of destruction and altered marrow edema in bilateral pubic symphysis with adjacent soft tissue component in the anterior pelvis with pubic diastasis (Fig. 4). It also showed two sinuses, one present on right side extending from right pubic symphysis into the right upper thigh around obturator muscle and another sinus is seen from the posterior cortex of right pubic symphysis extending from 3 cm and terminating 0.4 cm from vaginal vault. A fluoroscopic-guided biopsy was done (Fig. 5) under local anesthesia. The patient was taken supine on a radiolucent table after emptying her bladder. Cleaning and draping were done as per standard sterile protocol.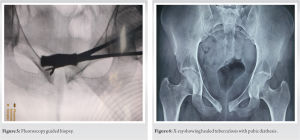 15 mL of 2% plain lignocaine was infiltrated in skin, subcutaneous tissue, and periosteum over the right side of the symphysis pubis after checking drug sensitivity. A core biopsy needle was used to harvest biopsy from the margin of the right pubic symphysis after confirming its position on the image intensifier. The sample was analyzed by CBNAAT for any drug resistance. There was no drug resistance found in this patient. The patient was leveled as relapse of pubic symphysis tuberculosis and started on daily ATT (HRZES2+HRZE4+HRE6) regime for 12 months. The patient was followed every 3 months with ESR, liver function test, and kidney function test. On completion of her ATT course at 12 months, her ESR and CRP were normal, X-ray pelvis AP view showed sclerosis of margin of pubic symphysis with diathesis (Fig. 6). Her constitution symptoms were absent, and her general physical conditions have improved. After completion of ATT, she was followed every 3 months with clinical examination, ESR level for 1 year. She remains asymptomatic for 1 year of her follow-up.
15 mL of 2% plain lignocaine was infiltrated in skin, subcutaneous tissue, and periosteum over the right side of the symphysis pubis after checking drug sensitivity. A core biopsy needle was used to harvest biopsy from the margin of the right pubic symphysis after confirming its position on the image intensifier. The sample was analyzed by CBNAAT for any drug resistance. There was no drug resistance found in this patient. The patient was leveled as relapse of pubic symphysis tuberculosis and started on daily ATT (HRZES2+HRZE4+HRE6) regime for 12 months. The patient was followed every 3 months with ESR, liver function test, and kidney function test. On completion of her ATT course at 12 months, her ESR and CRP were normal, X-ray pelvis AP view showed sclerosis of margin of pubic symphysis with diathesis (Fig. 6). Her constitution symptoms were absent, and her general physical conditions have improved. After completion of ATT, she was followed every 3 months with clinical examination, ESR level for 1 year. She remains asymptomatic for 1 year of her follow-up.
TB infection occurs by Mycobacterium tuberculosis complex (MTBC) and is a major public health threat. Most of the TB patients gets effectively cured using a combination of anti-tubercular drug treatment regimens when given in adequate dose and duration [3]. However, some patient still exhibits recurrence of tuberculosis after completion of treatment which adds considerably to the burden of TB cases worldwide. Recurrence can either be due to relapse of an original infection or reinfection by new MTBC strain. Risk factors for recurrence include length of time <2 years for endogenous relapse whereas co-infection with HIV, Beijing family genotype, imprisonment, and immigrations are associated with exogenous reinfection [1,2]. Relapse and failure can be seen as different expressions of the same problem. True relapse can only be deemed if tuberculous bacilli still persist after an apparent cure which account to inadequate treatment either regimen or duration wise [2]. True relapse is most likely to occur soon after completion of treatment for the first episode by contrast recurrence due to reinfection is a constant risk over time. In a BMRC trial with 5 years’ follow-up most of recurrences were found to occur within 6 months of post therapy [3]. Some authors have proposed to define late failure as any recurrence within first 6 months after the end of treatment. The two pubic bones meet in the midline at pubic symphysis (a secondary cartilaginous joint). The articulating surfaces are covered by a thin layer of tightly adherent hyaline cartilage which are connected by fibrocartilage, varying in thickness and constituting inter-pubic disc which is strengthened anteriorly by anterior pubic ligament and posteriorly by posterior pubic ligaments [4]. Although the main ligaments are superior and arcuate pubic ligament which along with inter-pubic disc are the main stabilizing factors of pubic symphysis. The pubic symphysis is supplied by pubic branches of the obturator, superficial external pudendal and inferior epigastric arteries while it is innervated by branches from iliohypogastric, ilioinguinal, and pudendal nerves [4,5,6]. Infection leads to formation of metaphyseal abscess destruction of bone and loss of nutrition to hyaline cartilage. The cartilaginous part may get destroyed by infection leading to symphyseal widening (Fig. 6). It is very important to diagnose this condition at early stage and treat it adequately before it causes pubic diastasis leading to sacroiliac strain and pelvic instability. Pain is the most common presenting symptoms followed by swelling which could be painless in groin, pubic or inguinal region which may be of horseshoe shape rarely. Due to paucity of clinically diagnosed cases of TB of pubic symphysis, these swelling may be attributed to lipoma, hernia or soft tissue tumor in early stages [1,7,8,9,10,11,12]. Pain may be dull aching and moderate in the symphyseal area, lower abdomen, pubic, inguinal, suprapubic, lumbar, hip, and pelvic regions [7]. The cold abscess from pubic symphysis may track along natural passages may present at distance away from its origin. It may track to medial side of thigh along fascia of adductor muscle (present in our case), or may present in perineal area, inguinal area etc. [6,13]. The pressure due to abscess collection in retro pubic space (Cave of Retzius) may lead to urinary symptoms like polyuria. Patient may also present osteuria or pyuria if the abscess perforates the bladder. Constitutional symptoms are usually not present due to slow progress of the disease. In our case she does had intermittent fever with loss of appetite, but she did not have significant loss of weight at the time of initial presentation. MRI is good modality for early diagnosis of the condition even before X-ray picks up the bony changes. The bone marrow edema which may be hypointense on T1 and hyperintense on T2 as well as any adjacent soft tissue involvement may give sufficient corroborative evidence to diagnose ongoing infective etiology. It will also show anatomic details of abscess, fistula bony defects etc. In our patient MRI has shown two sinuses, one present on right side extending from right pubic symphysis into the right upper thigh around obturator muscle and another sinus is seen from posterior cortex of right pubic symphysis extending from 3 cm and terminating 0.4 cm from vaginal vault apart from usual signs of infection like oedema and bony destruction. It is good practice to establish diagnosis of TB on histopathology or on positive smear for acid fast bacilli from aspirates/biopsy. CBNAAT from the biopsy/aspirates have proven fast and reliable method of establishing diagnosis of tuberculosis and resistant to any conventional ATT. Pubic symphysis is easily palpable hence biopsy can be obtained easily. But it is very important to be aware about important vital structures present around the symphysis pubis. Secondly the inclination of pubic symphysis is such that biopsy needle may injure urinary bladder if it is not aligned properly. Hence it is advisable needle biopsy should be done under fluoroscopic guidance after emptying the bladder. With daily doses of ATT for adequate duration, the tubercular infection can be controlled in majority of the patients [4]. However, some patient may present as recurrence of the disease if there has been incomplete course of therapy or if infected by a new strain. In our patient we attributed to this recurrence as reactivation of previous infection because of incomplete therapy and relapse of the disease within 2 years of completion of therapy without any presence of concomitant HIV or any other immunocompromised state. To the best of our knowledge this is the first known case report on recurrence of tubercular pubic symphysis.
Noncompliance to oral ATT can lead to recurrence of TB. For musculoskeletal TB oral daily dose of ATT should be continued for nine to 12 months. In case of recurrence biopsy must be obtained to rule out multidrug-resistant (MDR) TB. Our patient had stopped ATT intake after 6 months and presented with recurrence. Biopsy from symphyseal area had ruled out MDR TB, and further 12 month course of ATT administration has healed her TB. She remained asymptomatic for another year during her regular follow up with clinical examination and laboratory investigations.
The clinician should have high index of suspicion regarding recurrence of TB in areas with rare occurrence of tuberculosis like symphysis pubis. The patients should be encouraged to complete full course of ATT and in case recurrence is suspected biopsy must be obtained to rule out MDR TB. Patient should be regularly followed up after stopping ATT as per standard protocol.
References
- 1.Lal H, Jain VK, Kannan S. Tuberculosis of the pubic symphysis: Four unusual cases and literature review. Clin Orthop Relat Res 2013;471:3372-80. [Google Scholar | PubMed]
- 2.Zong Z, Huo F, Shi J, Jing W, Ma Y, Liang Q, et al. Relapse versus reinfection of recurrent tuberculosis patients in a national tuberculosis specialized hospital in Beijing, China. Front Microbiol 2018;9:1858. [Google Scholar | PubMed]
- 3.Mitchison D, Davies G. The chemotherapy of tuberculosis: Past, present and future. Int J Tuberc Lung Dis 2012;16:724-32. [Google Scholar | PubMed]
- 4.Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: A systematic review. J Anat 2010;217:475-87. [Google Scholar | PubMed]
- 5.Garg D, Goyal V. Spinal tuberculosis treatment: An enduring bone of contention. Ann Indian Acad Neurol 2020;23:441-8. [Google Scholar | PubMed]
- 6.Bali K, Kumar V, Patel S, Mootha AK. Tuberculosis of symphysis pubis in a 17 year old male: A rare case presentation and review of literature. J Orthop Surg Res 2010;5:63. [Google Scholar | PubMed]
- 7.Gamble JG, Simmons SC, Freedman M. The symphysis pubis. Anatomic and pathologic considerations. Clin Orthop Relat Res 1986;203:261-72. [Google Scholar | PubMed]
- 8.Rozadilla A, Nolla JM, Rodriguez J, Del Blanco J, Escofet DR. Tuberculosis of the pubis symphysis. J Rheumatol 1991;18:1271-2. [Google Scholar | PubMed]
- 9.Manzaneque L, Marin I, García-Bragado F, Beiztegui A, Dastis C, Sánchez-Matas P. Osteoarticular tuberculosis of the symphysis pubis presenting as a hypogastric cystic mass in a woman with primary Sjögren’s syndrome. Br J Rheumatol 1992;31:495-6. [Google Scholar | PubMed]
- 10.Tsay MH, Chen MC, Jaung GY, Pang KK, Chen BF. Atypical skeletal tuberculosis mimicking tumor metastases: Report of a case. J Formos Med Assoc 1995;94:428-31. [Google Scholar | PubMed]
- 11.Benbouazza K, Allali F, Bezza A, El Hassani S, El Maghraoui A, Lazrak N, et al. Pubic tuberculous osteo-arthritis. Apropos of 2 cases. Rev Chir Orthop Reparatrice Appar Mot 1997;83:670-2. [Google Scholar | PubMed]
- 12.Balsarkar DJ, Joshi MA. Tuberculosis of pubic symphysis presenting with hypogastric mass. J Postgrad Med 2001;47:54. [Google Scholar | PubMed]
- 13.Bayrakci K, Daglar B, Tasbas BA, Agar M, Gunel U. Tuberculosis osteomyelitis of symphysis pubis. Orthopedics 2006;29:948-50. [Google Scholar | PubMed]











