Giant cell tumor evolving into aneurysmal bone cyst of small bones of hand and feet is a rare presentation and can be treated by excision of the lesion.
Dr. R V Raghav,
Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
E-mail: raghavravi2193@gmail.com
Introduction: Giant cell tumor (GCT) most commonly involves distal femoral condyles, distal end of radius, proximal tibial plateau, and proximal humerus. GCT is uncommon to occur in small bones of hand and feet. 2% of GCT occur in hand. The incidence of GCT in foot is 1.2–1.8%. Only a few cases have been reported in literature worldwide. GCT is the most common cause of secondary ABC. We report a case of GCT of intermediate cuneiform in a 25-year-old female evolving into aneurysmal bone cyst (ABC).
Case Report: A 25-year-old female presented to us with complaints of pain and swelling over the dorsum of right foot for a period of 1 year. On examination, there was a localized ovoid-shaped swelling of 2 by 2 cm over the dorsum of right foot. Radiographs revealed a well-defined osteolytic lesion in the intermediate cuneiform. T2 MRI showed hyper-intense lesion in intermediate cuneiform. The patient was taken up for surgery, and the intermediate cuneiform was excised completely. Removed bone was sent for histopathological examination which confirmed it to be GCT evolving into secondary ABC. The patient was followed for 1 year and had no complaints. The patient was able to weight bear and walk without any difficulty. There was no recurrence of lesion.
Conclusion: GCT of the cuneiform evolving into ABC is a very rare presentation. The treatment of choice is excision of the tumor with or without bone grafting. Any osteolytic lesion in the small bones must be evaluated and should be intervened in the early stage.
Keywords: Giant cell tumor, osteolytic lesion, surgical resection, intermediate cuneiform.
Giant cell tumor (GCT) of bone was first described by Turcotte in the year 1818 [1]. The percentage distribution of GCTs is 4–5% and that of aneurysmal bone cyst (ABC) is 5–6%. ABC was first described by Jaffe and Lichtenstein in the year 1942 [2]. GCT occurs mostly in skeletally mature individuals and it is epiphyseal in location. In some scenarios, metaphyseal extension is seen. It has a higher incidence in females and occurs mostly in the 3rd or 4th decade. The occurrence of GCT in hand and foot is a rare presentation. ABC occurs mostly in young individuals in the first two decades which are metaphyseal in location. GCT of cuneiform is rare to occur, and very few cases have been reported in literature. GCT evolving into ABC is common in spine and long bones [3] but rare to occur in the hand and foot [4]. There is no documented evidence of a GCT in the intermediate cuneiform. In this case report, we are discussing a case of intermediate cuneiform GCT evolving into ABC which was managed by complete excision of the intermediate cuneiform.
A 25-year-old female presented to our patient clinic with complaints of pain and swelling over the dorsum of her right foot for a period of 1 year. Swelling was insidious in onset, gradually progressive and reached the present size. Pain was insidious in onset, intermittent, moderate intensity, dull aching, no radiation, aggravated by walking, and relieved with medications. There is no history of fever, trauma, loss of weight, and loss of appetite. The patient had no other medical comorbidities.
On examination, there was a localized ovoid-shaped swelling of 2 by 2 cm over the dorsum of right foot, 7–8 cm in front of medial malleolus, and 5 cm behind the base of 2nd toe. Surface appeared to be smooth. Edge of the swelling was clearly defined. There was no hyperpigmentation of skin. On palpation, there was no warmth and tenderness was present. Swelling had well-defined margins, non-mobile, and hard in consistency. Skin over the swelling was pinchable. There was no enlargement of any regional lymph node. 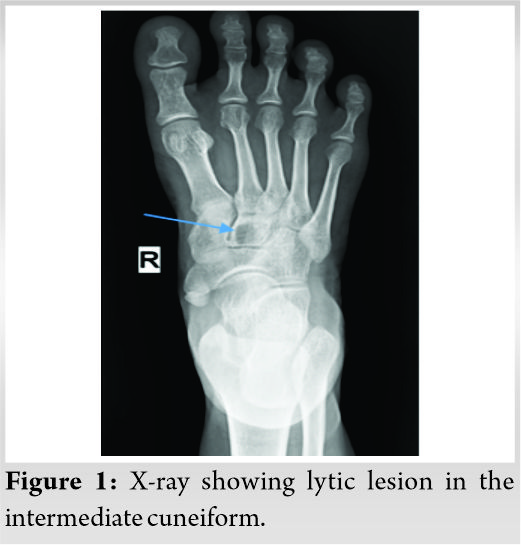 X-ray of right foot AP and oblique (Fig. 1) was done which revealed well-defined osteolytic lesion in the center of the intermediate cuneiform, geographic pattern of destruction, narrow zone of transition, and not breaching the cortex.
X-ray of right foot AP and oblique (Fig. 1) was done which revealed well-defined osteolytic lesion in the center of the intermediate cuneiform, geographic pattern of destruction, narrow zone of transition, and not breaching the cortex. 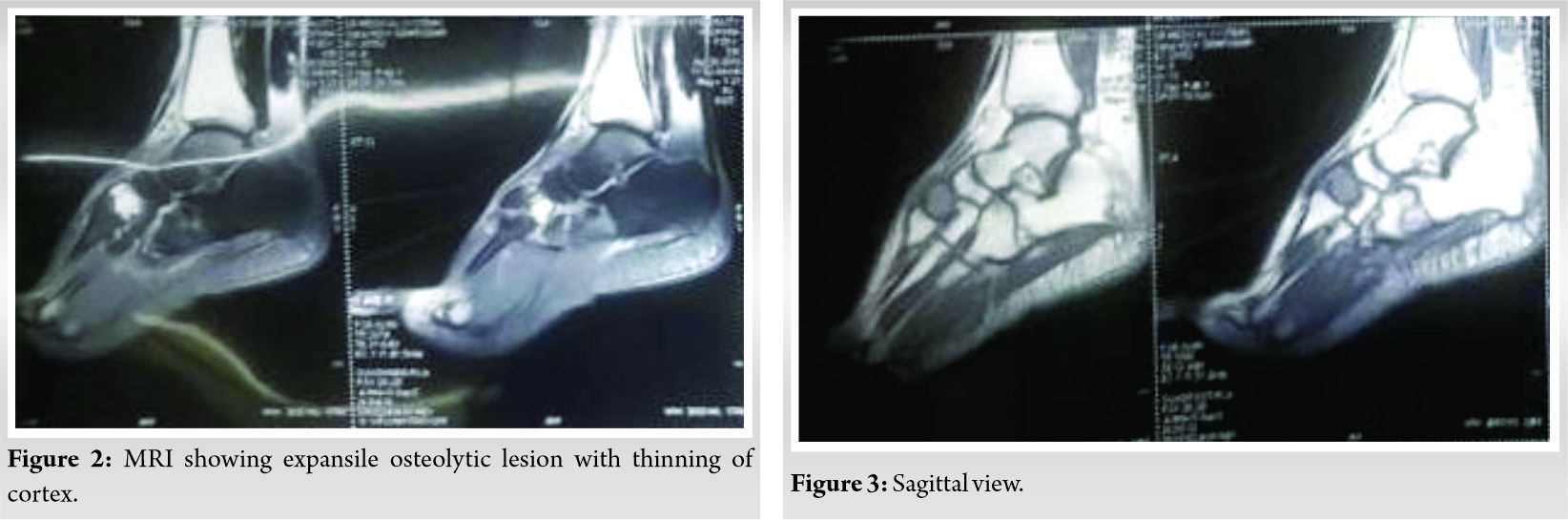 MRI of right foot (Fig. 2, 3, 4, 7) was done which showed an expansile osteolytic lesion with multiple internal septations in intermediate cuneiform with thinning of the cortex.
MRI of right foot (Fig. 2, 3, 4, 7) was done which showed an expansile osteolytic lesion with multiple internal septations in intermediate cuneiform with thinning of the cortex. 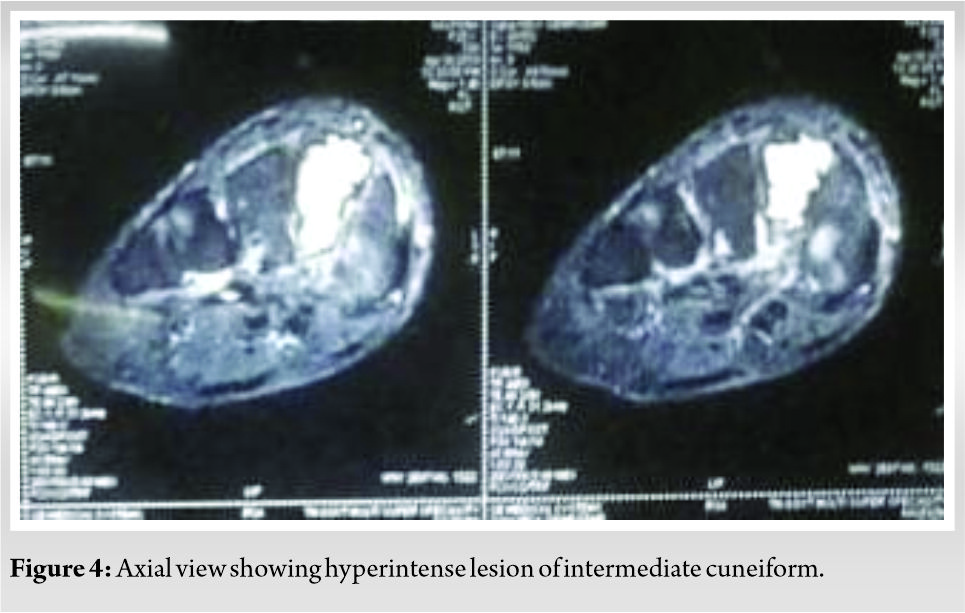 Patient was planned for surgery, the incision was made over the dorsum of the foot, the bone was approached between extensor hallucis longus and extensor digitorum brevis.The intermediate cuneiform was identified and excised completely and was sent for histopathological examination. There was no extension of the lesion to the surrounding soft tissues. Postop xray (Fig. 5) showed the removal of intermediate cuneiform.
Patient was planned for surgery, the incision was made over the dorsum of the foot, the bone was approached between extensor hallucis longus and extensor digitorum brevis.The intermediate cuneiform was identified and excised completely and was sent for histopathological examination. There was no extension of the lesion to the surrounding soft tissues. Postop xray (Fig. 5) showed the removal of intermediate cuneiform. 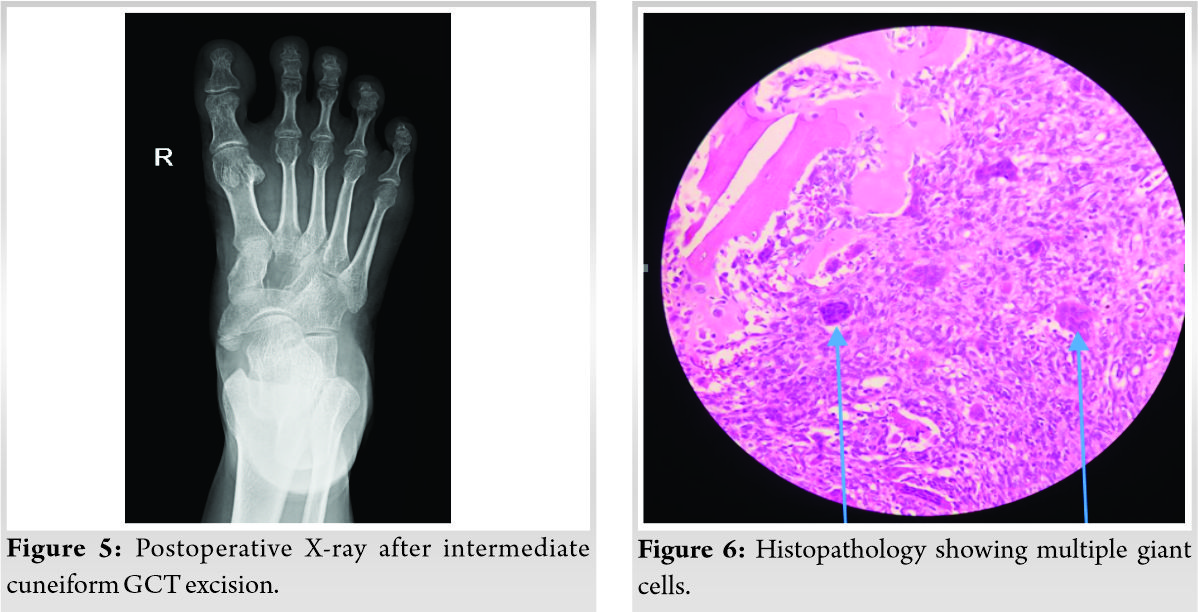 Microscopic examination showed the presence of focal giant cell-rich lesions with background stromal cells, and areas of hemorrhage were also noted (Fig. 6 and 8).
Microscopic examination showed the presence of focal giant cell-rich lesions with background stromal cells, and areas of hemorrhage were also noted (Fig. 6 and 8). 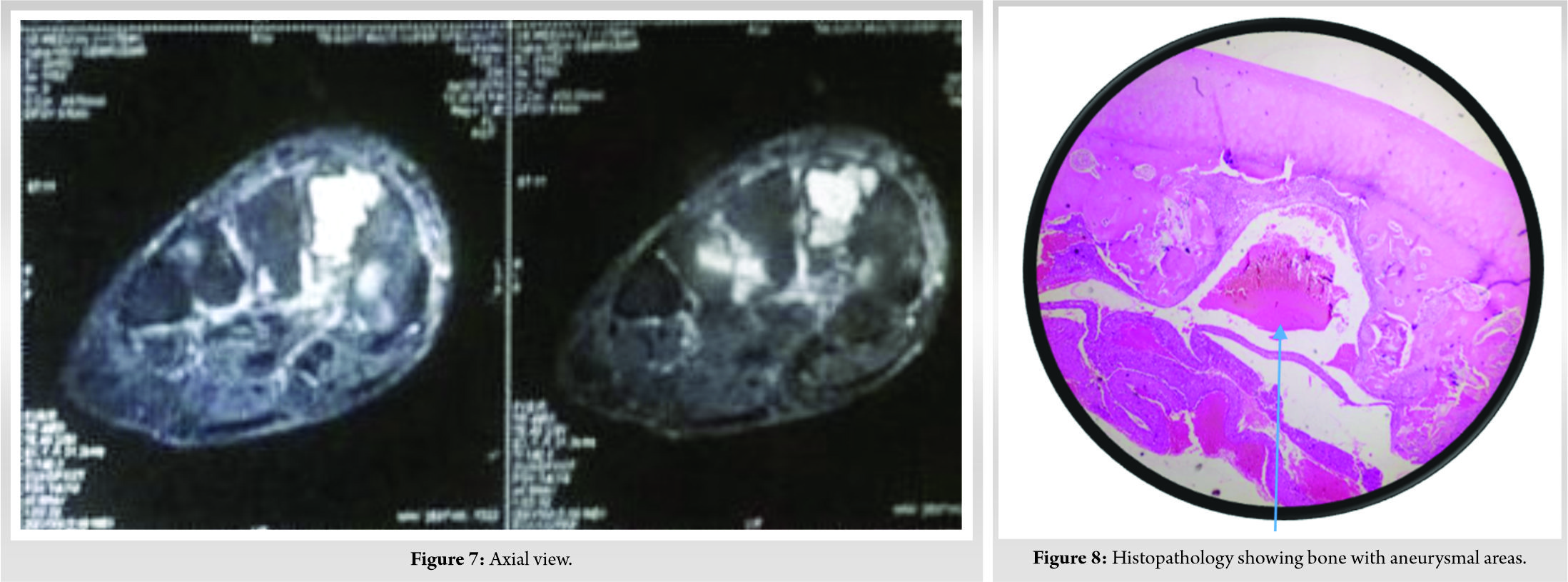 The finding in the microscopic picture helped us in narrowing our diagnosis to GCT evolving into secondary ABC. The patient was made to partially weight bear for 1 month and following that full weight bearing was started. The patient was not on any sort of immobilizing splint to the ankle or foot. The patient was followed periodically and by 1-year patient was able to weight bear without pain and there was no recurrence of lesion in the foot. Foot Function Index [5] preoperatively was 49% (84/170) and got improved to 5% (9/170) after 1 year postoperatively. Activity limitation scale improved from 13% to 3%.
The finding in the microscopic picture helped us in narrowing our diagnosis to GCT evolving into secondary ABC. The patient was made to partially weight bear for 1 month and following that full weight bearing was started. The patient was not on any sort of immobilizing splint to the ankle or foot. The patient was followed periodically and by 1-year patient was able to weight bear without pain and there was no recurrence of lesion in the foot. Foot Function Index [5] preoperatively was 49% (84/170) and got improved to 5% (9/170) after 1 year postoperatively. Activity limitation scale improved from 13% to 3%.
GCT is characterized by the presence of multi-nucleated giant cells and it occurs mostly in skeletally mature patients between the age group of 20–50 years. Mostly, they are benign with a risk of malignancy in <1% of cases. They mostly occur in epiphysis of long bones involving mostly distal end of femur, proximal tibia, distal end of radius [6, 7]. Spine and pelvis may be rarely involved. GCT of hand and foot are very rare presentation [8, 9]. In the study done by Biscaglia et al., [8] 2 cases involving medial cuneiform and 1 case involving lateral cuneiform were reported. In the study done by O’Keefe et al. [9], 2 cases of GCT involving cuneiform were reported.
ABC is a benign lesion and it is composed of blood filled spaces. The matrix is separated by connective tissue septa. The occur mostly in the 2nd decade. ABC involves mostly metaphysis of long bones followed by spine. They may arise de novo called primary ABC or from pre-existing osseous lesions called secondary ABC. Secondary ABC mostly occur from GCT, osteoblastoma, chondroblastoma, fibrous dysplasia. The most common theory for the formation of secondary ABC is arteriovenous malformation of the pre-existing bony lesion [10].
It has been observed that GCT of hand and feet differs from GCT of usual location by shorter duration of symptoms before the patient comes to hospital for intervention. It may be due to limited space in the hand and foot bones. Even the small tumor will cause significant swelling in the foot and causes symptoms to the patients [11]. Patients with GCT of cuneiform and small bones present at an average of 6 months earlier when compared to GCT of long bones.
In radiology, it is difficult to differentiate between GCT and ABC. Because both will have osteolytic lesion in X-ray [4]. MRI will show hyperintense lesion in T2 MRI and hypo-intense lesion in T1 MRI. MRI will show fluid-filled levels in ABC, but it is not typical to ABC. This finding can also be seen in other GCT like lesions such as chondroblastoma [12].
Hence, only histology can differentiate between primary ABC and secondary ABC evolving from GCT. In our case, there were no septations seen in the lesion as per X-ray. In MRI, there were no fluid levels. Hence, our diagnosis before biopsy report was provisionally made as GCT. However, biopsy report showed the presence of hemorrhagic areas, and hence, it was diagnosed as GCT transforming into ABC. However, the treatment will not vary for both the conditions unless any features of malignant changes are present in the biopsy.
In our case, we have did complete excision of the intermediate cuneiform without any additional grafting. Since curettage of the lesion and bone grafting has high chance of recurrence we proceeded with excision of cuneiform. The patient was able to walk without any difficulty following surgery. There were no gait disturbances while walking. After 1-year follow-up, there was no recurrence of lesion and the patient was asymptomatic at the end of 1 year. In a study done by Verma et al., [13] the middle cuneiform was removed completely for a dislocation caused by trauma. The patient was asymptomatic postoperatively and had no complications due to the absent intermediate cuneiform which was similar to our study.
GCT with secondary transformation into ABC is a rare entity in small bones. It is even more rare to occur in the intermediate cuneiform. The treatment of choice will be similar to any other GCT which is curettage with bone grafting or complete excision of the lesion. We can either plan for biopsy or definitive treatment depending on the nature of lesion. Curettage alone has more chance of recurrence, and hence, it is best to go for complete excision of the lesion with or without bone grafting.
Osteolytic lesions are rare to occur in small bones. Thus, any swelling with pain in small bones must be given importance and X-ray must be done to look for any pathology in bone. The lytic lesion in the small bones is more likely to be missed. Any lytic lesion must be given importance, and further evaluation is needed like MRI to find the exact pathology.
References
- 1.Turcotte RE. Giant cell tumor of bone. Orthop Clin North Am 2006;37:35-51. [Google Scholar]
- 2.Jaffe HL, Lichtenstein L. Benign chondroblastoma of bone: A reinterpretation of the so-called calcifying or chondromatous giant cell tumor. Am J Pathol 1942;18:969-91. [Google Scholar]
- 3.de Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK. Aneurysmal bone cyst. A clinicopathologic study of 238 cases. Cancer 1992;69:2921-31. [Google Scholar]
- 4.Li M, Gan Y, Shi D, Zhao J. Huge aneurysmal bone cyst secondary to giant cell tumor of the hand phalanx: A case report and related literature. BMC Cancer 2020;20:233. [Google Scholar]
- 5.Budiman-Mak E, Conrad KJ, Roach KE. The foot function index: A measure of foot pain and disability. J Clin Epidemiol 1991;44:561-70. [Google Scholar]
- 6.Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg Am 1987;69:106-14. [Google Scholar]
- 7.Dahlin DC, Cupps RE, Johnson EW Jr. Giant-cell tumor: A study of 195 cases. Cancer 1970;25:1061-70. [Google Scholar]
- 8.Biscaglia R, Bacchini P, Bertoni F. Giant cell tumor of the bones of the hand and foot. Cáncer 2000;88:2022-32. [Google Scholar]
- 9.O’Keefe RJ, O’Donnell RJ, Temple HT, Scully SP, Mankin HJ. Giant cell tumor of bone in the foot and ankle. Foot Ankle Int 1995;16:617-23. [Google Scholar]
- 10.Patel PJ, Demos TC, Lomasney LM, Rapp T. Your diagnosis? Aneurysmal bone cyst. Orthopedics 2005;28:428-511. [Google Scholar]
- 11.Khanna AK, Sharma SV, Kumar M. A large metatarsal giant-cell tumor. Acta Orthop Scand 1990;61:271-2. [Google Scholar]
- 12.Roemer FW, Remplik P, Bohndorf K. Uncommon aneurysmal bone cyst: Radiographic and MRI findings. AJR Am J Roentgenol 2005;184:349. [Google Scholar]
- 13.Verma A, Sharma VK, Batra S, Rohria MS. Neglected isolated plantar dislocation of middle cuneiform: A case report. BMC Musculoskelet Disord 2007;8:5. [Google Scholar]









