The congruent arc modification enhances glenoid arc restoration and graft contact area, enabling improved stability and predictable outcomes in patients with significant glenoid bone loss undergoing the Latarjet procedure.
Dr. Sumit Kaushik, Department of Orthopaedics, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, 751024, India. Email: iamdrmeet@gmail.com
Introduction: Recurrent anterior shoulder instability with significant glenoid bone loss is associated with high failure after isolated soft-tissue repair. The open Latarjet procedure with congruent arc modification improves graft coverage and glenoid arc restoration, but mid-term clinical data are limited.
Materials and Methods: This retrospective cohort included patients who underwent open Latarjet with congruent arc modification between January 2015 and December 2020. Eligibility criteria were ≥3 anterior dislocations, ≥15% glenoid bone loss, and ≥24 months of follow-up. Functional outcomes (Western Ontario Shoulder Instability Index [WOSI], Rowe), range of motion, complications, and graft union on computed tomography (CT) were assessed. Kaplan–Meier survival analysis estimated recurrence-free survival.
Results: A total of 80 patients (62 males, 18 females; mean age 28.5 ± 6.4 years) were analyzed with a mean follow-up of 4.5 ± 1.2 years. WOSI improved from 46.7 ± 12.3 to 79.4 ± 15.8 (P < 0.001), and Rowe from 32.5 ± 9.6 to 85.6 ± 10.7 (P < 0.001), both exceeding minimal clinically important difference thresholds. Forward flexion (+15°) and abduction (+20°) improved significantly, whereas external rotation showed a mild, non-significant reduction (–10°, P = 0.079). Complications occurred in 12.5%, mainly graft non-union (5%). CT confirmed graft union in 95%. Kaplan–Meier analysis showed 97.5% recurrence-free survival at 5 years.
Conclusion: Open Latarjet with congruent arc modification provides clinically meaningful functional improvement, reliable graft union, and durable mid-term stability in recurrent anterior instability with glenoid bone loss.
Keywords: Latarjet, congruent arc, shoulder instability, glenoid bone loss, functional outcomes.
Recurrent anterior shoulder instability in young, active patients is frequently associated with glenoid bone loss, particularly when it exceeds 15% of the inferior glenoid diameter. In such cases, isolated soft-tissue repair carries a high risk of failure [1,2]. The Latarjet procedure addresses this by transferring the coracoid to the glenoid rim, offering both bony augmentation and dynamic stability through the conjoint tendon [3].
The congruent arc modification rotates the coracoid by 90° to increase articular arc coverage and surface contact, potentially enhancing stability and reducing graft-related complications [4,5,6]. Although biomechanical advantages have been demonstrated, clinical outcome evidence at mid-term follow-up remains scarce. Furthermore, most available studies are limited by small sample sizes or heterogeneous populations, and data from Asian centers are particularly sparse. The present study aimed to evaluate functional outcomes, range of motion, complications, and graft survival following open Latarjet with congruent arc modification in patients with recurrent anterior shoulder instability and significant glenoid bone loss. We hypothesized that this technique would yield clinically meaningful improvements in validated outcome scores, high graft union rates, and low recurrence.
This retrospective cohort study was conducted at a tertiary orthopedic center. Ethical approval for this study was obtained from the Institutional Ethical Committee (No-KIIT/KIMS/IEC/1038/2022 on February 22, 2022). The study complied with the Declaration of Helsinki principles.
Patient selection
Patients who underwent open Latarjet with congruent arc modification between January 2015 and December 2020 were identified from the institutional surgical registry. Inclusion criteria were:
- ≥3 documented anterior shoulder dislocations,
- Pre-operative CT or MRI confirming ≥15% glenoid bone loss using the best-fit circle method,
- Open Latarjet procedure performed with a congruent arc modification, and
- Minimum clinical follow-up of 24 months.
Exclusion criteria included multidirectional or posterior instability, massive irreparable rotator cuff tears, prior bony stabilization procedures, active infection, or incomplete follow-up. Of 112 screened patients, 80 met all eligibility criteria.
Surgical technique
All procedures were performed by three fellowship-trained shoulder surgeons using a standardized deltopectoral approach. The coracoid process was osteotomized, rotated 90° (congruent arc orientation), and fixed flush with the glenoid rim using two 4.0-mm partially threaded screws.
Post-operative rehabilitation
A four-phase standardized rehabilitation protocol was followed:
- Phase I (0–6 weeks): Immobilization in a sling with passive range-of-motion exercises
- Phase II (6–12 weeks): Active-assisted motion and progressive strengthening
- Phase III (3–6 months): Advanced strengthening and sport-specific drills
- Phase IV (≥6 months): Return to contact sports, provided pain-free symmetric motion was restored.
Outcome measures
The primary outcomes were functional scores:
- Western Ontario Shoulder Instability Index (WOSI; normalized 0–100, higher = better),
- Rowe score (0–100, higher = better).
Secondary outcomes included range of motion (forward flexion, abduction, and external rotation), complications (graft non-union, malposition, recurrence, neurologic symptoms, reoperation, infection, and hardware issues), and graft union assessed on post-operative CT scans.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD). Pre- and post-operative comparisons were performed using paired t-tests. Mean differences were reported with 95% confidence intervals (CI) and effect sizes (Cohen’s d). Statistical significance was set at P < 0.05. Minimal clinically important difference (MCID) thresholds were applied for interpretation (14 for WOSI, 9.7 for Rowe). Kaplan–Meier survival analysis was performed to estimate recurrence-free survival.
Patient demographics
A total of 80 patients (62 males and 18 females) with a mean age of 28.5 ± 6.4 years were included (Fig. 1).
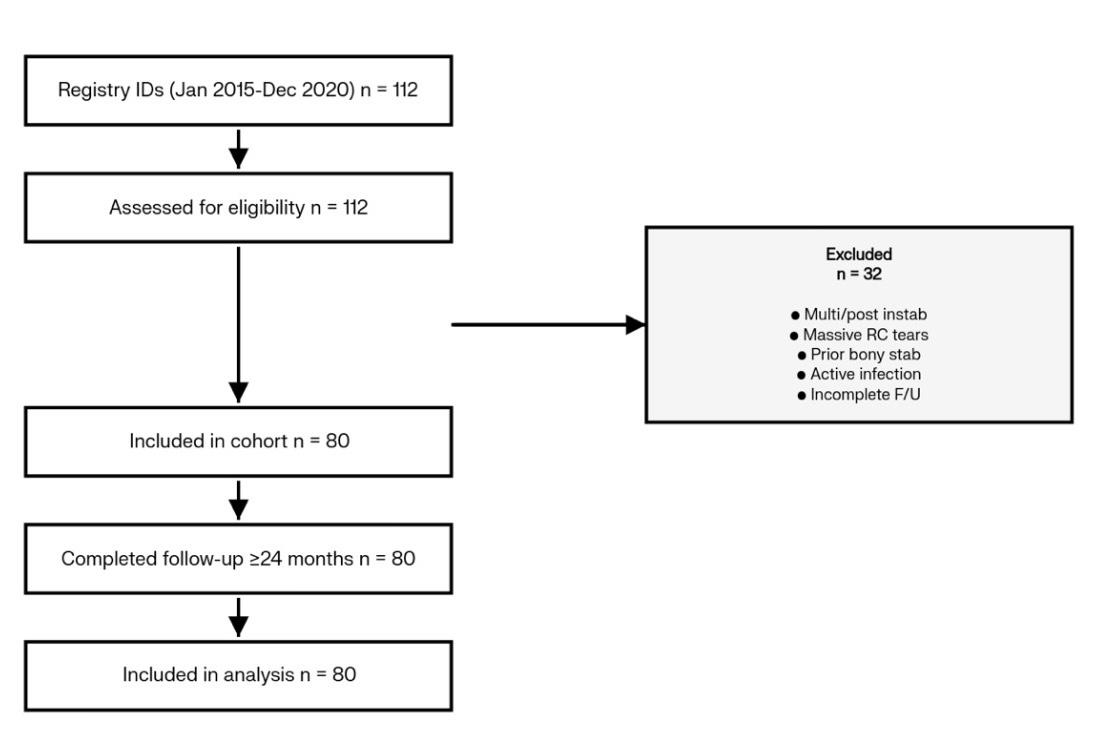
Figure 1: Patient flow diagram (STROBE).
The mean follow-up was 4.5 ± 1.2 years (range, 2.1–7.0 years). Of these, 51 patients (63.7%) were competitive or recreational contact-sport athletes, and 16 (20.0%) had failed prior arthroscopic stabilization. Functional outcomes, both primary outcome measures, improved significantly (Table 1 and Fig. 2).
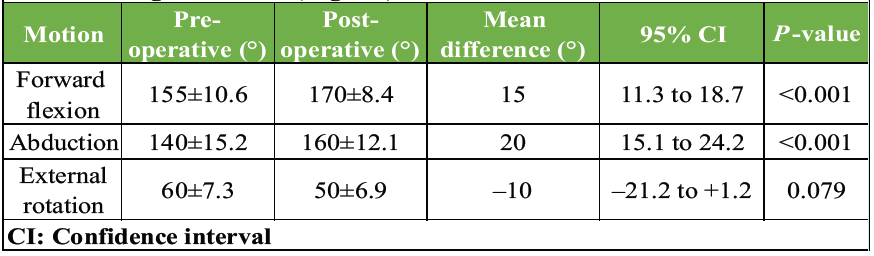
Table 1: Range of motion (degrees)
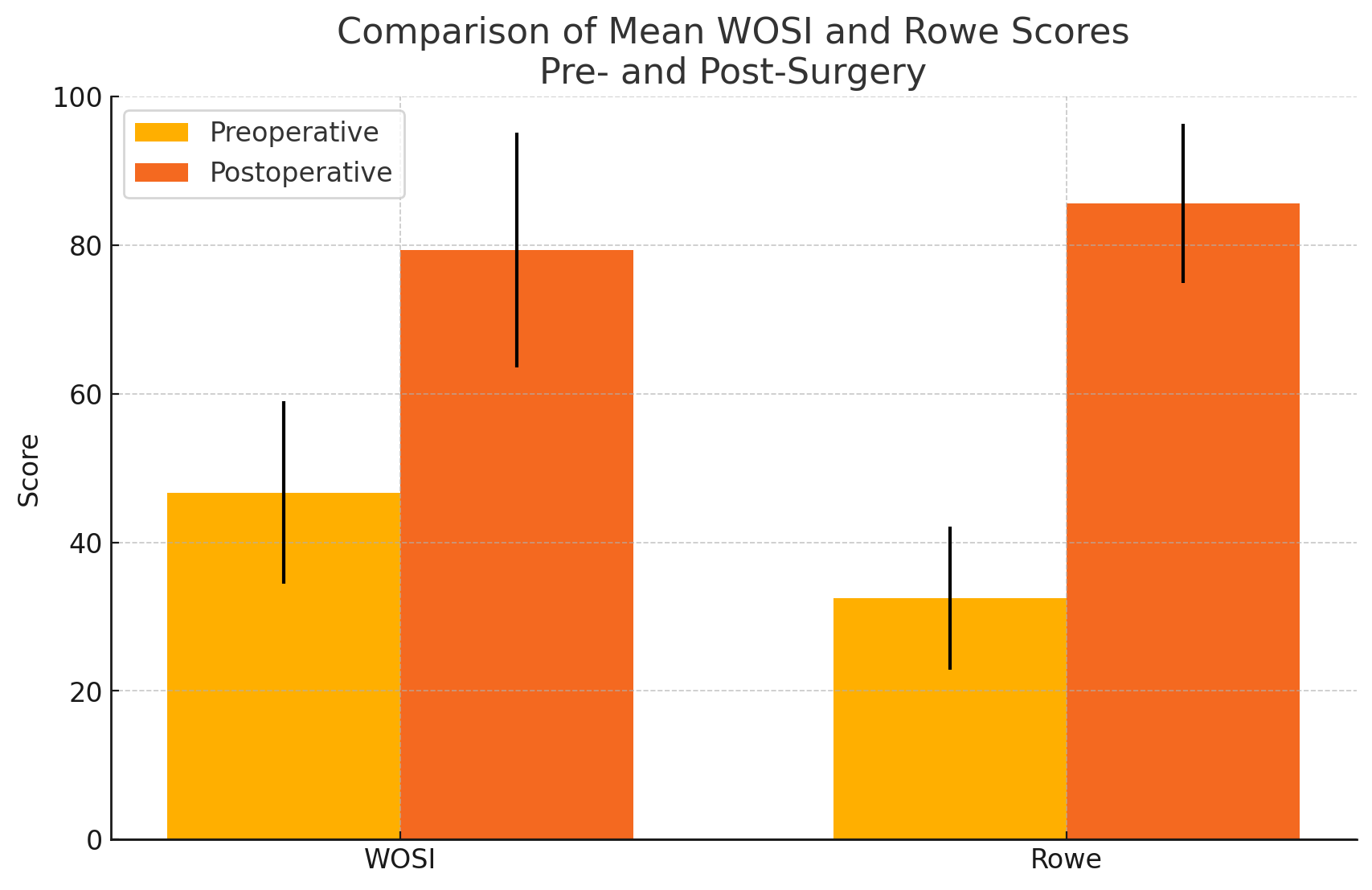
Figure 2: Bar graph comparing pre- and post-operative Western Ontario Shoulder Instability Index and Rowe scores.
- WOSI score improved from 46.7 ± 12.3 to 79.4 ± 15.8, with a mean difference of +32.7 (95% CI, 28.9–36.5; P < 0.001; d = 1.89).
- Rowe’s score improved from 32.5 ± 9.6 to 85.6 ± 10.7, with a mean difference of +53.1 (95% CI, 49.8–56.3; P < 0.001; d = 3.58).
- Both exceeded the established MCID thresholds.
Range of motion
Post-operative forward flexion and abduction improved significantly, whereas external rotation showed a mild, non-significant reduction (Table 1).
- Forward flexion: 155° ± 10.6 to 170° ± 8.4; mean difference +15° (95% CI, 11.3–18.7; P < 0.001).
- Abduction: 140° ± 15.2 to 160° ± 12.1; mean difference +20° (95% CI, 15.1–24.2; P < 0.001).
- External rotation: 60° ± 7.3 to 50° ± 6.9; mean difference –10° (95% CI, –21.2 to +1.2; P = 0.079).
Complications
Complications were observed in 10 patients (12.5%):
- Graft non-union: 4 patients (5.0%)
- Transient axillary nerve symptoms: 3 patients (3.8%),
- Recurrent instability: 2 patients (2.5%),
- Graft malposition: 1 patient (1.3%).
No infections, hardware failures, or reoperations were recorded during follow-up.
Graft union and survival
CT evaluation confirmed graft union in 76 patients (95.0%). Kaplan–Meier survival analysis demonstrated a 97.5% recurrence-free survival at 5 years (95% CI, 91.2–99.4%) (Fig. 3).
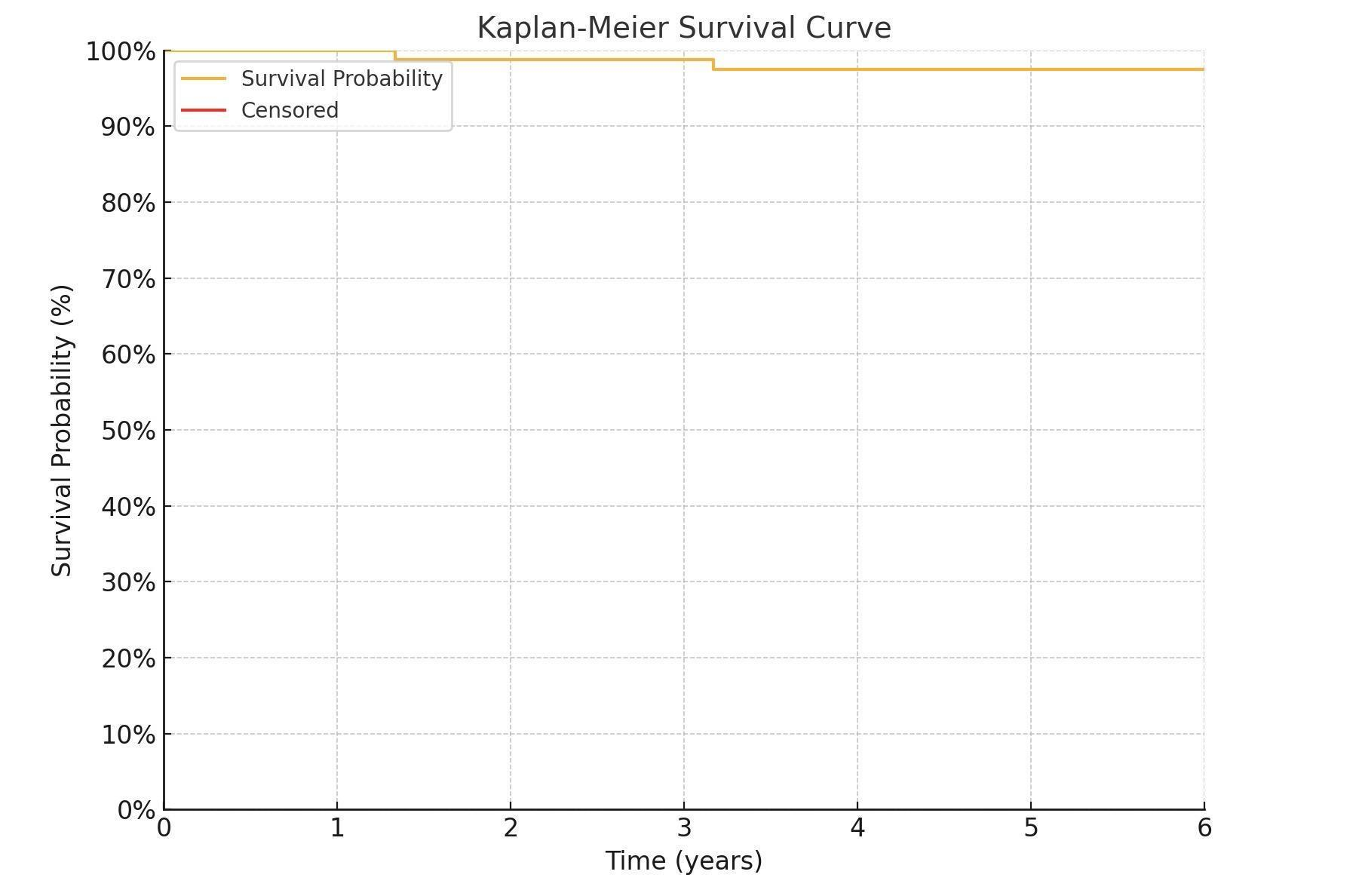
Figure 3: Kaplan-Meier survival curve illustrating time to instability recurrence.
This study demonstrates that the open Latarjet procedure with congruent arc modification results in substantial functional gains and reliable stability at mid-term follow-up. Both WOSI and Rowe scores improved well beyond established MCID thresholds, confirming the clinical significance of these outcomes.
Our findings support earlier reports of the congruent arc modification. De Beer and Roberts first described the technique, highlighting improved graft coverage [4], while subsequent biomechanical studies confirmed its superiority in restoring glenoid arc width compared with the traditional orientation [5,6,7,8,9,10]. In our series, Rowe improved by +53 points and WOSI by +33 points, comparable to or exceeding earlier clinical cohorts [11,12]. The complication rate of 12.5% aligns with systematic reviews, which report pooled rates between 10 and 15% [13,14].
Recent studies further validate these outcomes in the Indian context. A prospective cohort reported Rowe improving from 42.16 ± 7.26 to 97.0 ± 8.45 with high patient satisfaction [19], while a multicenter evaluation of open congruent arc Latarjet in low-resource hospitals (n = 40) demonstrated Rowe improving from 23.05 to 91.10 and ASES from 22.95 to 75.65, with no redislocations at 24 months [20]. These results are consistent with our low redislocation rate (2.5%) and excellent 5-year recurrence-free survival (97.5%). Meta-analyses comparing open and arthroscopic Latarjet procedures also show broadly similar WOSI and Rowe outcomes [13,17], suggesting that the favorable results in our cohort reflect the construct itself rather than the surgical approach.
Loss of external rotation, though mild and not statistically significant in our series, remains a recognized concern. Some reports describe measurable deficits [15], while others suggest minimal functional impact [16]. In our cohort, the reduction was small and outweighed by the stability benefits. Graft-related complications, mainly non-union, accounted for most adverse events. Our non-union rate (5%) was lower than some previous reports [14,17], possibly due to standardized surgical technique and structured rehabilitation. Transient neurologic symptoms were in line with published data [18], and no hardware failures or reoperations occurred.
The strengths of this study include a relatively large cohort, standardized surgical technique performed by fellowship-trained surgeons, and the use of validated scoring systems.
Limitations
This retrospective, single-center, non-randomized study with a modest sample size may introduce selection bias and limit generalizability. The absence of a control group and heterogeneity in surgeon experience may have influenced outcomes. Mid-term follow-up restricts long-term assessment, and radiological evaluation was non-uniform with limited dynamic imaging. Patient-reported scores, incomplete return-to-sport data, and potential loss to follow-up may affect interpretation. Cost-effectiveness and subclinical complications were not assessed, external validity is limited by the young active cohort, and learning-curve effects were not evaluated.
In summary, the open congruent arc Latarjet provides reliable mid-term stability, high graft union, and excellent functional recovery in recurrent anterior instability with glenoid bone loss. While mild external rotation loss may occur, recurrence rates remain low. Future prospective and comparative studies with long-term follow-up are warranted to further define its role relative to classic and arthroscopic techniques.
The open Latarjet procedure with congruent arc modification provides excellent functional outcomes, durable stability, and low recurrence at mid-term follow-up in recurrent anterior shoulder instability with glenoid bone loss.
The congruent arc Latarjet provides reliable stability and clinically meaningful functional improvement for recurrent anterior shoulder instability with glenoid bone loss, with high graft-union rates and acceptable complication rates at mid-term follow-up.
References
- 1. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Google Scholar] [PubMed]
- 2. Bessière C, Trojani C, Carles M, Mehta SS, Boileau P. The open Latarjet procedure is more reliable in terms of shoulder stability than arthroscopic Bankart repair. Clin Orthop Relat Res 2014;472:2345-51. [Google Scholar] [PubMed]
- 3. Latarjet M. Technique of coracoid graft for treatment of recurrent dislocation of the shoulder. Lyon Chir 1954;49:994-7. [Google Scholar] [PubMed]
- 4. de Beer JF, Roberts C. Glenoid bone defects–open Latarjet with congruent arc modification. Orthop Clin North Am 2010;41:407-15. [Google Scholar] [PubMed]
- 5. Hovelius L, Sandström B, Sundgren K, Saebö M. The congruent-arc Latarjet technique: Technical note. Shoulder Elbow 2014;6:177-80. [Google Scholar] [PubMed]
- 6. Giles JW, Boons HW, Elkinson I, Faber KJ, Ferreira LM, Johnson JA, et al. Anterior shoulder instability: Biomechanical evaluation of bone block procedures. J Bone Joint Surg Am 2013;95:1161-7. [Google Scholar] [PubMed]
- 7. Moroder P, Hirschmann MT, Danzinger V, Huber J, Tauber M. Three-dimensional planning and navigation in Latarjet surgery. J Shoulder Elbow Surg 2016;25:1133-40. [Google Scholar] [PubMed]
- 8. Dumont GD, Fogerty S, Rosso C, Lafosse L. Arthroscopic Latarjet: Imaging, indications, and technique. Arthroscopy 2014;30:1116-23. [Google Scholar] [PubMed]
- 9. de Beer JF, Roberts C, Bhatia DN. Congruent arc Latarjet procedure: Technical aspects and outcome. Tech Shoulder Elbow Surg 2010;11:45-53. [Google Scholar] [PubMed]
- 10. Ghodadra NS, Gupta A, Romeo AA, Bach BR Jr., Verma NN, Shewman EF, et al. The importance of the congruent-arc modification in coracoid transfer procedures. Am J Sports Med 2010;38:1918-24. [Google Scholar] [PubMed]
- 11. Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JJ. Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 2012;94:495-501. [Google Scholar] [PubMed]
- 12. Lafosse L, Lejeune E, Bouchard A, Kakuda C, Gobezie R, Kochhar T. Arthroscopic Latarjet procedure. Orthop Clin North Am 2010;41:393-405. [Google Scholar] [PubMed]
- 13. Hurley ET, Lim Fat D, Farrington SK, Mullett H. Systematic review of the Latarjet procedure in athletes. Am J Sports Med 2019;47:2593-600. [Google Scholar] [PubMed]
- 14. Cowling PD, Akhtar MA, Liow RY. Complications following the Latarjet procedure. Bone Joint J 2019;101-B:627-34. [Google Scholar] [PubMed]
- 15. Mizuno N, Denard PJ, Raiss P, Melis B, Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 2014;23:1691-9. [Google Scholar] [PubMed]
- 16. Young AA, Maia R, Berhouet J, Walch G. Open Latarjet procedure for management of bone loss in anterior instability of the glenohumeral joint. Am J Sports Med 2011;39:2106-13. [Google Scholar] [PubMed]
- 17. Frank RM, Romeo AA, Provencher MT. Outcomes after Latarjet procedure: A systematic review. Arthroscopy 2014;30:1185-90. [Google Scholar] [PubMed]
- 18. Hovelius L, Sandström B, Olofsson A, Svensson O, Rahme H. Complications and long-term outcomes of the Bristow-Latarjet procedure: A prospective study with 15–20 years of follow-up. Clin Orthop Relat Res 1983;175:35-42. [Google Scholar] [PubMed]
- 19. Sharma A, Gupta V, Singh S, Arora S, Singh D. Functional outcomes of open Latarjet procedure in recurrent anterior shoulder instability: A prospective Indian cohort. Indian J Orthop 2020;54:285-91. [Google Scholar] [PubMed]
- 20. Reddy R, Iyer S, Menon J, Krishnan SG, Sinha S, Sharma A, et al. Multicenter evaluation of congruent arc Latarjet in low-resource tertiary hospitals in India. J Clin Orthop Trauma 2021;17:120-6. [Google Scholar] [PubMed]
- 21. Hurley ET, Montgomery C, Jamal MS, Shimozono Y, Ali Z, Pauzenberger L, et al. Open versus arthroscopic Latarjet procedure: A systematic review and meta-analysis. Am J Sports Med 2019;47:1248-53. [Google Scholar] [PubMed]