Although atypical femoral fractures are associated with the use of bisphosphonates or denosumab, they can occur without prior use of these drugs.
Dr. George F. Georgiadis, Department of Orthopaedics, Asclepieion Voulas General Hospital, Voula, Athens, Greece. E-mail: gegeorgiades@yahoo.com
Introduction: Atypical femoral fractures (AFF) are associated with the use of bisphosphonates (BPs) or denosumab. However, few cases that meet the characteristics of these fractures, as established by the American Society of Bone and Mineral Research, have occurred in patients who have never used antiresorptive drugs.
Case Report:We report a case of AFF in a 67-year-old woman who had never used antiresorptive medications. The history and comorbidities of the patient, the characteristics of the fracture, and the subsequent treatment are presented.
Conclusion: AFFs may occur even in patients who have never been exposed to BPs or denosumab. The absence of antiresorptive osteoporosis therapy and the lack of radiographic focal periosteal reaction in the lateral femoral cortex, as in our case, can make it difficult to detect and prevent the disorder. Prolonged use of proton pump inhibitors and Vitamin D deficiency-related osteomalacia may contribute to the occurrence of these fractures. Further studies are required to accurately understand all inciting factors contributing to the development of AFFs.
Keywords: Atypical femoral fractures, subtrochanteric fractures, denosumab, bisphosphonates, antiresorptive drugs.
Prolonged antiresorptive therapy with bisphosphonates (BPs) or denosumab for osteoporosis as well as high-dose antiresorptive therapy in patients with metastatic bone disease are associated with atypical femoral fractures (AFFs) [1]. However, a few cases of femoral stress fractures which fulfill the features of AFFs established by the American Society of Bone and Mineral Research (ASBMR) have been reported in patients who never used antiresorptive drugs [2, 3, 4]. For that reason, the ASBMR Task Force 2013 Revised Case Definition of AFFs did not include the use of antiresorptive medications in the minor features of AFFs. We present a case of AFF in a patient who has never received BPs or denosumab.
In October 2019, a 67-year-old woman presented to the emergency department of our hospital with a spontaneous right femur fracture which occurred while she was trying to sit on her bed. Upon her arrival, she reported experiencing constant pain in her right thigh for a period of 4 months and that 2 months earlier she had visited the Orthopaedic outpatient Clinics of the hospital for the same reason. Plain lumbar spine X-rays performed at that time, showed findings of mild spondyloarthritis. An anteroposterior radiograph of her right hip showed a subtle minimal endosteal thickening without localized periosteal thickening in the lateral cortex of the right subtrochanteric femur. The X-ray was misinterpreted as normal (Fig. 1).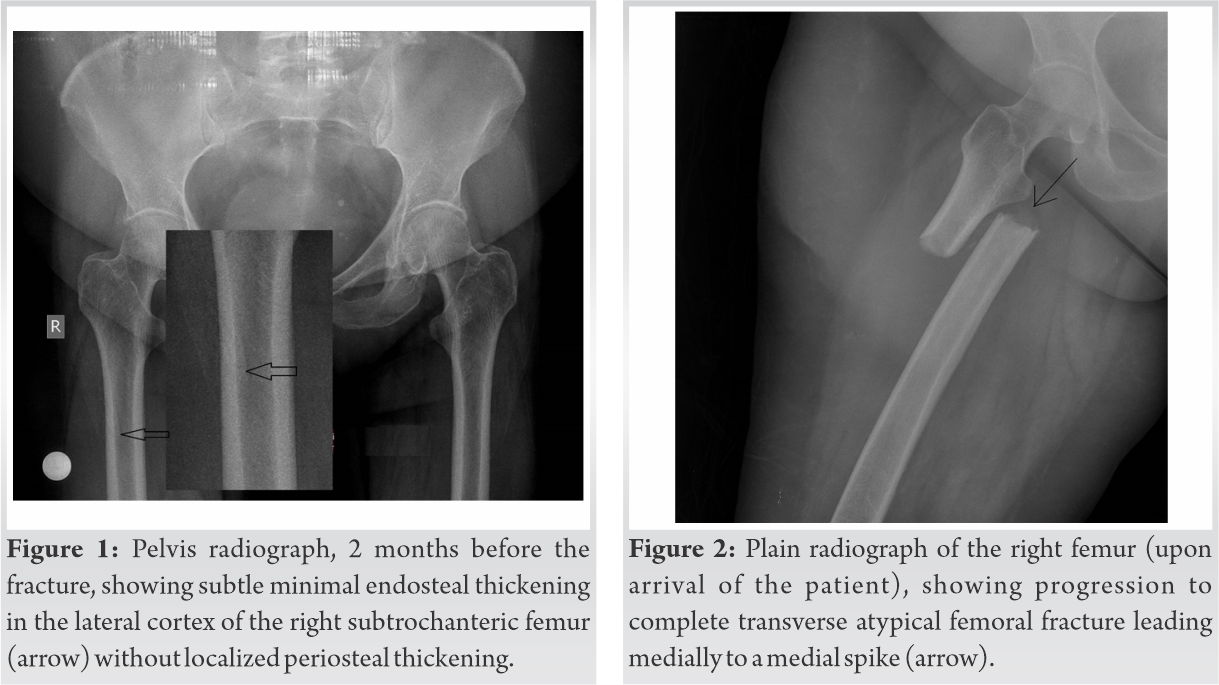
The new serial hip radiographs revealed a noncomminuted fracture, located just below the lesser trochanter, and transverse in orientation (Fig. 2). Multidetector computed tomography (MDCT) of the femur demonstrated a complete transverse fracture without focal cortical thickening of the shaft (Fig. 3). Radiographs and MDCT scan of the contralateral femur were negative.
The patient denied any exposure to BPs or denosumab. She never underwent a bone mineral density (BMD) measurement and had no history of kidney failure, steroid use, endocrine or genetic disorders. She received intermittent treatment with omeprazole for 4 years due to gastric ulcer.
Long cephalomedullary interlocking nailing was performed on the same day (Fig. 4). 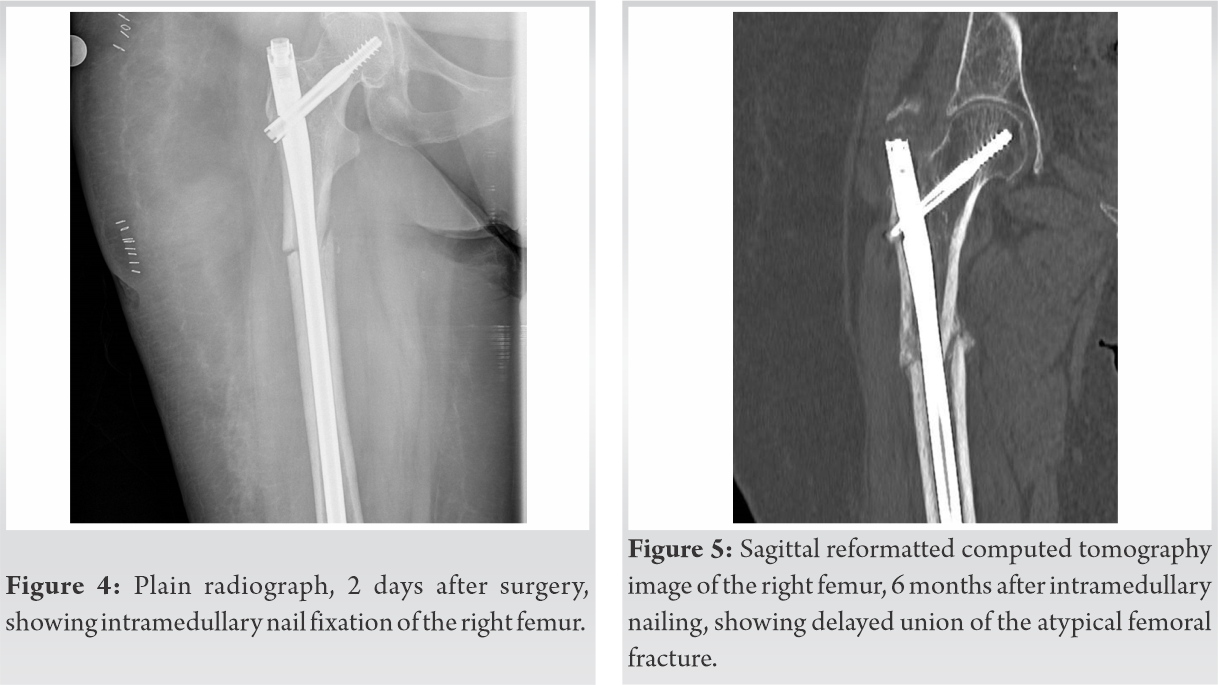 In addition, tissue from the fracture area was obtained during surgery and sent for histopathology. This showed no malignancy. The patient was discharged from the hospital 4 days later, with instructions to visit the outpatient Clinic of Osteoporosis, as soon as possible, for further examination and investigation of the cause of fracture. Unfortunately, she did not comply. 3 months later, during follow-up, the fracture failed to show clinical and radiographic signs of progressive callus formation, and the nail was dynamized. Despite this, the fracture continued to show a delay in union 6 months post-operatively (Fig. 5). At that time, 25-hydroxy-vitamin D (25 OH Vit D) level was low (7.6 ng/m), parathyroid hormone (PTH) and alkaline phosphatase (ALP) were high (171 pg/ml and 230 U/L, respectively) while urea, creatinine, blood calcium and blood phosphorous were in normal ranges. Dual-energy X-ray absorptiometry revealed a low BMD of the contralateral femoral neck (0,633 gr/cm2). Unfortunately, no bone turnover markers or histological indexes were obtained at any point during the course of the patient. Vitamin D and calcium supplements were prescribed and 6 months later the patient had normal serum levels of 25 OH Vitamin D, PTH, and ALP and she initiated treatment with teriparatide. Fracture healing occurred 13 months after the initial operation with callus formation (Fig. 6a, 6b).
In addition, tissue from the fracture area was obtained during surgery and sent for histopathology. This showed no malignancy. The patient was discharged from the hospital 4 days later, with instructions to visit the outpatient Clinic of Osteoporosis, as soon as possible, for further examination and investigation of the cause of fracture. Unfortunately, she did not comply. 3 months later, during follow-up, the fracture failed to show clinical and radiographic signs of progressive callus formation, and the nail was dynamized. Despite this, the fracture continued to show a delay in union 6 months post-operatively (Fig. 5). At that time, 25-hydroxy-vitamin D (25 OH Vit D) level was low (7.6 ng/m), parathyroid hormone (PTH) and alkaline phosphatase (ALP) were high (171 pg/ml and 230 U/L, respectively) while urea, creatinine, blood calcium and blood phosphorous were in normal ranges. Dual-energy X-ray absorptiometry revealed a low BMD of the contralateral femoral neck (0,633 gr/cm2). Unfortunately, no bone turnover markers or histological indexes were obtained at any point during the course of the patient. Vitamin D and calcium supplements were prescribed and 6 months later the patient had normal serum levels of 25 OH Vitamin D, PTH, and ALP and she initiated treatment with teriparatide. Fracture healing occurred 13 months after the initial operation with callus formation (Fig. 6a, 6b).
The fracture was defined as AFF because it fulfilled all major criteria for the definition of AFFs established by ASBMR [1, 2]. It was located in the subtrochanteric region, it was transverse with a medial spike, there was no trauma, there was no comminution and there was an endosteal thickening of the lateral cortex, albeit without periosteal reaction. It also displayed the minor features of prodromal pain and delayed fracture union. The absence of focal periosteal reaction at the lateral femoral cortex on the initial radiograph and the subtle nature of the endosteal thickening may explain why the disorder was not initially diagnosed.
Current evidence suggests that there is an association between antiresorptive agent use and AFFs [1, 3, 4, 5]. Long-term use or high dosing of antiresorptive agents inhibits osteoclast function and causes a reduction of bone turnover and alterations of bone structure and biomechanics. Microcracks within the lateral femoral cortex are not adequately repaired due to the severe suppression of bone remodeling and accumulation of defects over time leads to fracture. As early as 2005, Odvina et al. reported nine atraumatic or low-energy subtrochanteric and diaphyseal femoral fractures associated with prolonged BP treatment [5]. Despite that, ASBMR did not include the use of antiresorptive therapy in the features needed for the definition of AFFs because as in our case, AFF can occur in patients who have never used antiresorptive therapy [2].
Low energy fractures of the femur with the characteristic radiographic pattern of atypical fractures have been previously reported in patients not receiving BPs or denosumab, though these cases are relatively infrequent [2, 3, 4]. The presence of a genetic metabolic bone disorder may predispose to the development of AFF. A number of monogenetic bone disorders, including hypophosphatasia, X-linked hypophosphatemia, pycnodysostosis, osteopetrosis, X-linked osteoporosis, and osteogenesis imperfecta were identified in patients with AFFs [6]. All of these cases, with the exception of osteogenesis imperfecta, were associated with the use of BPs. Nevertheless, our patient did not have any of these genetic disorders. Femur geometry parameters like lateral femoral bowing and varus hip alignment increase tensile stress on the lateral femoral cortex, in turn increasing the risk of an AFF [7, 8]. Our patient did not show increased lateral femoral bowing and she had rather valgus femoral geometry (Fig. 1).
Additional factors associated with deterioration of bone quality such as the use of certain medications (glucocorticoids, proton pump inhibitors [PPIs]) [9], certain comorbid conditions (type 1 diabetes, rheumatoid arthritis, and other autoimmune disease) [10, 11], and conditions with impaired mineralization caused by osteomalacia or Vitamin D deficiency [11], are considered risk factors for AFFs. In the present case, the patient was on PPIs for 4 years and we speculate she had osteomalacia from Vitamin D deficiency, based on the low levels of 25 OH Vit D and high levels of PTH and ALP documented 6 months after the fracture. PPI use may decrease bone strength and increase the incidence of insufficiency fractures by inhibiting proton pumps in osteoclasts and decreasing bone turnover, impairing calcium absorption, and altering homocysteine levels through impairment of folate and vitamin B12 absorption [12, 13]. Vitamin D deficiency-related osteomalacia may predispose to femur deformities such as bowing and curving and is a common cause of insufficiency fractures in the elderly [14].
The lack of radiographic lateral femoral “beaking” (localized periosteal or endosteal thickening that resembles a bird’s beak) makes it difficult to identify and prevent the completion of AFFs in patients with prodromal symptoms, even when the disorder is suspected. Radiographic beaking at the lateral femoral cortex was observed less frequently in patients with AFFs not treated with BPs than in patients treated with BPs (37.9% vs. 86.1%) [15]. Perhaps MRI imaging should be considered when this disorder is suspected in patients without a history of antiresorptive therapy and plain radiographs are negative, because of the low sensitivity of X-rays in this patient population.
AFFs have a prolonged healing time and increased rate of nonunion, as would be expected given the underlying pathophysiology of these fractures [2, 5]. Static cephalomedullary nailing remains the first-line treatment of choice for most authors for both complete and incomplete AFFs regardless of antiresorptive therapy exposure. Combination therapy with teriparatide, Vitamin D and calcium, effectively enhance AFF healing [15].
Our case highlights that some patients may sustain AFFs without exposure to BPs or denosumab. The absence of an antiresorptive osteoporosis therapy history and the frequent absence of radiographic focal periosteal or endosteal thickening at the lateral femoral cortex, as in our case, complicate the early diagnosis and implementation of preventative measures. Prolonged PPI use and Vitamin D-related deficiency osteomalacia may contribute to AFF occurrence. Further studies are required to accurately understand all inciting factors contributing to the development of AFFs.
AFFs are associated with the use of BPs or denosumab. However, they can occur without prior use of these drugs. Careful and detailed laboratory and imaging examination of patients can lead to early detection and prevention of this type of fractures.
References
- 1.Starr J, Tay YK, Shane E. Current understanding of epidemiology, pathophysiology, and management of atypical femur fractures. Curr Osteoporos Rep 2018;16:519-29. [Google Scholar]
- 2.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American society for bone and mineral research. J Bone Miner Res 2014;29:1-23. [Google Scholar]
- 3.Tan S, Koh S, Goh S, Howe T. Atypical femoral stress fractures in bisphosphonate-free patients. Osteoporos Int 2011;22:2211-2. [Google Scholar]
- 4.Szolomayer LK, Ibe IK, Lindskog DM. Bilateral atypical femur fractures without bisphosphonate exposure. Skeletal Radiol 2017;46:241-7. [Google Scholar]
- 5.Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: A potential complication of alendronate therapy. J Clin Endocrinol Metab 2005;90:1294-301. [Google Scholar]
- 6.Nguyen HH, van de Laarschot DM, Verkerk AJ, Milat F, Zillikens MC, Ebeling PR. Genetic risk factors for atypical femoral fractures (AFFs): A systematic review. JBMR Plus 2018;2:1-11. [Google Scholar]
- 7.Morin SN, Wall M, Belzile EL, Godbout B, Moser TP, Michou L, et al. Assessment of femur geometrical parameters using EOS™ imaging technology in patients with atypical femur fractures; preliminary results. Bone 2016;83:184-9. [Google Scholar]
- 8.Sasaki S, Miyakoshi N, Hongo M, Kasukawa Y, Shimada Y. Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: A case series. J Bone Miner Metab 2012;30:561-7. [Google Scholar]
- 9.Giusti A, Hamdy NA, Papapoulos SE. Atypical fractures of the femur and bisphosphonate therapy. Bone 2010;47:169-80. [Google Scholar]
- 10.Rasmussen NH, Dal J, de Vries F, van den Bergh JP, Jensen MH, Vestergaard P. Diabetes and fractures: New evidence of atypical femoral fractures? Osteoporos Int 2020;31:447-55. [Google Scholar]
- 11.Girgis CM, Sher D, Seibel MJ. Atypical femoral fractures and bisphosphonate use. N Engl J Med 2010;362:1848-9. [Google Scholar]
- 12.Mizunashi K, Furukawa Y, Katano K, Abe K. Effect of omeprazole, an inhibitor of H+, K(+)- ATPase, on bone resorption in humans. Calcif Tissue Int 1993;53:21-5. [Google Scholar]
- 13.O’Connell MB, Madden DM, Murray AM, Heaney RP, Kerzner LJ. Effects of proton pump inhibitors on calcium carbonate absorption in women: A randomized crossover trial. Am J Med 2005;118:778-81. [Google Scholar]
- 14.McKenna MJ, Kleerekoper M, Ellis BI, Rao DS, Parfitt AM, Frame B. Atypical insufficiency fractures confused with Looser zones of osteomalacia. Bone 1987;8:71-8. [Google Scholar]
- 15.Hagino H, Endo N, Yamamoto T, Harada A, Iwamoto J, Kondo N, et al. Treatment status and radiographic features of patients with atypical femoral fractures. J Orthop Sci 2018;23:316-20. [Google Scholar]











