Managements of intertrochanteric fracture with posterior fracture requires immediate open reduction and internal fixation to avoid delay and thus reduce the chances of AVN of femoral head.
Dr. Pranav Gupta, Department of Orthopaedics, Guru Gobind Singh Medical College and Hospital, Faridkot, Punjab, India. E-mail: pranavchd88@gmail.com
Introduction: High-energy trauma has increased the incidence of traumatic hip dislocation and dislocation is often associated with fractures. However, a hip fracture-dislocation extending to the ipsilateral femoral trochanter is exceedingly rare and only a few cases have been described. We report a case of irreducible posterior dislocation of the hip with ipsilateral intertrochanteric fracture managed by open reduction and osteosynthesis.
Case Report: A 50-year-old male presented with a history of fall from an electricity pole with pain in the left hip and an inability to bear weight on his left lower limb. Radiographs confirmed the presence of posterior dislocation of the left hip with comminuted intertrochanteric fracture on the same side.
Conclusion: Posterior dislocation of the hip with same side inter trochanteric fracture is a rare traumatic entity, with only few case being reported. Literature does not provide any classification for such rare traumatic fracture dislocation. Management of such fracture requires early diagnosis and intervention which can result in good prognosis.
Keywords: Avascular necrosis, intertrochanteric fracture, Pipkin classification, posterior dislocation, proximal femoral nailing.
Increases in high-energy road traffic accidents have also increased the incidence of traumatic hip dislocation which is often associated with fractures which commonly include fractures of the femoral head, neck, shaft, or posterior acetabular wall [1, 2]. However, a hip fracture-dislocation extending to the ipsilateral femoral trochanter is exceedingly rare and only a few cases have been described [3, 4, 5, 6, 7]. The most commonly used classification of this injury is the Thompson and Epstein and its subset the Pipkin classification [2]. However, this classification does not include posterior dislocation of the hip with associated ipsilateral intertrochanteric fracture or other complex fracture patterns. We there fore report a case of irreducible posterior dislocation of the hip with ipsilateral comminuted intertrochanteric fracture managed by open reduction and internal fixation. The case is being reported not only because of its rarity but also to emphasize that with increase in high-energy trauma, these fracture patterns would be more common and there is a need to review the existing classifications so that these fractures are better categorized and treatment guidelines defined. Consent of the patient was taken for data being used for publication.
A 50-year-old male presented in emergency with a history of fall from electricity pole with pain in left hip and an inability to bear weight on his left lower limb. On examination, there was tenderness on the left greater trochanteric region and inability to actively raise the left lower limb. The radiographs confirmed the presence of comminuted intertrochanteric fracture with posterior dislocation of the hip. CT scan with 3D reconstruction was also done (Fig. 1).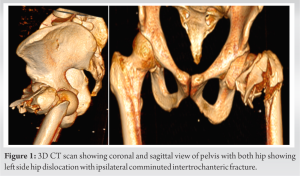 We applied skin traction. The patient did not have any comorbid conditions. An attempt of closed reduction was taken in emergency, but it failed. The patient was planned for surgery within 12 h of injury. The patient was taken under general anesthesia in a lateral position. Closed reduction was attempted with Schanz pin inserted into the neck of femur under c-arm guidance and manipulated to reduce the dislocation (Fig. 2).
We applied skin traction. The patient did not have any comorbid conditions. An attempt of closed reduction was taken in emergency, but it failed. The patient was planned for surgery within 12 h of injury. The patient was taken under general anesthesia in a lateral position. Closed reduction was attempted with Schanz pin inserted into the neck of femur under c-arm guidance and manipulated to reduce the dislocation (Fig. 2).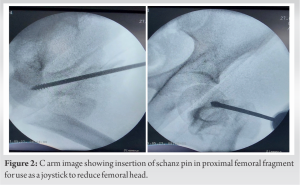 The dislocation was not getting reduced, so we decided for open reduction through posterior approach. We found that the head had buttonholed through a small rent in the posterior capsule and the short external rotators and greater trochanter were also fractured. The femoral head was successfully reduced by gentle traction and manipulation with Schanz pin inserted into the proximal fragment along with pushing the femoral head from the posterior aspect towards the acetabulum (Fig. 3).
The dislocation was not getting reduced, so we decided for open reduction through posterior approach. We found that the head had buttonholed through a small rent in the posterior capsule and the short external rotators and greater trochanter were also fractured. The femoral head was successfully reduced by gentle traction and manipulation with Schanz pin inserted into the proximal fragment along with pushing the femoral head from the posterior aspect towards the acetabulum (Fig. 3). Post reduction, inter-trochanteric fracture was reduced and reduction was held with sharp reduction forceps. Since it was the unstable type of intertrochanteric fracture with associated greater trochanteric fracture, we did proximal femoral nailing in lateral position and fixed fractured greater trochanter with the ethibond no.5 (Fig. 4).
Post reduction, inter-trochanteric fracture was reduced and reduction was held with sharp reduction forceps. Since it was the unstable type of intertrochanteric fracture with associated greater trochanteric fracture, we did proximal femoral nailing in lateral position and fixed fractured greater trochanter with the ethibond no.5 (Fig. 4). On post-operative day 1, X-rays were done and the patient was allowed bedside sitting (Fig. 5). The patient was allowed non-weight bearing walking with the help of a walker on day 2 and was discharged on postoperative day 5. At 2 weeks’ follow-up, suture removal was done. The patient was on regular follow-up for 1 year after the surgery. The patient was allowed partial weight bearing 3 months after surgery and full weight bearing was started at 6 months. At every follow-up, we did a radiological evaluation to look for union and also evaluated Harris’’s hip score. The patient was followed up for 3 years at which there was complete union and there were no signs of AVN on X-ray (Fig. 6).
On post-operative day 1, X-rays were done and the patient was allowed bedside sitting (Fig. 5). The patient was allowed non-weight bearing walking with the help of a walker on day 2 and was discharged on postoperative day 5. At 2 weeks’ follow-up, suture removal was done. The patient was on regular follow-up for 1 year after the surgery. The patient was allowed partial weight bearing 3 months after surgery and full weight bearing was started at 6 months. At every follow-up, we did a radiological evaluation to look for union and also evaluated Harris’’s hip score. The patient was followed up for 3 years at which there was complete union and there were no signs of AVN on X-ray (Fig. 6). Also at 3 years’ follow-up, the patient can squat and sit cross-leg comfortably and do adduction and internal rotation at the hip joint of operated side without any difficulty (Fig. 7).
Also at 3 years’ follow-up, the patient can squat and sit cross-leg comfortably and do adduction and internal rotation at the hip joint of operated side without any difficulty (Fig. 7).
Posterior dislocation of the hip with associated ipsilateral intertrochanteric fracture has been very infrequently described in the literature. Traumatic hip dislocations are a result of high-energy trauma [1]. Associated fractures of the intertrochanteric region have limited incidence and may indicate even more severe injury [8]. Zhen in his article described the mechanism of this injury that posterior dislocation of the hip resulted from a continuous axial force on the hip joint with the limb in flexion, adduction, and internal rotation and the displaced intertrochanteric fracture of the femur resulted from either a second force directly acting on the greater trochanter or an indirect force in the form of rotation when the femoral head is fixed in position by the posterior joint capsule and ischiofemoral ligament [1]. The most important thing in this fracture is how to reduce and whether closed reduction should be attempted in an emergency or we should go for open reduction at first. A few case reports mentioned about attempting closed reduction with axial traction in emergency, but failed. Agarwal et al. in their study reported a case of hip dislocation with ipsilateral intertrochanteric fracture in which he tried closed reduction using schanz pin as a joystick but it did not get reduced and later did open reduction and fixation through lateral approach [9]. Chotai et al. in their study also reported a case with a similar fracture pattern in which they tried closed reduction with axial traction under anesthesia but failed and later did open reduction through a lateral approach [10]. Ul Haq et al. in their study reported two cases of hip dislocation with an ipsilateral intertrochanteric fracture where open reduction and internal fixation were done in both the cases after closed reduction failed [2]. In the present study, we also tried percutaneous method of closed reduction using schanz pin as joystick with but failed and later through the posterior approach, we found femoral head buttonholed through a small rent in the posterior capsule and the short external rotators, so did open reduction and internal fixation with proximal femoral nail 2. DHS was not used as intertrochanteric fracture was unstable and comminuted. Furthermore, proximal femoral nailing reduces operative time as well as soft-tissue dissection thus decreasing the time of surgery and increasing the chances of union. The osteonecrosis rate has been reported to be 4.8% if the reduction was done within 6 h of injury compared with 53% if reduction was delayed for more than 6 h [11]. Displaced femoral intertrochanteric fractures along with dislocation of the hip have a higher risk of avascular necrosis of the femoral head due to damage to the retinacular vessels at the time of injury [8]. In a study by Ul Haq et al. one case was 5 days old injury treated with DHS and another was 1-day-old injury treated with DCS after closed reduction failed in both the cases, but at 1 year follow-up, AVN was not present [2]. In the present study also, the patient was operated on within 12 hrs of injury. At 1 year follow-up, radiographs of the hip showed normal anatomy without signs of avascular necrosis of the femoral head which could be because of partly intact posterior and superior portion of the capsule or not subjecting the patient to MRI investigation, yet a possibility of avascular necroses cannot be ruled out in follow-up of longer duration. Furthermore, at 1 year after the injury, the patient had only terminal restriction of range of motion compared to his normal hip.
Thus, intertrochanteric fracture with posterior dislocation of the hip is a rare traumatic entity, with only few case reports and it does not fit into the present classification systems described for hip dislocation injuries. Therefore, present classification system should be reviewed to include such a pattern of injury. Management of such fracture requires immediate open reduction and internal fixation to avoid delay and thus reduce the chances of AVN of the femoral head. Furthermore, long-term follow-up is essentially required in such cases before making a diagnosis for avascular necrosis.
Hip dislocation with intertrochanteric fracture must be included in the present classification system so that it would provide guidance to future surgeons in managing this type of injury and such injuries should be managed without delay to avoid long-term complications.
References
- 1.Zhen P. Traumatic posterior hip dislocation with an ipsilateral comminuted femoral intertrochanteric fracture: A case report. Orthop Surg 2013;5:219-21. [Google Scholar]
- 2.Ul Haq R, Kumar J, Dhammi IK, Jain AK. Posterior dislocation of hip with ipsilateral intertrochanteric fracture: A report of two cases. Indian J Orthop 2016;50:571-6. [Google Scholar]
- 3.Sahin V, Karakaş ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: A long-term follow-up study. J Trauma 2003;54:520-9. [Google Scholar]
- 4.Pipkin G. Treatment of grade IV fracture-dislocation of the hip. J Bone Joint Surg Am 1957;39-A:1027-42. [Google Scholar]
- 5.Maini L, Mishra P, Jain P, Upadhyay A, Aggrawal A. Three part posterior fracture dislocation of the hip without fracture of the femoral head: Review of literature and a case report. Injury 2004;35:207-9. [Google Scholar]
- 6.Singh R, Sharma SC, Goel T. Traumatic inferior hip dislocation in an adult with ipsilateral trochanteric fracture. J Orthop Trauma 2006;20:220-2. [Google Scholar]
- 7.Korovessis P, Droutsas P, Spastris P, Christodoulou G. Anterior dislocation of the hip associated with fracture of the ipsilateral greater trochanter. A case report. Clin Orthop Relat Res 1990;253:164-7. [Google Scholar]
- 8.Desai KB, Dhamangaonkar AC. A case of posterior HIP dislocation with intertrochanteric fracture: Beware of the sharp calcar spike. J Clin Orthop Trauma 2019;10:975-80. [Google Scholar]
- 9.Agarwal R, Rai A, Saraf S, Singh S, Singh A. An unusual pattern of posterior dislocation of hip associated with comminuted trochanteric fracture. Internet J Orthop Surg 2008;9:1-4. [Google Scholar]
- 10.Chotai PN, Ebraheim NA, Hart R, Wassef A. Concomitant posterior hip dislocation, ipsilateral intertrochanteric-and proximal tibial-fractures with popliteal artery injury: A challenging trauma mélange. Clin Pract 2015;5:776 [Google Scholar]
- 11.Canale ST, Beaty JH. In: Canale ST, editor. Traumatic Hip Dislocations in Children. Vol. 3. Amsterdam: Elsevier; 2013. p. 1438-40. [Google Scholar]









