Intra-articular malunion of the elbow can treat by extra-articular corrective osteotomy in children.
Dr. Hiroki Shibayama, Department of Orthopaedic Surgery, KKR Sapporo Medical Center, Sapporo, Hokkaido, Japan. E-mail: hiroki2001com@yahoo.co.jp
Introduction: Malunion of intra-articular fracture of the elbow in children is uncommon and may be difficult to treat. Intra-articular corrective osteotomies are still not commonly performed in children, and the main reason is the concern regarding the risk of osteonecrosis. We present a case of extra-articular corrective osteotomy for malunion after open reduction and internal fixation for fracture dislocation of the elbow.
Case Report: An 8-year-old boy was injured by a fall and he underwent an operation the day after the injury with diagnosis of lateral condyle fracture of the right humerus. He was referred to our department 4 months after the operation due to restricted range of motion. His elbow exhibited cubitus varus, and range of motion was 80° of flexion, −30° of extension, 55° of pronation, and 85° of supination. Plain radiographs showed malunion, a Baumann angle of 3°, and a tilting angle of 5°. We diagnosed this injury not as lateral condyle fracture but as posterolateral dislocation with Milch type 1 lateral condyle fracture associated with osteochondral flap fracture of the coronoid process with computed tomography images at the time of injury. Because the patient was only 8 years old, we decided to perform an extra-articular corrective osteotomy to encourage bone remodeling and improve the flexion range of motion. After the operation, the range of motion improved as 130° of flexion, −30° of extension, 85° of pronation, and 90° of supination 4 years after the operation. Plain radiographs showed that the epiphysis of the capitellum was closed, and the trochlea presented a fishtail deformity.
Conclusion: We obtained relatively good outcomes with extra-articular corrective osteotomy, and long-term follow-up is necessary. Especially in the elbow, the injury itself may cause fishtail deformity due to avascular necrosis of the trochlea, and if an additional osteotomy is performed, the risk increases. Although there is concern about the occurrence of secondary osteoarthritis, we expect that the intra-articular deformity would be remodeled due to the patient’s young age if normal elbow movement could be obtained.
Keywords: Fracture-dislocation of the elbow, malunion, osteochondral flap fracture, osteotomy, pediatrics.
Lateral condyle fractures of the humerus occur in about 15% of all elbow injuries in children [1]. Moreover, anatomical reduction is necessary for treatment, because such fractures are intra-articular. Malunion of intra-articular fracture is treated by intra-articular corrective osteotomy in adults, but this is rarely performed in children due to the risk of osteonecrosis and difficulty of the technique [2]. Although many reports have described extra-articular corrective osteotomies for cubitus varus after supracondylar fractures of the humerus in children [3, 4], we found no report of extra-articular osteotomy for malunion of intra-articular fractures. We, herein, report a case of extra-articular corrective osteotomy for malunion after open reduction and internal fixation (ORIF) in an 8-year-old boy. His injury was posterolateral dislocation of the elbow associated with a Milch type 1 lateral condyle fracture and osteochondral flap fracture (OCFF) of the coronoid process.
An 8-year-old boy was injured by a fall while riding a snowmobile with his uncle. He was transported to a hospital, where he was diagnosed with a lateral condyle fracture of the right humerus. He underwent ORIF the day after the injury (Fig. 1, 2). 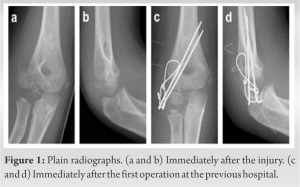
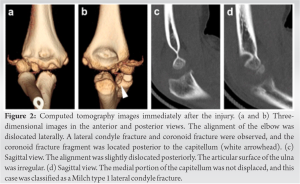 Recovery of his range of motion was poor postoperatively and did not improve even after the implant removal; therefore, the patient was referred to our department 4 months after the injury. On presentation to our hospital, the patient’s chief complaint was limited range of motion of the right elbow; he had no pain. On physical examination, his elbow exhibited cubitus varus with a carrying angle of 195°, and range of motion was 80° of flexion, −30° of extension, 55° of pronation, and 85° of supination. Yamamoto’s test showed 20° of internal rotation deformity in the right humerus [5]. Plain radiographs showed malunion after ORIF, a Baumann angle of 3°, and a tilting angle of 0°. A bone defect of the medial part of the capitellum and a sharpened coronoid process was also observed (Fig. 3). Computed tomography (CT) images showed that the medial part of the capitellum was present in the anatomical position, and the lateral condyle fragment including the lateral part of the capitellum was united in an extended position. Irregularities of the articular surface of the ulna and trochlea were observed, and heterotopic ossification was present around the medial collateral ligament (Fig. 4). CT images at the time of the injury showed that the ulnohumeral joint was subluxated laterally, with Milch type 1 fracture of the lateral condyle and fracture of the coronoid process of the ulna. There was a deficiency of the articular surface of the ulna from the coronoid process toward the trochlear notch on the sagittal view, and the fragment of the coronoid process was located posterior to the capitellum (Fig. 2). Based on these findings, we diagnosed this injury not as lateral condyle fracture of the humerus but as posterolateral dislocation of the elbow with Milch type 1 lateral condyle fracture associated with OCFF of the coronoid process. The cause of the deformity was thought to be failed reduction of the osteochondral fragment of the coronoid process, resulting in subluxation of the ulnohumeral joint; the OCFF fragment was also preventing anatomical reduction of the lateral condyle. As a result, the lateral condyle was malunited into an extension deformity, and deformity of the coronoid process remained. Because a carrying angle of the non-injured side was 175°, his deformity was considered to be 20° of varus, 20° of internal rotation, and 45° of extension. The patient’s elbow flexion was severely limited to 80°, and he had difficulty in daily life; therefore, it was necessary to improve the flexion range of his elbow. Because the patient was only 8 years old and had no elbow pain, we decided to perform an extra-articular corrective osteotomy to improve the flexion range of motion and encourage bone remodeling rather than an intra-articular osteotomy. The patient and his parents provided informed consent for this procedure. The operation was performed under general anesthesia 6 months after the injury. With the patient in the supine position, the previous skin incision on the lateral side of the elbow was extended proximally to expose the humerus, and a 20° lateral wedge of the humerus was removed at the distal diaphysis.
Recovery of his range of motion was poor postoperatively and did not improve even after the implant removal; therefore, the patient was referred to our department 4 months after the injury. On presentation to our hospital, the patient’s chief complaint was limited range of motion of the right elbow; he had no pain. On physical examination, his elbow exhibited cubitus varus with a carrying angle of 195°, and range of motion was 80° of flexion, −30° of extension, 55° of pronation, and 85° of supination. Yamamoto’s test showed 20° of internal rotation deformity in the right humerus [5]. Plain radiographs showed malunion after ORIF, a Baumann angle of 3°, and a tilting angle of 0°. A bone defect of the medial part of the capitellum and a sharpened coronoid process was also observed (Fig. 3). Computed tomography (CT) images showed that the medial part of the capitellum was present in the anatomical position, and the lateral condyle fragment including the lateral part of the capitellum was united in an extended position. Irregularities of the articular surface of the ulna and trochlea were observed, and heterotopic ossification was present around the medial collateral ligament (Fig. 4). CT images at the time of the injury showed that the ulnohumeral joint was subluxated laterally, with Milch type 1 fracture of the lateral condyle and fracture of the coronoid process of the ulna. There was a deficiency of the articular surface of the ulna from the coronoid process toward the trochlear notch on the sagittal view, and the fragment of the coronoid process was located posterior to the capitellum (Fig. 2). Based on these findings, we diagnosed this injury not as lateral condyle fracture of the humerus but as posterolateral dislocation of the elbow with Milch type 1 lateral condyle fracture associated with OCFF of the coronoid process. The cause of the deformity was thought to be failed reduction of the osteochondral fragment of the coronoid process, resulting in subluxation of the ulnohumeral joint; the OCFF fragment was also preventing anatomical reduction of the lateral condyle. As a result, the lateral condyle was malunited into an extension deformity, and deformity of the coronoid process remained. Because a carrying angle of the non-injured side was 175°, his deformity was considered to be 20° of varus, 20° of internal rotation, and 45° of extension. The patient’s elbow flexion was severely limited to 80°, and he had difficulty in daily life; therefore, it was necessary to improve the flexion range of his elbow. Because the patient was only 8 years old and had no elbow pain, we decided to perform an extra-articular corrective osteotomy to improve the flexion range of motion and encourage bone remodeling rather than an intra-articular osteotomy. The patient and his parents provided informed consent for this procedure. The operation was performed under general anesthesia 6 months after the injury. With the patient in the supine position, the previous skin incision on the lateral side of the elbow was extended proximally to expose the humerus, and a 20° lateral wedge of the humerus was removed at the distal diaphysis. 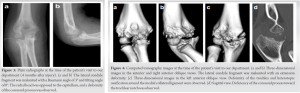 Two 3.5-mm half-pins were then inserted into both fragments, and the pins were fixed to each other with wire and cement to close the wedge while correcting the cubitus varus, internal rotation, and extension deformities [6, 7]. The angle of flexion was defined as the angle at which the hand could reach the mouth when the elbow was flexed. Due to a gap on the dorsal side of the osteotomy, the resected wedge bone was grafted and the fragments were additionally stabilized to each other with a wire (Fig. 5). Bone healing progressed well postoperatively, and the external fixators were removed 3 months after the operation. Then, exercise of the range of motion was started, and it The range of motion improved to 125° of flexion and −35° of extension over the next year. At the time of this, writing 4 years had passed since the operation, and the patient had no pain or limitations in daily life. He was able to play sports activities as well as other children. His range of motion was 130° of flexion, −30° of extension, 85° of pronation, and 90° of supination, and Yamamoto’s test showed 20° on both sides. Plain radiographs showed that the epiphysis of the capitellum was closed, and the trochlea presented a fishtail deformity (Fig. 6).
Two 3.5-mm half-pins were then inserted into both fragments, and the pins were fixed to each other with wire and cement to close the wedge while correcting the cubitus varus, internal rotation, and extension deformities [6, 7]. The angle of flexion was defined as the angle at which the hand could reach the mouth when the elbow was flexed. Due to a gap on the dorsal side of the osteotomy, the resected wedge bone was grafted and the fragments were additionally stabilized to each other with a wire (Fig. 5). Bone healing progressed well postoperatively, and the external fixators were removed 3 months after the operation. Then, exercise of the range of motion was started, and it The range of motion improved to 125° of flexion and −35° of extension over the next year. At the time of this, writing 4 years had passed since the operation, and the patient had no pain or limitations in daily life. He was able to play sports activities as well as other children. His range of motion was 130° of flexion, −30° of extension, 85° of pronation, and 90° of supination, and Yamamoto’s test showed 20° on both sides. Plain radiographs showed that the epiphysis of the capitellum was closed, and the trochlea presented a fishtail deformity (Fig. 6).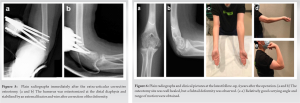
Several reports have described intra-articular corrective osteotomies in adults for malunion of intra-articular fractures in the upper extremities, but only one report has described such treatment in children [2]. Almost all cases involved injury, the one exception is a report of intra-articular osteotomy by Feldman et al. [8], who described the treatment of genu valgum in a child with lateral compartment deficiency. It seems that this procedure is still not commonly performed in children. The main reason for this is the concern regarding the risk of osteonecrosis; in addition, the procedure is reported to be technically difficult and prone to complications [8]. Especially in the elbow, the injury itself may cause fishtail deformity due to avascular necrosis of the trochlea, and if an additional osteotomy is performed, the risk increases. Although there was concern about the occurrence of secondary osteoarthritis, we expected that the intra-articular deformity would be remodeled due to the patient’s young age. Therefore, we aimed to correct the axial and rotational deformities of the humerus to correct the direction of flexion and extension force applied to the elbow joint with an extra-articular osteotomy. The osteotomy site was the distal diaphysis of the humerus, as in the osteotomy for cubitus varus after supracondylar fracture [3], and it was stabilized in flexed position to ensure improvement of the elbow flexion. It took about 1 year for the patient’s range of motion to improve after removal of the external fixation, but the patient had no disability in activities of daily life 4 years postoperatively. Not only did the flexion angle improve but also the extension and pronation angles also improved. This phenomenon is also seen after performing osteotomies for malunions after supracondylar fractures and is probably due to the effect of rehabilitation after the osteotomy. In this case, there may have been some bone remodeling, but we do not know the details because we did not perform magnetic resonance imaging (MRI) postoperatively. At the time of this writing, plain radiographs showed a fishtail deformity, and long-term follow-up is necessary to monitor for the occurrence of further deformity and osteoarthritis. Of all elbow injuries in children, lateral condyle fractures of the humerus occur in about 15% and dislocations of the elbow in about 3% [1, 9, 10]. Approximately 60% to 70% of elbow dislocations are reportedly associated with fractures, most of which are medial epicondyle fractures; they are very rarely lateral condyle fractures [9, 10]. A survey of the literature showed that elbow dislocations with lateral condyle fractures account for about 0.5% of all elbow injuries [11] and mainly occur in children aged 5 to 15 years, that most lateral condyle fractures are Milch type 2, and that the direction of dislocation is almost always posteromedial [12, 13]. However, the fracture type in this case was Milch type 1, and the direction of dislocation was posterolateral. Only three cases of the same type of injury have been reported to date [12, 13]. Moreover, our patient’s condition was also complicated by OCFF of the coronoid process; thus, it seems that this case was an extremely rare injury. OCFF was first reported by Rang [14] in 1974, and it was caused by interference between the coronoid process and the trochlea during spontaneous reduction of a dislocated elbow. Only 18 cases have been reported to date [9, 15, 16, 17, 18, 19, 20, 21, 22, 23]; of these cases, 17 involved the ulna and 1 involved the trochlea [17]. In most cases, osteochondral fragments are peeled off from the coronoid process toward the trochlear notch, interfering with the trochlea. In our case, however, the OCFF was probably caused by the coronoid process being affected by the remaining capitellum after posterolateral dislocation. A similar mechanism was reported by Wang and Wang [13]. Because OCFFs have only a few abnormal findings on plain radiographs, they are often difficult to diagnose. In such cases, CT, MRI, or arthrography may be useful. In our case, the diagnosis of OCFF was made based on the lateral dislocation of the elbow, the coronoid process fracture, the irregularity of the ulnar articular surface, and the presence of the coronoid process fragment posterior to the capitellum on CT images. Dislocations of the elbow with lateral condyle fractures and OCFFs are very difficult to diagnose, presenting a major problem in clinical practice. In patients with lateral condyle fractures, it is necessary to differentiate distal humeral epiphyseal separations and T-condylar fractures, and in patients with OCFFs, it is important to avoid missing very small fragments on plain radiographs. It is also important to know that this type of injury exists and to view plain radiographs with vigilance. If the diagnosis is not clear, additional tests such as MRI, CT, and arthrography should be performed. With respect to treatment, the prognoses of both injuries are reported to be good if the fractures are anatomically reduced [9, 13]. Internal fixation may not be mandatory for OCFF; good outcomes have been reported after resection of a small osteochondral fragment located in the ulnohumeral joint [22]. At the very least, however, intra-articular interpositions and inhibitory factors of reduction must be removed, and good gliding and a centripetal position of the joint must be achieved.
We obtained a relatively good outcome of extra-articular corrective osteotomy in an 8-year-old boy with malunion after posterolateral dislocation of the elbow associated with a Milch type 1 lateral condyle fracture of the humerus and OCFF of the coronoid process. Four years postoperatively, the patient obtained 130° of elbow flexion and −30° of extension without restriction of the forearm rotation; however, the fishtail deformity of the trochlea remained. Extra-articular corrective osteotomy could be a choice of treatments for intra-articular malunion of the elbow in children.
In pediatric elbow trauma, the initial diagnosis is most important and improper treatment can be disastrous. If intra-articular malunion remains, extra-articular corrective osteotomy gives relatively good outcomes.
References
- 1.Sharma H, Ayer R, Taylor GR. Complex pediatric elbow injury: An uncommon case. BMC Musculoskelet Disord 2005;6:13. [Google Scholar]
- 2.Bauer AS, Bae DS, Brustowicz KA, Waters PM. Intra-articular corrective osteotomy of humeral lateral condyle malunions in children: Early clinical and radiographic results. J Pediatr Orthop 2013;33:20-5. [Google Scholar]
- 3.Solfelt DA, Hill BW, Anderson CP, Cole PA. Supracondylar osteotomy for the treatment of cubitus varus in children: A systematic review. Bone Joint J 2014;96-B:691-700. [Google Scholar]
- 4.Farr S, Ganger R, Girsch W. Distal humeral flexion osteotomy for the treatment of supracondylar extension-type malunions in children. J Pediatr Orthop B 2018;27:115-20. [Google Scholar]
- 5.Yamamoto I, Ishii S, Usui M, Ogino T, Kaneda K. Cubitus varus deformity following supracondylar fracture of the humerus. A method for measuring rotational deformity. Clin Orthop Relat Res 1985;201:179-85. [Google Scholar]
- 6.Usui M, Ishii S, Miyano S, Narita H, Kura H. Three-dimensional corrective osteotomy for treatment of cubitus varus after supracondylar fracture of the humerus in children. J Shoulder Elbow Surg 1995;4:17-22. [Google Scholar]
- 7.Tang X, Wang J, Slongo T, Wang SY, Ze RH, Zhou R, et al. Comparison of internal fixation vs. External fixation after corrective osteotomy in children with cubitus varus. J Shoulder Elbow Surg 2020;29:845-52. [Google Scholar]
- 8.Feldman DS, Goldstein RY, Kurland AM, Taha AM. Intra-articular osteotomy for genu valgum in the knee with a lateral compartment deficiency. J Bone Joint Surg Am 2016;98:100-7. [Google Scholar]
- 9.Kajiwara R, Ishida O, Sunagawa T, Suzuki O, Sugioka T, Ochi M. Osteochondral flap fracture of the olecranon in a child. J Pediatr Orhtop 2007;27:304-6. [Google Scholar]
- 10.Rasool MN. Dislocations of the elbow in children. J Bone Joint Surg Br 2004;86:1050-8. [Google Scholar]
- 11.Sharma H, Sibinski M, Sherlock DA. Outcome of lateral humeral condylar mass fractures in children associated with elbow dislocation or olecranon fracture. Int Orthop 2009;33:509-14. [Google Scholar]
- 12.Rovinsky D, Ferguson C, Younis A, Otsuka NY. Pediatric elbow dislocation associated with a milch Type 1 lateral condyle fracture of the humerus. J Orthop Trauma 1999;13:458-60. [Google Scholar]
- 13.Wang J, Wang ZL. Osteochondral flap fracture of the coronoid in pediatric humeral lateral condyle. A report of 3 cases. Medicine (Baltimore) 2019;98:e15915. [Google Scholar]
- 14.Rang MC, editor. Dislocations of the elbow joint. In: Children’s Fractures. 1st ed. Philadelphia, PA: Lippincott and Williams; 1974. p. 190. [Google Scholar]
- 15.Blamoutier A, Klaue K, Damsin JP, Carlioz H. Osteochondral fractures of the glenoid fossa of the ulna in children: Review of four cases. J Pediatr Orthop 1991;11:638-40. [Google Scholar]
- 16.Blasier RD. Intra-articular flap fracture of the olecranon in a child. A case report. J Bone Joint Surg Am 1989;71:945-7. [Google Scholar]
- 17.Grant IR, Miller JH. Osteochondral fracture of the trochlea associated with fracture-dislocation of the elbow. Injury 1975;6:257-60. [Google Scholar]
- 18.Kim DC, Cutchen W, Teachey W, Brewer J, Nimityongskul P. Pediatric olecranon osteochondral flap fractures with subtle radiographic abnormality. J Hand Surg Am 2021;46:155.e1-8. [Google Scholar]
- 19.Kowtharapu DN, Thabet AM, Holmes L Jr., Kruse R. Osteochondral flap avulsion fracture in a child with forearm compartment syndrome. Orhopedics 2008;31:805. [Google Scholar]
- 20.Ohta T, Itoh S, Okawa A, Matuyama Y, Shinomiya K. Osteochondral flap fracture of the olecranon with subluxation of the elbow in a child. J Orthop Sci 2010;15:686-9. [Google Scholar]
- 21.Quick TJ, Gibbons P, Smith N. An olecranon chondral flap and osteochondral coronoid fracture in a spontaneously reduced elbow dislocation in a child. J Periatr Orthop B 2013;22:481-5. [Google Scholar]
- 22.Song KS, Jeon SH. Osteochondral flap fracture of the olecranon with dislocation of the elbow in a child: A case report. J Orthop Trauma 2003;17:229-31. [Google Scholar]
- 23.Valisena S, Hamitaga F, Gonzalez JG, Voumard NM, Ciritsis BD, de Rosa V, et al. Osteochondral flap fracture of the coronoid in pediatric elbow dislocation: A case report and literature review. Eur J Orthop Surg Traumatol 2019;29:213-20. [Google Scholar]








