Consider Morel-Lavallée lesions in pediatric patients with bruising if a remote history of trauma is present.
Dr. Kailey A Remien, Department of Medical Education, Akron Children’s Hospital, 1 Perkins Square, Akron, Ohio 44308. E-mail: kremien@akronchildrens.org
Introduction: A Morel-Lavallée lesion (MLL) is a closed degloving injury secondary to shearing forces. MLL is a rare, easily overlooked diagnosis, especially in those without recent trauma or fracture. Patients will present with ecchymosis, edema, fluctuance, and skin hypermobility or tightness. We present a case of pediatric MLL that was initially challenging to diagnose as the inciting trauma was 2 months before her diagnosis.
Case Report: A 14-year-old girl presented with 5 days of left leg bruising, swelling, and pain. Two months prior, she collided with another softball player’s cleat and developed a hairline fracture. Magnetic resonance imaging of the left lower extremity (LLE) showed a closed, soft-tissue degloving injury, and she was diagnosed with a MLL. Throughout her admission, she had improvement in her bruising but continued to have pain with ambulation that was somewhat alleviated with the use of a compression stocking. Pediatric Orthopedic Surgery and Interventional Radiology were consulted, and a conservative approach was recommended with 3 months of LLE compression.
Conclusion: MLL typically occurs in patients in their 30–40 s and rarely occurs in children. Identifying MLL in children is essential as children are more susceptible to shock and multi-organ damage from blunt trauma than adults. They are also more vulnerable to fractures and deep organ injuries. In the setting of MLL, children can quickly develop hypovolemic shock due to lower blood volumes and necrosis secondary to mass effect in the dead space. MLL should be included on the differential for children with trauma or a history of a shearing injury.
Keywords: Pediatrics, orthopedics, bruising, trauma.
A Morel-Lavallée lesion (MLL) is a closed degloving injury due to the separation of the hypodermis from the fascia secondary to shearing forces [1, 2]. It is typically a secondary effect of high-energy trauma, such as a sports injury or motor vehicle accident [3]. About 25% of patients with MLL were involved in a car accident and many concurrently had a nearby fracture [4]. MLL is a rare diagnosis, especially in those without recent trauma or fracture [4]. A degloving injury leads to disruption of lymphatic and vascular structures, causing hemolymphatic fluid to exsanguinate into the soft-tissue envelope. This creates space between the two planes. The fluid contents and inflammatory cascade perpetuate the fluid collection due to increasing permeability and osmotic gradient in the fluid collection. The local inflammatory cascade leads to the formation of a fibrous pseudocapsule filled with blood products, debris, fibrin, and necrosed fatty tissue [4, 5].
A 14-year-old girl presented to the emergency department with left the lower extremity (LLE) bruising, swelling, and pain. 2 months prior, during a softball game, she collided with another player’s cleat and that day was diagnosed with a hairline fracture of the left tibial diaphysis with an overlying hematoma. She followed up with orthopedic surgery in the outpatient setting, participated in physical therapy for several weeks, and received clearance to resume sports 6 weeks before the current presentation. Six days before this presentation, she participated in two softball games. She denied any significant trauma or sliding events during these games. The next day (5 days before presentation), she woke up with pain and bruising of her left lateral shin. She treated the associated pain with ibuprofen. This was the 1st time; she took non-steroidal anti-inflammatory drugs in the past 2 months. Over the following days, the pain and bruising worsened and she developed edema of the LLE. She presented again to the emergency department with significant pain, requiring morphine. She was mildly hypertensive, secondary to pain, with otherwise normal vitals. Her examination was notable for extensive bruising, pain with light palpation or weight-bearing, and edema of the left calf (Fig. 1). No erythema, abrasions, or skin tightness was noted. Distal dorsalis pedis pulses were 2/4 and equal bilaterally. Dorsiflexion and plantar flexion of the ankle caused moderate distress secondary to calf pain, but she had full range of motion in all joints. Homan sign was negative. Laboratory studies, including complete blood count, complete metabolic panel, prothrombin time, partial thromboplastin time, creatinine kinase, C-reactive protein, lactate dehydrogenase, and uric acid, were within normal limits for age. Frontal and lateral X-rays of the left lower leg demonstrated anterior, and medial and lateral subcutaneous soft-tissue edema of the proximal and mid leg (Fig. 2).
No erythema, abrasions, or skin tightness was noted. Distal dorsalis pedis pulses were 2/4 and equal bilaterally. Dorsiflexion and plantar flexion of the ankle caused moderate distress secondary to calf pain, but she had full range of motion in all joints. Homan sign was negative. Laboratory studies, including complete blood count, complete metabolic panel, prothrombin time, partial thromboplastin time, creatinine kinase, C-reactive protein, lactate dehydrogenase, and uric acid, were within normal limits for age. Frontal and lateral X-rays of the left lower leg demonstrated anterior, and medial and lateral subcutaneous soft-tissue edema of the proximal and mid leg (Fig. 2).  An ultrasound image demonstrated complex fluid collection in the lateral subcutaneous soft tissues (Fig. 3) which prompted further workup with magnetic resonance imaging (MRI) with and without contrast. She was admitted to the Pediatric Hospital Medicine service for further workup, including MRI, and management. While on the acute care medical floor, the patient’s LLE was closely monitored without any significant changes in examination, including girth (Fig. 4). The patient stated that she had regular periods; on her heaviest day, she uses three to four pads but does not bleed through them. She denied any history of epistaxis but has a distant relative with an unknown bleeding disorder. She denied abdominal pain, headache, fever, easy bruising, weight loss, petechiae, and fatigue.
An ultrasound image demonstrated complex fluid collection in the lateral subcutaneous soft tissues (Fig. 3) which prompted further workup with magnetic resonance imaging (MRI) with and without contrast. She was admitted to the Pediatric Hospital Medicine service for further workup, including MRI, and management. While on the acute care medical floor, the patient’s LLE was closely monitored without any significant changes in examination, including girth (Fig. 4). The patient stated that she had regular periods; on her heaviest day, she uses three to four pads but does not bleed through them. She denied any history of epistaxis but has a distant relative with an unknown bleeding disorder. She denied abdominal pain, headache, fever, easy bruising, weight loss, petechiae, and fatigue. 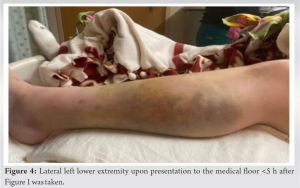 The differential diagnosis included hematologic and oncologic causes such as hematoma, coagulopathies, platelet disorders, and leukemia. Orthopedic etiologies included trauma, bursitis, compartment syndrome, or fat necrosis. Medication-induced ecchymosis and alcohol abuse were also considered [4, 5, 6]. MRI of the LLE was notable for a MLL (Fig. 5) along with some soft-tissue inflammation concerning for cellulitis. On the day of discharge, she had improvement in her bruising (Fig. 6) but continued to have pain with ambulation that was somewhat alleviated with the use of a compression stocking. Pediatric Orthopedic Surgery and Interventional Radiology were consulted and recommended a conservative approach with 3 months of LLE compression. Her cellulitis was treated with 7 days of clindamycin.
The differential diagnosis included hematologic and oncologic causes such as hematoma, coagulopathies, platelet disorders, and leukemia. Orthopedic etiologies included trauma, bursitis, compartment syndrome, or fat necrosis. Medication-induced ecchymosis and alcohol abuse were also considered [4, 5, 6]. MRI of the LLE was notable for a MLL (Fig. 5) along with some soft-tissue inflammation concerning for cellulitis. On the day of discharge, she had improvement in her bruising (Fig. 6) but continued to have pain with ambulation that was somewhat alleviated with the use of a compression stocking. Pediatric Orthopedic Surgery and Interventional Radiology were consulted and recommended a conservative approach with 3 months of LLE compression. Her cellulitis was treated with 7 days of clindamycin.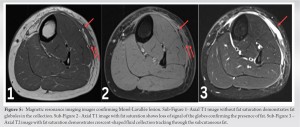 At her 1-week outpatient follow-up with orthopedics, she reported improvement in her pain, edema, and bruising, and she was able to ambulate without difficulty. She continued to use acetaminophen for pain, elevate her leg after exercise, and wear her compression stocking as advised. Both sclerotherapy and consultation with pediatric plastic surgery were deferred due to her marked improvement.
At her 1-week outpatient follow-up with orthopedics, she reported improvement in her pain, edema, and bruising, and she was able to ambulate without difficulty. She continued to use acetaminophen for pain, elevate her leg after exercise, and wear her compression stocking as advised. Both sclerotherapy and consultation with pediatric plastic surgery were deferred due to her marked improvement.
Patients with MLL will present with ecchymosis, edema, fluctuance, and skin hypermobility or tightness [1]. Symptoms are impacted by the patient’s body habitus, location of the fluid collection, and rate of accumulation. MLL typically presents within a few days following a precipitating trauma. The most common location for MLL is the greater trochanter (>60% of cases), hip, and thigh due to the large surface area, skin mobility, and dense capillary network [4]. Calf and lower leg injuries are rare and only seen in 1.5% of MLL incidents [1]. The preferred imaging modality for diagnosis is MRI to accurately depict the size, location, shape, and contents; however, clinical diagnosis can be made, especially in the setting of significant trauma [4]. Ultrasound is a quick and safe way to identify if the lesion is deep to the hypodermis and superficial to the muscle plane [2]. Computed tomography is of little utility in MLL as it commonly goes unrecognized [7]. Treatment is dependent on the size and severity of the lesions as well as proximity to a coinjury or surgical site. Options include debridement and irrigation, percutaneous drainage, and observation [1]. Early surgical intervention can be performed to remove necrotic tissue to decrease the chance of infection. Bacterial colonization occurs in over 45% of sampled lesion fluid [1]. Lesions with capsules typically do not resolve without surgical intervention [2]. Small lesions may resolve with a percutaneous approach, but some may need serial drainage [1]. If a small lesion without a capsule is noted, a conservative approach utilizing compression bandaging is appropriate. If the lesion returns or does not improve, drainage is required. Sclerodesis, a process where a sclerosing agent (such as doxycycline) is injected into a lesion with the intent of causing fibrosis, has also been successfully used as a treatment modality for MLL [4]. MLL typically occurs in patients in their 30–40 s and rarely occurs in children [8]. We present a case of MLL that was initially challenging to diagnose as the inciting trauma was 2 months prior to her presentation. In the limited literature of pediatric MLL, there is little information regarding pediatric MRI findings, making diagnosis more difficult [9]. One study found that there were <20 documented pediatric MLL cases [10]. The anterior knee has been documented to be the most affected joint identified in pediatric MLL cases on MRI and is most often associated with sports traumas [9]. Identifying MLL in children is essential as children are more susceptible to shock and multi-organ damage from blunt trauma than adults [8]. They are also more vulnerable to fractures and deep organ injuries as their skeletons are still developing and they are more susceptible to fascial layer separation [9]. In the setting of MLL, children can quickly develop hypovolemic shock due to lower blood volumes and necrosis secondary to mass effect in the dead space. These lesions can be fatal [11]. MLL should be included on the differential for children with trauma or a history of a shearing injury [8].
A MLL is a rare closed degloving injury that most often occurs after trauma but may occur spontaneously as well. It is not well-documented or diagnosed in the pediatric population and should be on the differential for significant bruising, as MLL can be fatal. Identifying MLL in children is essential as children are more susceptible to shock and multi-organ damage from blunt trauma than adults [8]. MLL should be considered if MRI findings support the presence of separation of the hypodermis and subdermal fat from the underlying fascia. There are no treatment guidelines for pediatric MLL, although multiple treatment modalities have been described, ranging from conservative management to invasive surgical intervention.
Children are at high risk of deterioration from degloving injuries; as such, MLL should be on the differential when significant bruising is present, even if the history of trauma is remote.
References
- 1.Scolaro JA, Chao T, Zamorano DP. The Morel-Lavallée lesion: Diagnosis and management. J Am Acad Orthop Surg 2016;24:667-72. [Google Scholar]
- 2.Nair AV, Nazar P, Sekhar R, Ramachandran P, Moorthy S. Morel-Lavallée lesion: A closed degloving injury that requires real attention. Indian J Radiol Imaging 2014;24:288-90. [Google Scholar]
- 3.Kushare I, Ghanta RB, Wunderlich NA. Morel-Lavallée lesions (internal degloving injuries) of the lower extremity in the pediatric and adolescent population. Phys Sportsmed 2021;49:182-6. [Google Scholar]
- 4.Agrawal U, Tiwari V. Morel Lavallee Lesion. 2022. https://www.ncbi.nlm.nih.gov/books/NBK574532/#:~:text=Morel%20Lavallee%20lesions%20are%20soft. [Last accessed on 2022 Jun 28]. [Google Scholar]
- 5.Ballas M, Kraut EH. Bleeding and bruising: A diagnostic work-up. Am Fam Physician 2008;77:1117-24. [Google Scholar]
- 6.Christian D, Leland HA, Osias W, Eberlin S, Howell L. Delayed presentation of a chronic Morel-Lavallée lesion. J Radiol Case Rep 2016;10:30-9. [Google Scholar]
- 7.McKenzie GA, Niederhauser BD, Collins MS, Howe BM. CT characteristics of Morel-Lavallée lesions: An under-recognized but significant finding in acute trauma imaging. Skeletal Radiol 2016;45:1053-60. [Google Scholar]
- 8.Rha EY, Kim DH, Kwon H, Jung SN. Morel-lavallee lesion in children. World J Emerg Surg 2013;8:60. [Google Scholar]
- 9.Rapp JB, Barrera CA, Ho-Fung VM. Morel-Lavellée lesions: MRI characteristics in the pediatric patient. Pediatr Radiol 2019;49:559-65. [Google Scholar]
- 10.Shelley J, Noritake A, Ortiz K, Ricca R. Morel-Lavallee lesion in pediatric trauma. Pediatr Surg Int 2017;33:921-4 [Google Scholar]
- 11.Rashid A, Singh MK, Feng SS, Yatim NM, Sahak MY, Mahmud R. Lethal Morel-Lavallée lesion: A forensic radiology-pathology correlation. Radiol Case Rep 2020;15:1280-4. [Google Scholar]









