The treatment of osteomyelitis often requires reconstruction for bone and soft-tissue defects, thereby necessitating the orthoplastic approach involving plastic surgery and orthopedic techniques.
Dr. Tomohiro Yasuda, Department of Orthopaedic Surgery, Showa University Fujigaoka Hospital, Yokohama, Japan. E-mail: shapedbytomo@gmail.com
Introduction: Post-traumatic osteomyelitis (OM) is often caused by Staphylococcus aureus. However, occasionally, it is caused by an infection with a rare bacterium. A case of OM caused by Aeromonas hydrophila was first reported in 1975. Since then, only nine cases have been reported, making it a rare disease. Here, we report a case of rare A. hydrophila OM that developed following open tibial fracture (classified as Gustilo–Anderson 3B) caused by an injury in a river.
Case Report: The patient was a 50-year-old male who got injured in a river and was diagnosed with open tibial fracture. Debridement in the first surgery happened at a leisurely pace. Purulent discharge from the wound persisted despite external fixation; however, no bacterium was detected in the bacterial culture. The patient underwent multiple debridement procedures; A. hydrophila was detected in the bone marrow. Despite the appropriate administration of antibacterial drugs and debridement, infection persisted until radical bone resection and tissue reconstruction were performed. In the present case, OM following an open fracture caused by an injury in a river was suspected, which was caused by the rare bacterium A. hydrophila.
Conclusion: In cases of OM occurring after underwater trauma, A. hydrophila should be considered as a causative pathogen. In addition, in cases of post-traumatic OM accompanied by bone and soft-tissue defects, the orthoplastic approach is required.
Keywords: Aeromonas hydrophila, osteomyelitis, reverse sural artery flap.
Osteomyelitis (OM) may be accompanied by soft-tissue defects, and its treatment requires bone reconstruction and soft-tissue reconstruction. Post-traumatic OM is often caused by Staphylococcus aureus infection [1]. However, OM can occasionally be caused by the infection with a rare bacterium. Infection associated with water injuries often occurs among fishermen and travelers following exposure to freshwater and seawater. Aeromonas infection is one of the infections associated with water injuries. The Aeromonas species are Gram-negative bacilli that thrive in aquatic environments [2]. For treating OM with soft-tissue defects following open fractures such as infected Gustilo-Anderson 3B fractures, it is important to simultaneously perform soft-tissue and bone reconstructions. Orthoplastic surgery should be the treatment strategy considered. Here, we report a case of A. hydrophila OM that developed following an open tibial fracture (Gustilo-Anderson 3B) caused by an injury in a river.
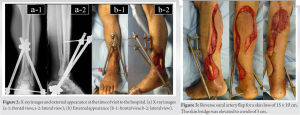
The patient was a 50-year-old male, who was a smoker. He got injured after falling into a river while staying in Thailand. He was rescued from the river 8 h after injury and was then transported to a hospital in Thailand. X-ray examination revealed left distal tibial diaphyseal and epiphyseal fractures (classified as AO/OTA type 43C3.3) (Fig. 1).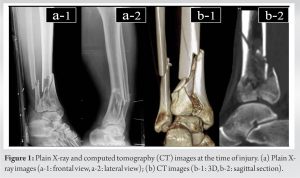
Surgery
The patient experienced a tibial distal epiphyseal fracture accompanied by a skin loss of 15 × 10 cm and infection. He was diagnosed as a case of infected Gustilo–Anderson 3B tibial fracture. We decided to treat it with a multistage management approach involving the three procedures of serial debridement, wound closure flap surgery, and bone reconstruction.
Serial debridement
Emergency surgery was performed 27 days after injury. The surgery was performed under general anesthesia with the patient in the prone position. Surgery was performed without using a tourniquet.
Wound closure flap surgery (reverse sural artery flap surgery)
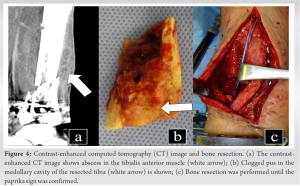
Wound closure flap surgery was performed on the same day as serial debridement. To cover the outer open wound at the distal lower leg, we performed reverse sural artery flap (RSAF) surgery. For the skin loss of 15 × 10 cm, a skin flap that was 1 cm larger in size was designed. Using Doppler echocardiography, peroneal artery perforator was confirmed at two positions – at 5 and 7 cm from the tip of the lateral malleolus. The center of the skin flap was aligned with the line of the medial sural cutaneous nerve and lesser saphenous vein, and the distal skin bridge was aligned with the peroneal artery perforator. Skin incision was made from the proximal side, the medial sural cutaneous nerve and lesser saphenous vein were confirmed, and the median superficial sural artery between deep gastrocnemius muscles was confirmed and included in the skin flap. For the lateral side, the lateral sural nerve was included in the skin flap. To manage venous congestion, a skin bridge of 3 cm was attached (Fig. 3). The skin flap was engrafted without congestion or partial necrosis. At 6 weeks after injury, redness in the lower limb and a sensation of heat in the skin of the lower leg appeared. Contrast-enhanced computed tomography revealed abscess accumulation in the tibialis anterior muscle. We suspected OM (Fig. 4a) and planned to perform bone resection of the infected tibia and bone reconstruction using a ring external fixator.
Debridement and bone reconstruction (through the surgical technique of ring external fixation)
Debridement and bone reconstruction surgeries were performed 7 weeks after the injury. During the surgery, the wound was opened from the skin flap suture. Bone resection was performed from the bone to the site where bleeding was observed (paprika sign) using a bone saw (Fig. 4b, c). The tibia was fixed with a ring external fixator. In the resected tibia, pus was observed in the medullary cavity, whereas blood flow was not observed (Fig. 4b). Aeromonas hydrophila was detected from the medullary cavity. The patient was diagnosed with OM caused by A. hydrophila. Poly(methyl methacrylate) mixed with 10% vancomycin was injected into the bone defect site (Fig. 5a). Following the surgery, vancomycin and clindamycin were intravenously administered for 2 weeks.
Course
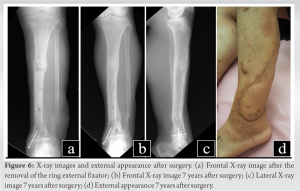
The bone defect site resected owing to OM was reconstructed through the bone transport method using a ring external fixator (Fig. 5b, c, d). The bone was moved at a rate of 1 mm/day. At 4 months after surgery, the bone was healed and the ring external fixator was removed (Fig. 6a). External fixation period was 360 days, bone extension amount was 5 cm, and the healing index (day/cm) was 72.2. At the final follow-up examination 7 years after surgery, there was no relapse of infection, and ankle range of motion was 5° of dorsiflexion and 35° of plantar flexion (Fig. 6b, c, d). The patient could walk without pain and has resumed work. The American Orthopaedic Foot and Ankle Society score was 93 points.
The incidence of post-traumatic fracture-related infections (FRIs) differs depending on the degree (grade and type) of fractures. FRIs include deep infection, OM, and osteitis. Of these, OM is difficult to treat. Therefore, treatment for post-traumatic OM is costly and time-consuming. In the present case, OM occurred following an open tibial fracture, accompanied by soft-tissue and bone defects.
A. hydrophila and OM
Overall, 37.5% of the cases of post-traumatic OM are caused by S. aureus [1]. However, in the present case, we encountered OM caused by a rare bacterium, A. hydrophila. There have been 9 reports including 12 cases of post-traumatic OM caused by this bacterium (Table 1) [3, 4, 5, 6, 7, 8, 9, 10, 11]. In 11 cases (91.6%), the site that was infected and developed OM was the lower limb. Infection caused by A. hydrophila is one of the infections associated with water injuries. Among the 12 cases of OM caused by A. hydrophila, 8 cases involved trauma associated with rivers, lakes, and seas. In the present case, the patient developed A. hydrophila OM following an injury in a river in Thailand. One of the reasons was that bacteria were identified in the bone marrow and were not sufficiently debrided. The Aeromonas species was first reported as the cause of post-traumatic OM in 1975. It was tibial OM; however, the treatment and its outcome were not reported [3]. The second report was presented by Blatz in 1979. It was a case of OM caused by A. hydrophila associated with open tibial fracture. To control the infection, above-the-knee amputation was performed [4]. Further, in a report by Weinstock et al. and Karam et al., the affected limb was preserved. Partial resection was performed; however, bone reconstruction was not performed [5, 6]. Dubey et al. reported a case of A. hydrophila OM in the forearm. For treatment, bone resection and bone reconstruction were not performed, and it developed into chronic OM [7]. Bonatus and Alexander reported the occurrence of A. hydrophila OM following surgery for closed pilon fracture. Reconstruction with gracilis free flap for soft-tissue defect was reported. Bone graft was performed for bone defect. However, bone resection was not performed for the lesion site of OM [8]. Gunasekaran et al. performed bone resection for the lesion site of OM but did not perform bone reconstruction [10]. The treatment principles for OM were lesion resection and reconstruction. Karam et al. and Gunasekaran et al. performed lesion resections [6, 10]. Meanwhile, only Bonatus and Alexander performed reconstruction [8]. In the present case, we performed both lesion resection and reconstruction for soft-tissue and bone defects.
Reverse sural artery flap surgery
In the present case, substantial skin loss (15 × 10 cm) was observed, and free skin flap or pedunculated skin flap was considered. For free skin flap, the anterolateral thigh flap would be an option. However, compared with RSAF, free skin flap requires microsurgical techniques and the surgery is time-consuming. We confirmed the median superficial sural artery and peroneal artery perforator through pre-operative echocardiography and determined whether RSAF surgery was possible. Complications of RSAF surgery, such as post-operative congestion and partial necrosis, reportedly occur in 14.8% of the cases. Moreover, the incidence of necrosis in cases undergoing RSAF surgery is reportedly 5.1% [12]. In the present case, the skin loss was substantial, and there was a concern regarding the occurrence of post-operative congestion and necrosis in RSAF surgery. Considering the large size of the skin flap, to prevent congestion, a skin bridge was attached and RSAF was elevated. This method was reported by Sugg et al.; they prevented post-operative congestion using a skin bridge of 4 cm [13]. In the present case, a 3-cm wide skin bridge was used, and the skin flap was engrafted without congestion or partial necrosis.
Treatment of an infected Gustilo–Anderson 3B fracture
There is a standard therapy for the management of open tibial fractures. Antibiotic administration, debridement, and fracture fixation are to be performed in the early stage. However, in the present case, treatment was delayed, and the patient underwent surgery 2 days after injury. We believe that this could be the reason for the co-occurrence of deep infection and OM. OM treatment may require bone resection depending on the extent of infection. Therefore, reconstruction is often required for soft-tissue and bone defects. Treatment for open fracture, OM, and tumors require the orthoplastic approach that involves plastic surgery and orthopedic techniques [14]. In the present case, the orthoplastic approach was performed by an orthopedic surgeon alone. In 2012, Yusof et al. reported treating infected Gustilo-Anderson 3B fractures through three stages – serial debridement, wound closure flap surgery, and bone reconstruction. All 11 cases healed without infection relapse, and satisfactory outcomes were reported [15]. In the present case, the patient was treated using the multistage management approach that includes serial debridement, wound closure flap surgery, and bone reconstruction, which was similar to that reported by Yusof and Halim [15]. When the patient was referred to our hospital, debridement was performed, and the bone was reconstructed by bone lengthening using RSAF surgery for soft-tissue reconstruction and ring external fixation for bone reconstruction. It was considered to be an effective treatment with no infection relapse in the 7 years after surgery.
A. hydrophila is rarely reported but it may cause OM or soft-tissue infection following underwater trauma. In cases of OM occurring after underwater trauma, A. hydrophila should be considered as a causative pathogen. When accompanied by soft-tissue defect, OM caused by trauma should be treated using the multistage management approach that includes serial debridement, wound closure flap surgery, and bone reconstruction.
OM caused by A. hydrophila is rare. In cases of OM following underwater trauma, A. hydrophila should be considered as a causative pathogen during treatment.
References
- 1.Peng J, Ren Y, He W, Li Z, Yang J, Liu Y, et al. Epidemiological, clinical and microbiological characteristics of patients with post-traumatic osteomyelitis of limb fractures in Southwest China: A hospital-based study. J Bone J Infect 2017;2:149-53. [Google Scholar]
- 2.Centers for Disease Control (CDC). Aeromonas wound infections associated with outdoor activities – California. MMWR Morb Mortal Wkly Rep 1990;39:334-5, 341. [Google Scholar]
- 3.Stephen S, Rao KN, Dumar MS, Indrani R. Letter: Human infection with Aeromonas species: Varied clinical manifestations. Ann Intern Med 1975;83:368-9. [Google Scholar]
- 4.Blatz DJ. Open fracture of the tibia and fibula complicated by infection with Aeromonas hydrophila. A case report. J Bone Joint Surg Am 1979;61:790-1. [Google Scholar]
- 5.Weinstock RE, Bass SJ, Lauf E, Sorkin BA. Aeromonas hydrophilia: A rare and potentially life-threatening pathogen to humans. J Foot Surg 1982;21:45-53. [Google Scholar]
- 6.Karam GH, Ackley AM, Dismukes WE. Posttraumatic Aeromonas hydrophila osteomyelitis. Arch Intern Med 1983;143:2073-4. [Google Scholar]
- 7.Dubey L, Krasinski K, Hernanz-Schulman M. Osteomyelitis secondary to trauma or infected contiguous soft tissue. Pediatr Infect Dis J 1988;7:26-34. [Google Scholar]
- 8.Bonatus TJ, Alexander AH. Posttraumatic Aeromonas hydrophila osteomyelitis. Orthopedics 1990;13:1158-63. [Google Scholar]
- 9.Gold WL, Salit IE. Aeromonas hydrophila infections of skin and soft tissue: Report of 11 cases and review. Clin Infect Dis 1993;16:69-74. [Google Scholar]
- 10.Gunasekaran L, Ambalkar S, Samarji RA, Qamruddin A. Post-traumatic osteomyelitis due to Aeromonas species. Indian J Med Microbiol 2009;27:163-5. [Google Scholar]
- 11.Agrawal S, Srigyan D, Nag HL, Kapil A, Dhawan B. Chronic osteomyelitis by Aeromonas hydrophila: A silent cause of concern. J Lab Physicians 2017;9:337-9. [Google Scholar]
- 12.Schmidt K, Jakubietz M, Meffert R, Gilbert F, Jordan M, Jakubietz R. The reverse Sural artery flap- how do modifications boost its reliability? A systematic analysis of the literature. JPRAS Open 2020;26:1-7. [Google Scholar]
- 13.Sugg KB, Schaub TA, Concannon MJ, Cederna PS, Brown DL. The reverse superficial Sural artery flap revisited for complex lower extremity and foot reconstruction. Plast Reconstr Surg Glob Open 2015;3:e519. [Google Scholar]
- 14.Khan U, Kelly MB, Pleat J, Chesser TJ. Orthoplastics: An integral evolution within comprehensive trauma care. Injury 2011;42:969-71. [Google Scholar]
- 15.Yusof NM, Halim AS. Outcomes of infected grade IIIB open tibial fractures. Singapore Med J 2012;53:591-4. [Google Scholar]