Subchondroplasty may prove to be a novel treatment option for TBME in the healthy adolescent population when conservative treatments fail and AVN risk is minimal.
Dr. Tanner Marriott, Kansas City University - 2901 St Johns Blvd, Joplin 64804, Missouri. E-mail: tanner.marriott@kansascity.edu
Background: Transient bone marrow edema (TBME) is a condition that typically presents in middle-aged adults with a male to female ratio of 3:1. Cases have also been noted in females during the third trimester of pregnancy. Vitamin D deficiency has been linked to this condition as the pathophysiology demonstrates poorly mineralized osteoid in presenting lesions. It is rare for a healthy child or adolescent to present with TBME introducing the purpose of this case study. This case report aims to provide medical and surgical education on TBME in a young and healthy adolescent. To our best knowledge, this is the first report on the use of subchondroplasty to treat transient bone marrow of the navicular in an adolescent male.
Case Presentation: A 16-year-old adolescent male with foot and ankle pain is treated from September of 2017 to September of 2019. The patient failed initial conservative treatments. His treatment concluded with subchondroplasty of the navicular bone, typically contraindicated due to the risk of avascular necrosis (AVN). The patient received follow-up in March of 2020, which included additional magnetic resonance imaging (MRI) for long-term treatment outcome data.
Conclusion: The patient was successfully treated with subchondroplasty after conservative therapy failed. In patients with TBME, subchondroplasty may not be the best option due to risk of AVN. At 1-year follow-up, our patient was asymptomatic and MRI showed reduction in edema.
Keywords: Transient bone marrow edema, bone marrow edema, pediatric bone marrow edema, avascular necrosis, subchondroplasty, case study.
Transient bone marrow edema (TBME) is a condition that most commonly affects a large joint, such as the hip or knee, of middle-aged, and adult males [1]. It is characterized by pain and increased interstitial fluid within the bone marrow. Diagnosing TBME can be challenging as patients typically present with localized pain but no trauma or definable etiology [2]. Most lesions require visualization with magnetic resonance imaging (MRI). However, plain radiographs may reveal osseous demineralization. Transient osteoporosis and regional migratory osteoporosis are typically self-limiting but ruling out more significant or persistent conditions such as avascular necrosis (AVN) is critical for treatment and surgical planning [3]. Both medical and surgical interventions have been utilized in the treatment of TBME. However, conservative treatments are much more common and limited published information is available for alternative treatments when conservative therapies fail. Compression, ice, and non-steroidal anti-inflammatory drugs are usually initiated given the patient’s presentation. Iloprost, a prostacyclin analog, may be used as well as it has shown to provide a significant reduction in pain as well as evidence of bone marrow edema reduction (evaluated through T1-weighted MRI) [4]. Should conservative and medicinal interventions fail, surgical intervention may prove successful. Surgical subchondroplasty is a minimally invasive outpatient surgical procedure in which the surgeon injects synthetic bone material under fluoroscopic guidance. Subchondroplasty injections mimic the physical and chemical properties of normal cancellous bone. The material acts as a placeholder that fills the bone marrow lesion; giving the bone structural support [5]. Over time, homeostatic bone maintenance allows for the conversion of synthetic material to natural bone. Typically, there is significant pain reduction following the procedure and a gradual return to activities. There are limited case reports published concerning bone marrow edema in the pediatric population [6, 7, 8, 9, 10, 11]. Of these limited reports, we failed to find any that used subchondroplasty as a means of treatment after prolonged conservative treatment failure. In this case report, we present an adolescent male patient with a unique case of TBME of the navicular bone. After several years of failed conservative and medicinal treatment, surgical intervention through subchondroplasty was initiated. The patient and his legal guardian provided consent for this retrospective chart review and case report. Our institutional review board exempts all retrospective case reports.
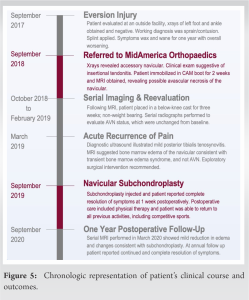
A 16-year-old athletic and white male with no significant medical history presented to an outside facility for foot and ankle pain in September of 2017. The patient described left foot and ankle pain after sustaining an eversion injury secondary to a mechanical fall down a flight of stairs. The outside facility performed a diagnostic workup involving an X-ray of the patient’s foot and ankle. Ultimately, the patient was splinted and sent home with no instruction for provider follow-up after the evaluation. One year later, in September of 2018, the patient was referred to SZ Foot and Ankle Clinic for specialist evaluation due to continued pain. The pain was localized to the arch of his left foot and no longer in his ankle. The patient was concerned because the pain had been negatively affecting his athletic performance. At that time, X-rays were performed (Fig. 1), and the patient was diagnosed with an accessory navicular bone along with insertional tendonitis. MRI was ordered, the patient was given a CAM boot for immobilization, and the patient was instructed to follow-up in 2 weeks. The MRI displayed edema of the tarsometatarsal joints with possible AVN of the navicular bone.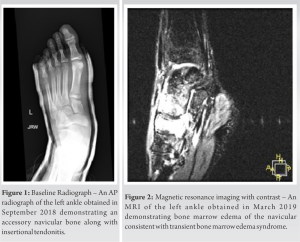
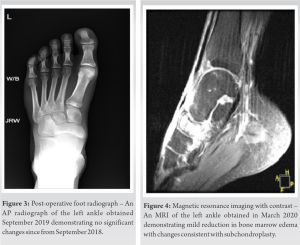
In this case report, we describe a pediatric patient with TBME of the navicular bone who was treated with subchondroplasty after conservative treatment proved unsuccessful. A thorough review of current literature failed to identify pediatric cases of TBME of the navicular bone that were treated in this manner. It is important to note that subchondroplasty is typically contraindicated for the navicular bone due to an increased risk of AVN. This did not prove to be a pertinent concern in this case due to negative MRI and US imaging for AVN. In addition, if the patient did indeed have an AVN, which we did not believe him to have, the injection of subchondroplasty would not have significantly worsened his symptomatology or outcome. The risks and benefits were thoroughly discussed with the patient and his guardian before proceeding with surgery. Possible AVN of the navicular bone was considered while working with this patient. Serial X-rays were performed to evaluate AVN status which remained unchanged from baseline. Over time, it was clear that the patient’s reported symptoms and imaging were inconsistent with AVN. A follow-up MRI with contrast was ordered which suggested bone marrow edema of the navicular consistent with TBME syndrome. Knowing that TBME in a healthy, pediatric patient is rare, it can easily be misdiagnosed as AVN. Furthermore, we recommend including TBME as part of a differential diagnosis for AVN. This also shows that taking a more careful review of the patient’s history, physical, and treatments could ultimately result in resolution of pain. Interestingly, on follow-up after surgical intervention, the MRI from March of 2020 showed resolution of the global edema in the area surrounding the navicular specifically the midfoot where the patient reported most of his pain but the navicular was essentially unchanged from baseline imaging. Nonetheless, the patient reported complete resolution of his symptoms by post-operative day 7. Zimmer-Biomet, the manufacturer of subchondroplasty, currently recommends a follow-up MRI be obtained 3–4 months postoperatively. While this recommendation is given for AVN, we obtained it to both confirm our suspicion of TBME while providing the patient with tangible proof of improvement even though his symptoms were clinically resolved. Of note, the radiologist who read the follow-up MRI commented that it may take longer for the bone to show significant change on imaging. This is consistent with reports by Zimmer-Biomet. Zimmer-Biomet reports that it may take up to 1 year for full resolution to be noted on MRI. This was discussed with the patient and a 1-year post-operative follow-up MRI was offered at no cost. The patient improved 1 week after surgery and was intrinsically better based on reduction of global edema and unchanged navicular lucency. This is a significant improvement after nearly 2 years of pain. In our opinion, the resolution of the patient’s pain, despite minimal change on imaging, speaks to the efficacy of his treatment.
While this case report has limitations, including the off-label use of subchondroplasty and a single patient experience, we believe that it is important to share these findings with the medical community as the clinical and surgical management of this patient could shed light on other young athletes who complain of chronic pain without a justifiable source. TBME is less common in pediatric populations and more research needs to be conducted in this field of study. In this case, the use of subchondroplasty after failed conservative and medicinal intervention proved to be a successful approach. Furthermore, given this patient’s complete resolution of symptoms and improvements on imaging, we believe that it is pertinent to provide other clinicians with this unique case to include TBME as part of their differential diagnosis for AVN and subchondroplasty as a potential treatment option after conservative treatment failure.
Subchondroplasty may prove to be a novel treatment option for TBME in the healthy adolescent population when conservative treatments fail and AVN risk is minimal.
References
- 1.Korompilias AV, Karantanas AH, Lykissas MG, Beris AE. Bone marrow edema syndrome. Skeletal Radiol 2009;38:425-36. [Google Scholar]
- 2.Bonadio MB, Filho AG, Helito CP, Stump XM, Demange MK. Bone marrow lesion: Image, clinical presentation, and treatment. Magn Reson Insights 2017;10. [Google Scholar]
- 3.Korompilias AV, Karantanas AH, Lykissas MG, Beris AE. Transient osteoporosis. J Am Acad Orthop Surg 2008;16:480-9. [Google Scholar]
- 4.Hörterer H, Baumbach SF, Gregersen J, Kriegelstein S, Gottschalk O, Szeimies U, et al. Treatment of bone marrow edema of the foot and ankle with the prostacyclin analog iloprost. Foot Ankle Int 2018;39:1183-91. [Google Scholar]
- 5.Pelucacci LM, LaPorta GA. Subchondroplasty: Treatment of bone marrow lesions in the lower extremity. Clin Podiatr Med Surg 2018;35:367-71. [Google Scholar]
- 6.De Houwer H, Van Beek N, Prinsen S, Van Riet A, De Roeck J, Verfaillie S. Bone marrow edema syndrome of the foot and ankle in a paediatric population: A retrospective case series with serial MRI evaluation. J Child Orthop 2020;14:440-50. [Google Scholar]
- 7.Pay NT, Singer WS, Bartal E. Hip pain in three children accompanied by transient abnormal findings on MR images. Radiology 1989;171:147-9. [Google Scholar]
- 8.Aigner N, Petje G, Schneider W, Krasny C, Grill F, Landsiedl F. Juvenile bone-marrow oedema of the acetabulum treated by iloprost. J Bone Joint Surg Br 2002;84-B:1050-2. [Google Scholar]
- 9.Kröger L, Arikoski P, Komulainen J, Seuri R, Kröger H. Transient bone marrow edema in a child. Ann Rheum Dis 2004;63:1528-9. [Google Scholar]
- 10.Joshi V, Hermann G, Balwani M, Simpson WL. Painless transient bone marrow edema syndrome in a pediatric patient. Skeletal Radiol 2014;43:1615-9. [Google Scholar]
- 11.Orr JD, Sabesan V, Major N, Nunley J. Painful bone marrow edema syndrome of the foot and ankle. Foot Ankle Int 2010;31:949-53. [Google Scholar]