In patients with isolated tuberculous involvement of posterior spinal elements having normal neurology, even with a large abscess, early intervention with antitubercular therapy can be of benefit in selected cases as it reduces further instability, deformity, and late complications of surgery.
Dr. Sumit Kumar, FNB Spine, Central Institute of Orthopedics, VMMC and Safdarjung Hospital, New Delhi, India. E-mail: drsumit26@gmail.com
Introduction: Tuberculosis of posterior spinal elements or neural arch tuberculosis is a rare clinical entity. We report a patient with isolated tuberculosis of the C5 spinous process and reformation of destroyed spinous process in response to antitubercular therapy (ATT). This is first case report of the kind to the best of our knowledge.
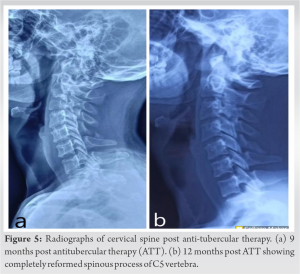
Case Report: A young male aged 22 years presented to us with a slow-growing, painful lump for the past 3 months accompanied by a discharging sinus at the back of his neck. Plain radiograph and computed tomography scan showed destruction of the C5 spinous process. Magnetic resonance imaging cervical spine showed presence of abscess in addition to the above finding. The patient underwent incision and drainage of abscess followed by local injection of streptomycin. CB-NAAT (Gene Xpert) and histopathological examination confirmed the diagnosis of tuberculosis. The patient responded to ATT very well. The C5 spinous process which was destroyed by the disease process was seen to have gradually reformed on serial radiographs.
Conclusion: Isolated posterior spinal tuberculosis is rare, but it must be thought of as a differential diagnosis in suitable cases. Diseased tissue in tuberculosis has high healing potential in response to medical therapy, thus avoiding the need of radical debridement.
Keyword: Spinal tuberculosis, spinous process, neural arch, laminectomy.
Spinal tuberculosis usually presents as a paradisiacal lesion commonly involving two adjacent vertebral body end plates and the intervening intervertebral disk. Tuberculosis of posterior spinal elements or neural arch tuberculosis is a rare clinical entity, caused by the same Mycobacterium tuberculosis (MTB) that causes usual tubercular spine. An incidence of lower than 2% in non-endemic regions and between 5 and 10% in endemic regions has been reported [1, 2, 3]. Isolated tuberculosis of the spinous process is a rare entity and only few cases have been reported [4, 5]. We report a patient with isolated tuberculosis of C5 spinous process, who presented with a posterior cervical lump. The C5 spinous process which was destroyed by disease process fully reformed in response to antitubercular therapy (ATT). To the best of our knowledge, no such case has been reported till date.
A young male aged 22 years presented to the hospital with a slow-growing, lump in the posterior neck region for the past 3 months, which was painful and accompanied with a discharging sinus and associated with weight loss, fever, and anorexia. His vitals, general physical evaluation, as well as systemic evaluation including a clinical examination of the chest, abdomen, and lymph nodes were all normal. Local examination revealed well-defined swelling of five cm by 6 cm size on midline of back of neck. The swelling was smooth, tender to touch, and fluctuant with overlying draining sinus. No neurological deficit, sensory, or motor was noted. Blood investigations showed raised erythrocyte sedimentation rate (ESR) (55 mm/h) and elevated C-reactive protein (CRP) (24 mg/L). The plain cervical radiograph showed destruction of the C5 spinous process without any involvement of vertebral body or disk space (Fig. 1).
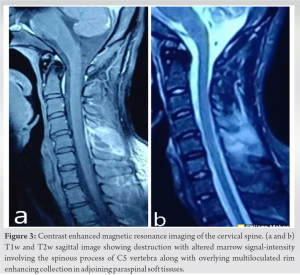
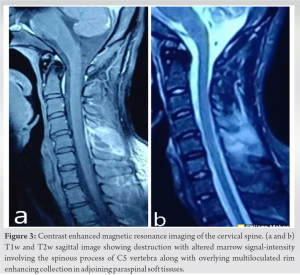
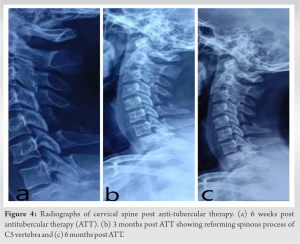
Spinal tuberculosis is the most common form of skeletal tuberculosis and accounts for nearly half of all cases of bone and joint tuberculosis [4]. Isolated posterior element spinal tuberculosis is uncommon and it involves pedicle, lamina, facet joints, spinous process, and transverse process in isolation or in combination. Isolated spinous process tuberculosis in cervical spine is even rarer. Shamim et al. reported a case of isolated tubercular affection of the spinous process of the C2 vertebra [5]. We did a thorough research and found that isolated involvement of C5 spinous process has not been reported in the literature. The earliest reports of isolated posterior complex tuberculosis were by Naim-ur-Rahman et al., in 1979, who presented case series of 13 patients with atypical spinal tuberculosis, of which five patients had isolated neural arch tuberculosis [6]. In a case series reported in 1984 by Babhulkar et al., all 22 patients with tuberculosis of posterior elements of vertebrae had cold abscess and neurological involvement [1]. Kumar, in 1985, reported case series on 27 such cases and proposed a classification system [2]. Narlawar et al., in 2002, elaborated on the MRI findings in 33 patients with isolated neural arch tuberculosis and concluded that MRI is very useful in detecting the extent of involvement and response to antitubercular treatment [7]. In 2012, Arora et al. presented a case series of 24 consecutive patients with neural arch tuberculosis [8]. They found that such patients had a high incidence of neurological deficit at presentation. In 2020, Boruah et al. evaluate MRI finding in 19 cases of posterior spinal tuberculosis [9]. Lumbar vertebra was involved in maximum number of cases in their study and pedicle involvement was the most common followed by that of the lamina. However, none of them reported isolated involvement of spinous process in any of their subjects. Like any other bone and joint TB, neural arch tuberculosis is usually secondary to primary tubercular lesion elsewhere in the body. Implantation of tubercular bacteria is through the hematogenous route. The venous plexus around the spinous, transverse, articular process, and posterior to the lamina, which anastomoses freely with neighboring venous plexuses help the infection to reach and affect the posterior elements [10]. Usually, the pedicles and laminae are the most affected areas. Clinically, posterior spinal tuberculosis is notorious for causing early neurological symptoms of compressive myelopathy. It is because that the tubercular debris gets mechanically pushed into the spinal canal. Radiographs are not always helpful in diagnosing posterior spinal tuberculosis. Babhulkar et al. found positive X-ray finding(s) in only 10% of cases with posterior element tuberculosis [1]. CT scan provides better osseous detail, while MRI shows the affection of the soft tissue and pus formation and has even greater value in evaluating spinal cord compression and in finding intramedullary lesions. Diagnosis of posterior spinal tuberculosis is based on the combination of clinical, imaging, and other laboratory investigation including AFB staining/culture, CB-NAAT, and histopathological examination. Although spinal tuberculosis is a medical disease and ATT has the main role in the recovery, still, if the patient does not get better or the condition worsens clinically after 6 to 8 weeks, surgical decompression should be performed. Due to high risk of neurological deterioration in posterior spinal tuberculosis, excisional surgery in the form of laminectomy with debridement is recommended. This not only helps in de-bulking of the lesion but also allows removal of extradural granuloma, if present. In our case, the spinous process of C5 vertebra which was not visible on radiographs due to destruction by the disease process got reformed after a few months of ATT. It was seen to be gradually reappearing on serial follow-up radiographs, and ultimately, the native anatomy of the spinous process was restored. This demonstrates the healing potential of diseased tissues in spinal tuberculosis and the ability of precursor cells residing in periosteum to reform bone even in adults. This is also in line with the practice of avoiding radical debridement in tubercular spine cases, even if surgery is necessary (decompression of neural elements as necessary, drainage of abscesses, and minimal debridement) as bone can reform from the diseased tissues once the disease starts healing. Hence, patients with isolated tuberculous involvement of posterior spinal elements having normal neurology, even with a large abscess, early intervention with ATT can be of benefit in selected cases as it reduces further instability, deformity, and late complications of surgery.
Although rare, posterior element spinal tuberculosis should always be suspected in patient presenting with posterior spinal abscess in endemic regions. Diseased tissue in tuberculosis has high healing potential in response to medical therapy and radical debridement of diseased tissue can be avoided.
Tuberculosis of isolated spinous process is a rarely reported condition, and conservative treatment with antitubercular drugs can be rewarding and may lead to reconstitution of bony anatomy even in cases with complete destruction of the spinous process.
References
- 1.Babhulkar SS, Tayade WB, Babhulkar SK. Atypical spinal tuberculosis. J Bone Joint Surg Br 1984;66:239-42. [Google Scholar]
- 2.Kumar K. A clinical study and classification of posterior spinal tuberculosis. Int Orthop 1985;9:147-52. [Google Scholar]
- 3.Abdelwahab IF, Camins MB, Hermann G, Klein MJ. Vertebral arch or posterior spinal tuberculosis. Skeletal Radiol 1997;26:737-40. [Google Scholar]
- 4.Bloch AB, Rieder HL, Kelly GD, Cauthen GM, Hayden CH, Snider DE. The epidemiology of tuberculosis in the United States. Semin Respir Infect 1989;4:157-70. [Google Scholar]
- 5.Shamim MS, Tahir MZ, Jooma R. Isolated tuberculosis of C2 spinous process. Spine J 2009;9:e30-2. [Google Scholar]
- 6.Naim-Ur-Rahman, Jamjoom A, Jamjoom ZA, Al-Tahan AM. Neural arch tuberculosis: Radiological features and their correlation with surgical findings. Br J Neurosurg 1997;11:32-8. [Google Scholar]
- 7.Narlawar RS, Shah JR, Pimple MK, Patkar DP, Patankar T, Castillo M. Isolated tuberculosis of posterior elements of spine: Magnetic resonance imaging findings in 33 patients. Spine (Phila Pa 1976) 2002;27:275-81. [Google Scholar]
- 8.Arora S, Sabat D, Maini L, Sural S, Kumar V, Gautam VK, et al. Isolated involvement of the posterior elements in spinal tuberculosis: A review of twenty-four cases. J Bone Joint Surg Am 2012;94:e151. [Google Scholar]
- 9.Boruah DK, Gogoi BB, Prakash A, Lal NR, Hazarika K, Borah KK. Magnetic resonance imaging evaluation of posterior spinal tuberculosis: A cross-sectional study. Acta Radiol 2021;62:1035-44. [Google Scholar]
- 10.Batson OV. The function of the vertebral veins and their role in the spread of metastases. Ann Surg 1940;112:138-49. [Google Scholar]