Early diagnosis and complete surgical excision with radical synovectomy are crucial for the treatment of PVNS in rare locations like ankle joint.
Dr. Nihar Ranjan Mishra, Department of Orthopedics Institute of Medical Sciences and Sum Hospital, Siksha ‘O’ Anusandhan University, Bhubaneswar, Odisha, India. E-mail: nihar.ranjan.litu@gmail.com
Introduction: Pigmented villonodular synovitis (PVNS)is a very uncommon lesion that involves the synovium of joints, tendon sheaths, or bursae. Approximately 2.5% of cases occur around the ankle. PVNS was earlier considered to be a synovial malignancy. Complete surgical excision is curative if bony destruction is not there. Radiotherapy is rarely helpful for residual lesions.
Case Report: We share a case report on PVNSof ankle in a 22-yearsold male patient. Clinical diagnosis was confirmed with the help of magnetic resonance imaging and histopathology.A surgical excision with synovectomy was carried out. Therewere no signs of recurrence in 1.5 years follow-up.
Conclusion: Complete surgical excision with radical synovectomy is crucial for the treatment of PVNS in rare locations like the ankle joint.
Keywords: Pigmented villonodular synovitis,anisonucleosis, synovectomy.
Pigmented villonodular synovitis (PVNS) is a rare benign inflammatory condition of unknown origin involving synovium of the joints first reported in 1941 by Jaffe et al. [1]. They described it as a tumor-like aggression of the synovial tissue involving joints. Basically, PVNS may be localized or diffuseand may be either intra or extra-articular [2]. PVNS around the ankle region is very rare and can result in wide spread lesion and bony destruction [3, 4]. Both localized and diffuse forms have been described around the ankle. PVNS, which originally was believed to be a low-grade malignancy of synovium, is now considered a benign tumor. Most cases are monoarticular. They may present as a simple painless nodule or swelling to a diffusely painful, stiff joint. MRI is the most useful modality for diagnosis besides clinical examination and radiograph. Surgical excision is the treatment of choice in most cases. The diffuse variants generally require total synovectomy to prevent recurrence. Recurrences are usually treated with radiotherapy [5]. In this case report, we share our experience of managing a case of PVNS of the ankle joint in a young adult which was successfully managed by complete surgical excision and synovectomy.
A 22-years old male patient came to our outpatient department with chief complaints of 18-month history of slowly increasing the left posterolateral ankle swelling and pain. The pain was insidious in onset, gradually progressive, and deep-seated throbbing in nature which increased with walking and relieved with rest and analgesics. There was no history of recent trauma, chronic fever, or any other joint pain. Examination revealed palpable firm tender swelling with irregular borders and ill-defined margin around the left ankle just posterior to the lateral malleolus. Range of motion and stability of the ankle were normal. Radiographs showed no apparent bony or articular abnormality. Ultrasound (USG) of the swelling was done which showed findings of heterotropic thickening (5.0 * 3.5), posterior to peroneus tendon extending into the ankle joint. Contrast-enhanced MRI showed lobulated outlines altered signal intensity lesion showing blooming foci in susceptibility-weighted angiography, heterogeneous avid contrast enhancement in posterior aspect of the ankle joint with synovial thickening and mild collection in posterior subtalar joint that was reported as PVNS or synovial sarcoma. FNAC of the swelling was done in which cytosmears were moderately cellular and showed predominantly osteoclastic giant cells admixed with many single scattered cells. Also seen were few spindle-shaped fibroblast-like cells and many mononuclear seven binucleated cells exhibiting mild anisonucleosis, inconspicuous nucleoli with mostly round to oval eccentrically placed nucleoli with abundant cytoplasm. Occasional pigment-laden macrophages were also noted. The features were suggestive of giant cell containing tumor. USG guided synovial biopsy was performed to rule out malignancy which revealed a fairly circumscribed tumor with hyperplastic synovial lining & comprised of nodules of pale & bland appearing mononuclear cells, plenty of osteoclastic giant cells, foamy cells & scattered hemosiderin laden macrophages with areas of hemorrhage that was conclusive of PVNS of left ankle . Through posterolateral approach, we thoroughly resected the mass, along with the synovium Fig. 1, with care to avoid peroneal tendon injury.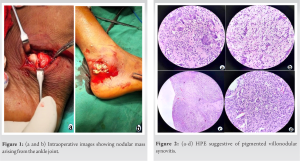 The synovial tissue was hold with an allis forcep and radical synovectomy was ensured by through debridement using electro-cautery. The histopathological findings of the excised tissue were corresponding to those of the biopsy specimen Fig. 2 A short leg slab was applied for 2 weeks after surgery, and then the patient was allowed for graded ankle range-of-motion exercises and weight-bearing. During the final follow-up (18 months following surgery), there was no significant pain or any limitation of ankle range of motion and the patient seemed happy with the outcome Fig. 3.
The synovial tissue was hold with an allis forcep and radical synovectomy was ensured by through debridement using electro-cautery. The histopathological findings of the excised tissue were corresponding to those of the biopsy specimen Fig. 2 A short leg slab was applied for 2 weeks after surgery, and then the patient was allowed for graded ankle range-of-motion exercises and weight-bearing. During the final follow-up (18 months following surgery), there was no significant pain or any limitation of ankle range of motion and the patient seemed happy with the outcome Fig. 3. The preoperative & 1 month follow up x-rays is shown in Fig. 4 & 5 respectively.
The preoperative & 1 month follow up x-rays is shown in Fig. 4 & 5 respectively.
PVNS is a rare tumor, even rarer to occur in the region of foot and ankle. There is still controversy regarding the bony involvement, but the pressure from the lesion is considered to be the primary etiology resulting in joint destruction [6, 7]. The MRI & findings in PVNS suggests alobulated or multinodular masses extending from the joint with low signal intensity on both T1- and T2-weighted images, suggestive of hemosiderin deposits[7, 8]. Similar findings may also be seen in osteoarthritis, rheumatoid arthritis, & hemophillia and should be excluded from the study[7]. The optimal treatment for PVNS is surgical excision [9]. Complete resection and total synovectomy are necessary to prevent recurrence. Considering its aggressive nature and the chance of recurrence, PVNS is a difficult disease to manage especially when it occurs in foot and ankle region where complete excision is difficult to achieve [10,11]. In our case, the lesion was localized to the posterior aspect of the left ankle joint. There was negligible bony involvement. Hence, complete synovectomy and excision of the tumor were successful. If bony involvement would have occurred, curettage with/without bone grafting to fill the bony gap would have been a good option. Similarly in case of articular involvement, arthrodesis of the joint may sometimes is required in case of severe destruction.
PVNS is a rare tumor involving ankle joint. However, complete surgical excision and synovectomy provide excellent results in the early stage.
PVNS rarely involves ankle joint. The most common symptoms are swelling and pain. USG of the affected part, FNAC, and contrast-enhanced MRI are helpful in diagnosing the condition. Bony involvement is rare but should be excluded from the study. Biopsy is investigation of choice. Complete excision with radical synovectomy is the procedure of choice.
References
- 1.Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol 1941;31:731-65. [Google Scholar]
- 2.Granowitz SP, D’Antonio J, Mankin HL. The pathogenesis and long-term end results of pigmented villonodular synovitis. Clin Orthop Relat Res 1976;114:335-51. [Google Scholar]
- 3.Pandey S, Pandey AK. Pigmented villonodular synovitis with bone involvement. Arch Orthop Trauma Surg (1978) 1981;98:217-23. [Google Scholar]
- 4.Rochwerger A, Groulier P, Curvale G, Launay F. Pigmented villonodular synovitis of the foot and ankle: A report of eight cases. Foot Ankle Int 1999;20:587-90. [Google Scholar]
- 5.Blanco CE, Leon HO, Guthrie TB. Combined partial arthroscopic synovectomy and radiation therapy for diffuse pigmented villonodular synovitis of the knee. Arthroscopy 2001;17:527-31. [Google Scholar]
- 6.Goldman AB, DiCarlo EF. Pigmented villonodular synovitis. Diagnosis and differential diagnosis. Radiol Clin North Am 1988;26:1327-47. [Google Scholar]
- 7.Konrath GA, Shifrin LZ, Nahigian K. Magnetic resonance imaging in the diagnosis of localized pigmented villonodular synovitis of the ankle: A case report. Foot Ankle Int 1994;15:84-7. [Google Scholar]
- 8.Bisbinas I, De Silva U, Grimer RJ. Pigmented villonodular synovitis of the foot and ankle: A 12 year experience from a tertiary orthopedic oncology unit. J Foot Ankle Surg 2004;43:407-11. [Google Scholar]
- 9.Mendenhall WM, Mendenhall CM, Reith JD, Scarborough MT, Gibbs CP, Mendenhall NP. Pigmented villonodular synovitis. Am J Clin Oncol 2006;29:548-50. [Google Scholar]
- 10.Mori H, Nabeshima Y, Mitani M, Ozaki A, Fujii H, Kuroda R. Diffuse pigmented villonodular synovitis of the ankle with severe bony destruction: Treatment of a case by surgical excision with limited arthrodesis. Am J Orthop (Belle Mead NJ) 2009;38:E187-9. [Google Scholar]
- 11.Lee M, Mahroof S, Pringle J, Short SC, Briggs TW, Cannon SR. Diffuse pigmented villonodular synovitis of the foot and ankle treated with surgery and radiotherapy. Int Orthop 2005;29:403-06Figure Legends [Google Scholar]









