Primary repair with non-absorbable sutures utilizing a Krackow configuration on distal traumatic Achilles tendon lacerations near the insertion site in pediatric patients is a safe and effective method of repair for this uncommon injury presentation.
Dr. Michael Anthony Supanich, Department of Orthopaedics, Mclaren Macomb Hospital-Michigan State University 1000 Harrington Blvd. Mount Clemens, Michigan 48043. E-mail: michael.supanich@mclaren.org
Introduction: Acute Achilles tendon ruptures in the pediatric population are an uncommon occurrence and there is currently limited literature with regard to this injury. Further, there is limited data evaluating traumatic lacerations of the distal substance of the Achilles tendon near the insertion site and its management, as opposed to the more common cited location of rupture at the mid-substance of the tendon. This case is the first known article to specifically address primary repair with non-absorbable sutures utilizing a Krackow configuration at this level in this patient population.
Case Report: A case of a 10-year-old male who sustained a traumatic distal Achilles tendon laceration near the insertion site who was successfully treated with primary repair with non-absorbable sutures utilizing a Krackow configuration is presented. This repair technique demonstrated return to full functional ankle plantar and dorsiflexion with return to pre-injury level of activity.
Conclusion: This case report highlights that primary repair with non-absorbable sutures utilizing a Krackow configuration on distal traumatic Achilles tendon lacerations near the insertion site in pediatric patients is a safe and effective method of repair for this uncommon injury presentation.
Keywords: Traumatic, pediatric, Achilles, case report.
An acute Achilles tendon rupture is a rare injury to occur in the pediatric patient. Conversely, this injury is relatively common in adults, specifically with elite and recreational athletes [1]. The average age for rupture is between 30 and 40 years old in males and females alike [2]. Often, the injury is associated with an explosive plantar flexion maneuver [1] or forced dorsiflexion of the ankle [2]. The rupture most commonly occurs in the midsubstance of the tendon, coinciding with a watershed region 2–6 cm from the Achilles insertion point [3]. Both surgical and non-operative interventions with functional rehab have proven to be effective modes of treatment in the adult population. Due to the rarity of a child sustaining such an injury, much less is known about the appropriate treatment methods within the pediatric population. There is only a limited number of case reports highlighting an Achilles rupture and/or laceration in this subset of patients. In addition, there are no studies addressing a traumatic laceration at the distal aspect of the tendon near the insertion point of the Achilles tendon. Our case study will highlight the surgical and postoperative interventions that were employed in treating a pediatric patient who suffered a traumatic distal Achilles tendon laceration near the insertion site.
A 10-year-old boy and his older brother were having a dispute at their home. As the argument escalated, the older brother retaliated by throwing a ceramic bowl in the direction of his brother. The bowl hits the ground, shattered, and lacerated the posterior aspect of the 10-year-old’s left ankle. He was subsequently brought to our hospital’s Emergency Department where he was evaluated by the orthopedic service. On examination, there was a positive Thompson test as well as a 5 × 2 cm wound with gross visualization of the ruptured Achilles tendon. The laceration was thoroughly irrigated, and antibiotics were provided upon arrival. The patient was admitted and maintained on perioperative antibiotics. He was taken to the operating room the following morning. He was placed in the prone position and the laceration site (Fig. 1) was once again thoroughly irrigated and debrided. A longitudinal incision incorporating the traumatic laceration was then made overlying the length of the Achilles tendon (Fig. 2).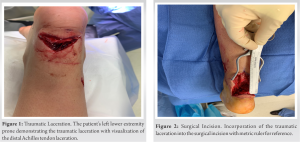 The rupture was identified at the distal tendon near the tendon’s insertion site. The proximal aspect of the tendon was mobilized followed by minimal debridement, as to allow adequate approximation of both the proximal and distal ends. FiberTape Suture (Arthrex AR-9200-16s) was then placed through the proximal and distal portions of the tendon in typical Krackow fashion (Fig. 3). The free ends of the FiberTape were then tied together, approximating the Achilles tendon. A free needle was then utilized to oversew the remaining limbs of the FiberTape around the medial and lateral borders of the tendon before cutting the ends of the suture (Fig.4).
The rupture was identified at the distal tendon near the tendon’s insertion site. The proximal aspect of the tendon was mobilized followed by minimal debridement, as to allow adequate approximation of both the proximal and distal ends. FiberTape Suture (Arthrex AR-9200-16s) was then placed through the proximal and distal portions of the tendon in typical Krackow fashion (Fig. 3). The free ends of the FiberTape were then tied together, approximating the Achilles tendon. A free needle was then utilized to oversew the remaining limbs of the FiberTape around the medial and lateral borders of the tendon before cutting the ends of the suture (Fig.4). The ankle was brought through plantar and dorsiflexion to ensure no gapping occurred at the repair site. The wound was once again irrigated and closed in a layered fashion. A short leg fiberglass cast was molded to the patient’s left lower extremity in roughly 30° of plantar flexion. He was discharged to home on oral antibiotics (Keflex 250 mg TID) secondary to the traumatic wound. The patient was treated non-weight bearing in his cast for 4 weeks. He was then transitioned to a walking boot with heel wedges and allowed to weight bear as tolerated. One heel wedge per week was removed over a course of 4 weeks. At 8-week post-operative, he was transitioned to a normal shoe but instructed to refrain from running, sports, and aggressive play. At the 1-year follow-up visit (Fig. 5), the patient demonstrated 10° and 45° of ankle dorsi and plantar flexion, respectively. Motor grading was found to be 5/5 with regard to ankle dorsi and plantar flexion.
The ankle was brought through plantar and dorsiflexion to ensure no gapping occurred at the repair site. The wound was once again irrigated and closed in a layered fashion. A short leg fiberglass cast was molded to the patient’s left lower extremity in roughly 30° of plantar flexion. He was discharged to home on oral antibiotics (Keflex 250 mg TID) secondary to the traumatic wound. The patient was treated non-weight bearing in his cast for 4 weeks. He was then transitioned to a walking boot with heel wedges and allowed to weight bear as tolerated. One heel wedge per week was removed over a course of 4 weeks. At 8-week post-operative, he was transitioned to a normal shoe but instructed to refrain from running, sports, and aggressive play. At the 1-year follow-up visit (Fig. 5), the patient demonstrated 10° and 45° of ankle dorsi and plantar flexion, respectively. Motor grading was found to be 5/5 with regard to ankle dorsi and plantar flexion.
The incidence of a traumatic Achilles tendon rupture and/or laceration in pediatric patients is rare. What makes our case even more unique is that the laceration occurred at the distal aspect of the tendon near the insertion point. This location is more distal than any other injury described in current literature. Several publications were reviewed in an attempt to identify the success or failure of relatively similar injuries in the pediatric population. Two separate case reports identified incidences of traumatic Achilles ruptures in patients who previously underwent Ponseti casting and Achilles tenotomies for congenital clubfeet. The first case involved a 15-year-old female who suffered a midsubstance tear of her right Achilles tendon while sprinting. Similar to our case, she was treated surgically through primary repair of the tendon utilizing non-absorbable sutures in a Krackow configuration. Postoperatively, she was splinted for 2 weeks in resting equinus and then transitioned into a walking boot with a large heel wedge. Over the course of 4 weeks, the heel wedge was gradually reduced in size. By 4 months post-operatively, she had returned to full activity [4]. The second case report involved a 16-year-old male who suffered complete midsubstance Achilles tendon tears on either leg, two years apart from one another. In both cases, as with our patient, he was treated with primary repair of the tendon utilizing a Krackow configuration. Postoperatively, the patient was immobilized in plantar flexion for 4 weeks and remained non-weight-bearing for a total of 8 weeks. A full recovery was achieved in both circumstances with the patient returning to full activity approximately 1 year from each procedure [5]. Vasileff and Moutzouros discussed a case involving a 10-year-old hockey player who sustained a partial laceration of his Achilles by an opponent’s skate blade [6]. The initial injury to the tendon was missed until 6 weeks later when a forced dorsiflexion event led to completion of the partial tear at the myotendinous junction. He was treated surgically with primary repair of the tendon using non-absorbable suture in a modified Bunnell pattern. Similar to our case, the tendon periphery was also oversewn to further improve alignment of the tendon ends. He was immobilized in a cast for 5 weeks with 30° knee flexion and the ankle in neutral alignment. He was then transitioned to an AFO with dorsiflexion limited to 10° and was permitted to fully weight bear. At 5.5 months, he had returned to light skating exercises and achieved a complete return to activity and sport by 8 months. Wurzer et al. present a case report involving a 15-year-old female who was in a motorcycle accident and suffered injuries to the right lower extremity consisting of a bimalleolar ankle fracture and a partial Achilles tendon tear with an overlying 10 × 6 cm soft-tissue defect [7]. The soft-tissue injury was sustained secondary to a burn from the exhaust pipe. The patient initially underwent irrigation and debridement of the wound followed by surgical fixation of the bimalleolar ankle fracture. In addition, she underwent an Achilles reconstruction with a plantaris autograft and temporary coverage of the heel wound with paraffin gauze. Two additional surgeries were required to close the soft-tissue defect consisting of a temporoparietal fascial flap connected to the posterior tibial branches and a full-thickness skin autograft from the left groin. Immobilization was utilized for 4 weeks. Gradual weight-bearing began at week 5 under the guidance of a physiotherapist. At 1 year from her index procedure, the patient had achieved 15° dorsiflexion and 40° plantarflexion with no complaints or concerns regarding her right ankle. Our case exemplifies one possible strategy in treating a traumatic distal Achilles tendon tear near the insertion site. As mentioned above, prior case reports have also utilized non-absorbable sutures to remedy more proximal tendon ruptures involving the midsubstance and myotendinous regions. Similar to these other cases, a course of immobilization in fixed plantar flexion with eventual transition to some form of walking boot with removable heel wedges proved to be an effective means to achieve a successful, gradual return to baseline activity level. To our knowledge, there has only been one published case study highlighting the non-operative treatment of a 7-year-old girl who sustained a traumatic Achilles rupture at the myotendinous junction. She was immobilized for 6 weeks in plantar flexion before being permitted to weight bear as tolerated without any device. She was reported to have had resumed regular activity 1 month later without complications [8]. Despite her successful outcome, there have been no comparative studies in the pediatric population evaluating operative versus non-operative intervention for traumatic Achilles tendon tears. In the adult population, non-operative treatment combined with functional rehabilitation has demonstrated no significant differences in rerupture rates when compared to operative treatment [9]. Similar findings were further supported by Renninger et al. in their study of active-duty military members, with the exception that operatively treated soldiers were able to return to duty approximately 1.5 months earlier [10]. Given this evidence, further research is needed to explore the possibility of non-operative treatment in the pediatric population. If found effective, it may limit health-care costs and limit complications associated with surgery.
Traumatic distal Achilles tendon rupture near the insertion site in the pediatric population is an uncommon injury presentation with limited depth of literature into its management. We feel that primary repair with non-absorbable sutures utilizing a Krackow configuration is an effective and safe method of repair that allowed for full return to the patient’s previous level of activity.
Primary repair with non-absorbable sutures utilizing a Krackow configuration for a traumatic distal Achilles tendon rupture near the insertion site provided a safe and effective treatment option in this pediatric patient.
References
- 1.Miller MD, Thompson SR. Achilles tendon injuries. In: DeLee D, editors. Miller’s Orthopaedic Sports Medicine. 5th ed., vol. 2. Philadelphia, PA: Elsevier; 2020. p. 1476. [Google Scholar]
- 2.Azar FM, Beaty JH, Daugherty K, Jones L, Campbell WC. Rupture of Achilles tendon. In: Campbell’s Operative Orthopaedics. 13th ed., Vol. 3. Philadelphia, PA: Elsevier; 2021. p. 2415-6. [Google Scholar]
- 3.Hess GW. Achilles tendon rupture: A review of etiology, population, anatomy, risk factors, and injury prevention. Foot Ankle Spec 2010;3:29-32. [Google Scholar]
- 4.Egger AC, Levine AD, Mistovich RJ. Acute rupture of Achilles tendon in an adolescent with a history of Ponseti casting and Achilles tenotomy. JBJS Case Connector 2019;9:e0197. [Google Scholar]
- 5.Aretakis AC, Georgopoulos G Sequential bilateral Achilles tendon rupture in a teenager after Ponseti treatment for bilateral clubfoot.. JBJS Case Connector 2021;11(2) doi: 10.2106/JBJS.CC.20.00929. [Google Scholar]
- 6.Vasileff WK, Moutzouros V. Unrecognized pediatric partial Achilles tendon injury followed by traumatic completion: A case report and literature review. J Foot Ankle Surg 2014;53:485-8. [Google Scholar]
- 7.Wurzer P, Eberl R, Kamolz LP, Parvizi D, Rappl T, Spendel S. Aesthetically and functionally satisfying reconstruction of an Achilles tendon and overlying skin defect in a 15 year old girl: A case report. Burns 2015;41:e1-3. [Google Scholar]
- 8.Eidelman M, Nachtigal A, Katzman A, Bialik V. Acute rupture of Achilles tendon in a 7-year-old girl. J Pediatr Orthop B 2004;13:32-3. [Google Scholar]
- 9.Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, Fowler P, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures. J Bone Joint Surg 2010;92:2767-75. [Google Scholar]
- 10.Renninger CH, Kuhn K, Fellars T, Youngblood S, Bellamy J. Operative and nonoperative management of Achilles tendon ruptures in active duty military population. Foot Ankle Int 2015;37:269-73. [Google Scholar]








