Understanding the mechanism of injury and computed tomography facilitates the early diagnosis of bilateral posterior fracture-dislocation of the shoulder caused by an electric shock.
Dr. Sanshiro Yasuma, Department of Orthopaedic Surgery, Nagoya City University East Medical Center, Nagoya, Japan. E-mail: 5mu9ph@bma.biglobe.ne.jp
Introduction: Bilateral posterior fracture-dislocation of the shoulder is a very rare injury that is commonly missed. Almost 70% of bilateral posterior dislocations are due to convulsive seizures, with electric shocks accounting for < 5% of bilateral posterior shoulder dislocations.
Case Report: The case of a walk-in patient, a 52-year-old man, with bilateral posterior fracture-dislocation of the shoulder caused by an electric shock is reported. Although he was initially admitted to the emergency department for observation of the potential complications of an electric shock, such as fatal arrhythmia and rhabdomyolysis, he subsequently consulted an orthopedic surgeon 4 days after the event due to persistent bilateral shoulder pain and was diagnosed using X-ray and computed tomography with bilateral posterior fracture-dislocation of the shoulder. Following open reduction and internal fixation 7 days after the injury, the upper limbs were fixed with shoulder braces at a slightly flexed and abducted position with neutral rotation for 3 weeks postoperatively followed by range of motion exercises. Twelve months after surgery, he had a Constant shoulder score of 94, an American Shoulder and Elbow Surgeon score of 100, and no shoulder re-dislocation or humeral head necrosis.
Conclusion: In this walk-in patient, the diagnosis of bilateral posterior fracture-dislocation of the shoulder caused by an electric shock was delayed. We believe that understanding the mechanism of this type of injury will facilitate its early diagnosis.
Keywords: Bilateral, electric shock, posterior fracture-dislocation, shoulder.
Bilateral posterior shoulder dislocation is a rare injury first reported by Mynter, in 1902 [1]. Brackstone et al. described the major causes of bilateral posterior shoulder dislocation as the triple “E” syndrome, which includes epileptic seizures, extreme trauma, and electric shock [2], since epileptic seizures and electric shocks account for about 70% and 5% of the causes of this injury, respectively [3]. Proper imaging is mandatory for correct diagnosis, since this injury is often not diagnosed or is misdiagnosed in up to 80% of cases [4,5]. Although several previous reports presented cases of bilateral posterior dislocation of the shoulder caused by an electric shock [6-9], there have been no previous case reports of bilateral posterior fracture-dislocation caused by an electric shock that required open reduction and internal fixation (ORIF). A case of delayed diagnosis of bilateral posterior fracture-dislocation of the shoulder secondary to an electric injury is reported.
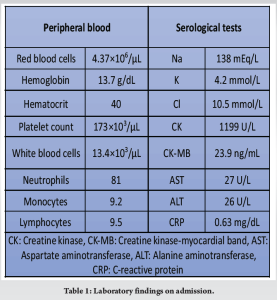
A 52-year-old man presented with pain in the upper limbs and shoulders after accidental contact with a high-voltage electric current while in the crouching position while working. Immediately after the injury, he was unable to actively move his fingers. He walked to the emergency department. On arrival, his level of consciousness was normal, and he had no complaints other than pain in both upper limbs. Physical examination showed subcutaneous hemorrhages in the proximal regions of both upper arms, implying that the electric current had extended to both upper limbs. Chest X-ray showed no abnormal findings, although the shoulder joints were not included in the imaging area. Laboratory findings showed a normal electrocardiogram and slight elevation of white blood cells and creatine kinase, but no evidence of myoglobinuria, ruling out fatal arrhythmia and rhabdomyolysis caused by the electric shock (Table 1).
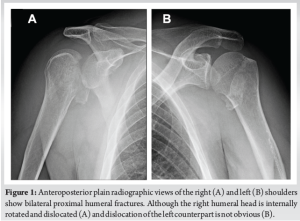
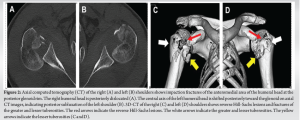
Although he was initially admitted to the emergency department for follow-up observation of the possible complications mentioned above due to electric shock, he did not develop these complications during his 41-day hospitalization. However, since he experienced limited range of motion of both shoulder joints due to persistent pain, he consulted an orthopedic surgeon on the 4th day after the event. Imaging examinations were performed on the same day. Plain anteroposterior radiographs of the shoulders showed bilateral proximal humeral fractures (Fig. 1). Subsequent review of computed tomography (CT) scans confirmed the diagnosis of bilateral four-part proximal humeral fractures according to the Neer classification with reverse Hill-Sachs lesions, along with posterior dislocation of the right shoulder joint and posterior subluxation of its left counterpart (Fig. 2). Magnetic resonance imaging showed edematous changes in bilateral deltoid and right triceps muscles and fluid accumulation around the insertion point of the left supraspinatus muscle.
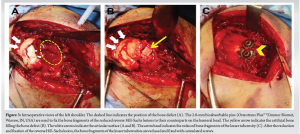
Although closed reductions of the posterior shoulder dislocations were performed under sedation, the right greater and lesser tuberosity fracture was still displaced, and the left shoulder was easily subluxated. Therefore, ORIF was performed 7 days after the injury to prevent re-dislocation, since the presence of reverse Hill-Sachs lesions with defects affecting more than 25% of the articular surface of the humeral head and a highly active person under the age of 65 years are risk factors for re-dislocation [1,4]. Under general anesthesia, the deltopectoral approach was used bilaterally to expose both shoulders. Intraoperatively, the bone fragments of the reverse Hill-Sachs lesions were found to be depressed internally, and fractures of the greater and lesser tuberosities were observed. The bone fragments of the reverse Hill-Sachs lesion were elevated and reduced by lifting the subchondral bone with a chisel. Subsequently, 2.0-mm bioabsorbable pins (Osteotrans Plus™ ®Zimmer Biomet, Warsaw, IN, USA) were used to fix the bone fragments of the reduced reverse Hill-Sachs lesions to their counterparts on the humeral head (Fig. 3a). The bone defect under the subchondral bone was filled with artificial bone (Bonish bone graft substitute®, Depuy Synthes, Westchester, PA, USA) to support the bone fragments (Fig. 3b). All bone fragments were fixed using 5.0-mm cannulated screws (ACE TiMAX Large Fragment System™ ®Zimmer Biomet), along with a plate with three distal screw holes for the right proximal humerus (PHILOS® System, Depuy Synthes, Raynham, MA, USA). Screw washers were used to prevent further crushing of the femoral head bone fragment (Fig. 3c). Intraoperative examination of the soft tissue showed no rotator cuff injuries and no other tendon or muscle rupture.
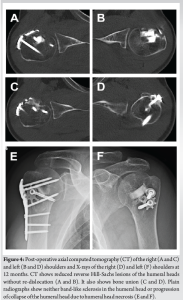
Shoulder braces were attached to both upper extremities, and both shoulder joints were fixed at a slightly flexed and abducted position with neutral rotation for 3 weeks postoperatively. Subsequently, active range of motion exercises of the shoulder joint, except external rotation, was started, followed by removing the restriction of the range of motion from 6 weeks after the operation. The patient’s post-operative course was evaluated using the Constant shoulder score [10] and the American Shoulder and Elbow Surgeons (ASES) score [11] 6 and 12 months after surgery. Both scores are the ones most commonly used for evaluating function of the shoulder joint; they are graded out of 100 points, and the higher the score, the better the function [12]. The patient’s Constant shoulder score and ASES score were 58 and 64 points, respectively, 6 months after surgery, and 94 and 100 points, respectively, 12 months after surgery. The domains of pain, muscle strength, and movement improved markedly from 6 to 12 months after surgery. The range of motion of both shoulder joints improved from 120° to 170° in flexion, from 95° to 120° in abduction, from 60° to 80° in external rotation, and from L3 to Th12 in internal rotation. He returned fully to work 6 months after surgery. There was no restriction in his ability to work, and neither humeral head necrosis nor re-dislocation was observed 12 months after surgery. Plain radiographs did not show any signs of humeral head necrosis, such as band-like sclerosis or progression of humeral head collapse 12 months after surgery. CT showed bone union in good overall alignment without re-dislocation of the humeral heads or loosening of the fixation implants 12 months after surgery (Fig. 4).
The mechanism of posterior fracture-dislocation of the shoulder during a convulsive seizure has been well described [13]. The typical position of the shoulder during a convulsion is adduction, internal rotation, and flexion. With the strong muscular spasm, the humeral head is forced superiorly and posteriorly over the glenoid cavity. Impression fractures of the anteromedial humeral head, which are also called reverse Hill-Sachs lesions, have been reported to occur in 40–90% of patients with an initial dislocation [14]. Further, convulsive force, with the humeral head impinged against the glenoid rim, eventually results in a complex proximal humeral fracture. The present patient was injured while doing electrical work in the crouching and bending forward position. The electric shock caused severe muscle contraction around the shoulder joint. It is speculated that the fracture-dislocation occurred by the same mechanism as in epileptic seizures. Posterior dislocation of the shoulder is an uncommon injury that accounts for 4% of all shoulder dislocations [2]. Its diagnosis is difficult and often missed due to its rarity. Imaging of the shoulder in cases of suspected fracture-dislocation should include an axillary or transthoracic view. Since the arm will usually be immobilized in internal rotation at the time of X-ray examination, overlapping of the humeral head and the glenoid fossa might mimic the normal overlapping seen with the shoulder in full internal rotation. However, it should be noted that axillary views might be difficult to obtain if the patient is experiencing acute pain and is only capable of limited abduction of the shoulders. CT is very useful for confirming dislocation and assessing fracture location. In the present patient, CT confirmed the diagnosis without the need for axillary X-ray views, although it was delayed because the injury was not suspected at the first visit. Once diagnosed, management of this injury must be individualized depending on the patient’s age, the amount of damage to the humeral head, the time from injury, and the level of activity [15]. Defects of the articular surface of the humeral head of up to 25% in patients with dislocations < 3 weeks old can be treated by closed reduction and immobilization in external rotation; however, for chronic dislocations (older than 3 weeks), closed reduction is highly unsuccessful [16]. Defects of more than 50% of the articular surface should be treated with shoulder arthroplasty [17]. Management of defects of between 25% and 50% of the articular surface, such as by open reduction with concomitant bone defect augmentation, is even more challenging. Rezazadeh and Vosoughi described an algorithm for the management of acute posterior shoulder dislocation in young patients [9]. In older patients (> 65 years old) with complex fracture patterns, there is a high risk of avascular necrosis. Francis et al. described their performance of reverse total shoulder arthroplasty in cases in which ORIF was not feasible [18]. In the present case, the bone defect due to the reverse Hill-Sachs lesions involved 40% and 25% of the articular surfaces of the humeral heads on the right and left sides, respectively. ORIF with concomitant bone defect augmentation was performed to prevent re-dislocation of the shoulders, and because the patient was under the age of 65 years and was engaged in an active occupation. In the current patient, no humeral head collapse or arthritis was observed at the last follow-up; the fractures had healed completely, and there was no recurrent instability in either shoulder.
The diagnosis of bilateral posterior fracture-dislocation of the shoulder caused by an electric shock was delayed in the present walk-in patient. We believe that understanding the mechanism of injury due to an electric shock and CT will facilitate its early diagnosis.
It is essential to suspect posterior fracture-dislocation of the shoulder in patients with shoulder joint pain caused by electric shock. CT is useful for emergency physicians to prevent missing the diagnosis, as well as to diagnose it early, even if they lack specialized knowledge of the orthopedic field. Once diagnosed, prompt consultation with orthopedic surgeons followed by the optimal treatment contributes to improved clinical outcomes of the injury.
References
- 1.Mynter H. XIV. Subacromial dislocation from muscular spasm. Ann Surg 1902;36:117-9. [Google Scholar | PubMed]
- 2.Brackstone M, Patterson SD, Kertesz A. Triple “E” syndrome: Bilateral locked posterior fracture dislocation of the shoulders. Neurology 2001;56:1403-4. [Google Scholar | PubMed]
- 3.Huizing JW, Monteban PE. Bilateral posterior fracture dislocation of the shoulders: Review of case reports and treatment. Acta Orthop Belg 2020;86:193-9. [Google Scholar | PubMed]
- 4.Rowe CR, Zarins B. Chronic unreduced dislocations of the shoulder. J Bone Joint Surg Am 1982;64:494-505. [Google Scholar | PubMed]
- 5.Hawkins RJ, Neer CS 2nd, Pianta RM, Mendoza FX. Locked posterior dislocation of the shoulder. J Bone Joint Surg Am 1987;69:9-18. [Google Scholar | PubMed]
- 6.Ketenci IE, Duymus TM, Ulusoy A, Yanik HS, Mutlu S, Durakbasa MO. Bilateral posterior shoulder dislocation after electrical shock: A case report. Ann Med Surg (Lond) 2015;4:417-21. [Google Scholar | PubMed]
- 7.Kechagias VA, Katounis CA, Badras SL, Notaras I, Badras LS. Bilateral posterior fracture-dislocation of the shoulder after electrical shock treated with bilateral hemiarthroplasty: A case report. Malays Orthop J 2022;16:146-9. [Google Scholar | PubMed]
- 8.Claro R, Sousa R, Massada M, Ramos J, Lourenço JM. Bilateral posterior fracture-dislocation of the shoulder: Report of two cases. Int J Shoulder Surg 2009;3:41-5. [Google Scholar | PubMed]
- 9.Rezazadeh S, Vosoughi AR. Closed reduction of bilateral posterior shoulder dislocation with medium impression defect of the humeral head: A case report and review of its treatment. Case Rep Med 2011;2011:124581. [Google Scholar | PubMed]
- 10.Constant CR, Gerber C, Emery RJ, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: Modifications and guidelines for its use. J Shoulder Elbow Surg 2008;17:355-61. [Google Scholar | PubMed]
- 11.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg 1994;3:347-52. [Google Scholar | PubMed]
- 12.Ashton ML, Savage-Elliott I, Granruth C, O’Brien MJ. What are we measuring? A systematic review of outcome measurements used in shoulder surgery. Arthrosc Sports Med Rehabil 2020;2:e429-34. [Google Scholar | PubMed]
- 13.Shaw JL. Bilateral posterior fracture-dislocation of the shoulder and other trauma caused by convulsive seizures. J Bone Joint Surg Am 1971;53:1437-40. [Google Scholar | PubMed]
- 14.Basal O, Dincer R, Turk B. Locked posterior dislocation of the shoulder: A systematic review. EFORT Open Rev 2018;3:15-23. [Google Scholar | PubMed]
- 15.Iosifidis MI, Giannoulis I, Traios S, Giantsis G. Simultaneous bilateral posterior dislocation of the shoulder: Diagnostic problems and management. A case report. Knee Surg Sports Traumatol Arthrosc 2006;14:766-70. [Google Scholar | PubMed]
- 16.Cicak N. Posterior dislocation of the shoulder. J Bone Joint Surg Br 2004;86:324-32. [Google Scholar | PubMed]
- 17.Page AE, Meinhard BP, Schulz E, Toledano B. Bilateral posterior fracture-dislocation of the shoulders: Management by bilateral shoulder hemiarthroplasties. J Orthop Trauma 1995;9:526-9. [Google Scholar | PubMed]
- 18.Francis AO, Kelly MJ, Flannery OM. Bilateral posterior fracture dislocations of the shoulder treated with bilateral reverse total shoulder arthroplasty. Ann Case Rep 2020;14:316. [Google Scholar | PubMed]