Patients undergoing surgery with Overlap Syndrome of Myasthenia Gravis and Motor Neuron Disease require expert medical care by a multidisciplinary approach.
Dr. Vidarshna Viburajah, Department of Anesthesia, Sri Ramachandra Institute of Higher Education and Research, Porur, Chennai, Tamil Nadu, India. E-mail: drvidarshna@gmail.com
Introduction: Amyotrophic lateral sclerosis (ALS) is a neurodegenerative condition producing symptoms of varying severity depending on the extent and progression of the disease pathology most importantly respiratory insufficiency and pulmonary complications. Myasthenia gravis (MG) on the other hand is an autoimmune condition due to the pathology involving failure of neuromuscular transmission causing muscle weakness exacerbated by activity and involvement of the respiratory muscles leading to respiratory failure. Overlap syndrome is a condition wherein both motor neuron disease (MND) and MG are present in the same patient. The safety of using muscle-relaxing agents in patients with MG undergoing major surgical procedures has so far been assessed as insufficient. There have been many concerns regarding anesthetic management in relation to complications with respiratory function in patients with ALS, with regional anesthesia being considered slightly safer.
Case Report: An 81-year-old female presented with a closed injury to her left hip, and she was diagnosed to have a left neck of femur fracture. She was also a known case of bulbar MND with an overlap syndrome of MG. She was hypertensive and controlled with regular medication. She was planned for a left hip bipolar arthroplasty. Anesthetic requirements and management of these patients require a high degree of expertise and anesthesia in patients undergoing surgery is prone to more complications and mortality. In addition, as the patient had an overlap of both MG and MND, more meticulous assessment and management strategies were necessary.
Conclusion: The importance and purpose of this study are to highlight a case of overlap syndrome of MND and MG patients who sustained a left neck femur fracture and underwent bipolar arthroplasty highlighting the anesthetic considerations in the patient for the procedure. We concluded that the choice of mode of anesthesia needs to be individualized based on each patient’s requirements after careful analysis of the risk-benefit ratio of general versus regional. Regional anesthesia was successfully administered for this patient.
Keywords: Motor neuron disease, myasthenia gravis, fracture, arthroplasty, surgery, anesthesia.
Motor neuron disease (MND) is a neurodegenerative condition caused by the loss of upper and lower motor neurons in the spinal cord, cranial nerve nuclei, and motor cortex. The most common form of MND is amyotrophic lateral sclerosis (ALS). The MND is relentlessly progressive and up to 50% end up in death within 2 years of diagnosis [1]. Respiratory insufficiency from muscle weakness and pulmonary complications is the prime cause of mortality in these patients. Myasthenia gravis (MG) is an autoimmune syndrome caused by the failure of neuromuscular transmission, which results from the binding of autoantibodies to proteins involved in signaling at the neuromuscular junction (NMJ). These proteins include the nicotinic acetylcholine receptor (AChR) or muscle-specific tyrosine kinase (MuSK) involved in AChR clustering [2]. The presence of these conditions in patients undergoing lower extremity surgery needs additional care and expertise in anesthetic management due to the lack of a universal consensus and a protocol. However, some literature and significant research work in the field relevant to the management of these conditions are available. ALS is a progressive neurodegenerative disease that mainly affects motor neurons responsible for controlling voluntary muscle movement [3]. It is caused by the loss of upper and lower motor neurons in the spinal cord, cranial nerve nuclei, and motor cortex [1]. Bulbar MND is one among the various types of ALS [1]. ALS is characterized by a combination of upper and lower motor neuron signs. The symptoms include limb muscle weakness, cramps, occasionally fasciculation and disturbance of speech/swallowing (dysarthria/dysphagia). Symptoms often begin focally in one part and spread gradually but relentlessly to become widespread. Signs include wasting and fasciculation of muscle, pyramidal tract involvement, causing spasticity, exaggerated deep tendon reflexes, and extensor plantar responses [1]. Respiratory-onset ALS is devastating and patients may develop dyspnea on exertion, orthopnea, hypoventilation, and pneumonia; therefore, patients require assisted breathing support devices such as non-invasive positive pressure ventilation, diaphragmatic pacing, or tracheotomy [4]. ALS patients pose challenges in perioperative anesthesia and care in view of post-operative respiratory complications, electrolyte imbalances, and worsening of neurologic status and functional decline after surgery [5]. MG is an autoimmune neuromuscular disease characterized by weakness and fatigability of skeletal muscles [6]. There is a failure of neuromuscular transmission. This is caused by the binding of autoantibodies to proteins involved in signaling at the NMJ [2]. There are usually no sensory signs or signs of involvement of the central nervous system [1]. There is variable muscle weakness which is exacerbated by exercise and repeated activity, with recovery after rest [6]. Respiratory muscles may get involved and respiratory failure is an avoidable cause of death, sometimes requiring ventilatory support if the weakness is severe or abrupt in onset [1]. Surgery and anesthesia in myasthenic gravis patients are associated with an increased risk of death and severe complications. The safety of using muscle-relaxing agents in patients with MG undergoing major surgical procedures has so far been assessed as insufficient. In general, inhalation anesthesia has the effect of inhibiting neuromuscular transmission, and the inhibitory effects were reported to be more prominent in patients with MG [7]. The issues thus elaborated above pose challenges to the anesthetic management of a patient who presented to us with MND and overlap with myasthenia, sustaining a neck of femur fracture of the left side requiring bipolar hemiarthroplasty surgery. At present, there is no consensus on the perioperative management neither for ALS patients nor patients with overlap syndrome undergoing lower extremity orthopedic surgery due to a lack of data because of the rarity and short life expectancy of the disease [5]. The two disorders, MG and ALS, are characteristic in their own aspect wherein MG is an autoimmune disorder of the NMJ causing fluctuating muscle weakness and fatigability, whereas ALS is a progressive neurodegenerative disorder affecting motor neurons of the brain and the spinal cord. While both of these diseases are rare incidences, our patient had a combination of both upper motor and lower motor symptoms signifying an overlap of both hence termed overlap syndrome.
An 81-year-old female presented to the Emergency Department with left hip closed injury following an alleged history of fall at her residence after which she was unable to bear weight over her injured hip. The patient had not sustained any other musculoskeletal injury or head injury at the time of the fall. After the initial clinical and radiological evaluation, she was diagnosed with left neck of femur fracture (Fig. 1 and 2).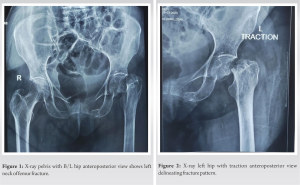 A computed tomography with 3D reconstruction of the pelvis was done to delineate the fracture pattern (Fig. 3). Her past medical history was significant for being a diagnosed case of bulbar MND with a possible overlap syndrome of MND and MG 2 years ago and has since been on treatment for the same. The patient is known to be hypertensive for the past 20 years on regular medications. The following details the sequence of events: 2 years back, the patient had complaints of drooling saliva, history of slurring of speech and progressive dysarthria, drooping of eyelids, breathlessness and unsteadiness while walking and progressive difficulty in swallowing, and liquids more than solid food. A neurologist was consulted for further evaluation. Physical examination revealed small muscle wasting (left more than right), and deep tendon reflexes were well elicited. A mild degree of fibrillations was noted over the tongue, with no significant atrophy.
A computed tomography with 3D reconstruction of the pelvis was done to delineate the fracture pattern (Fig. 3). Her past medical history was significant for being a diagnosed case of bulbar MND with a possible overlap syndrome of MND and MG 2 years ago and has since been on treatment for the same. The patient is known to be hypertensive for the past 20 years on regular medications. The following details the sequence of events: 2 years back, the patient had complaints of drooling saliva, history of slurring of speech and progressive dysarthria, drooping of eyelids, breathlessness and unsteadiness while walking and progressive difficulty in swallowing, and liquids more than solid food. A neurologist was consulted for further evaluation. Physical examination revealed small muscle wasting (left more than right), and deep tendon reflexes were well elicited. A mild degree of fibrillations was noted over the tongue, with no significant atrophy. 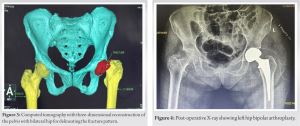 Fatigability was noted with drooping of eyelids on sustained elevation. There were brisk reflexes and mild impairment of left palatal movements with increased tone of lower limbs (left more than right) on examination and the patient was mobilizing with the help of walker support. Magnetic resonance imaging of the brain with contrast revealed an ectatic left vertebral artery indenting upon and compressing the left anterolateral aspect of the medulla. Constructive interference in steady state-three-dimensional protocol images showed that the medullary by vertebral artery is minimal only. Nerve conduction velocity suggested of axonal type of sensory-motor neuropathy involving bilateral lower limb nerves – reduced compound muscle action potential(CMAP) amplitude from bilateral peroneal nerves (extensor digitorum brevis pickup) with Achilles tendon pick up normal. Lower limb sensory conduction showed absent sensory nerve action potentials(SNAP) amplitude from bilateral superficial peroneal nerves. Responsive neurostimulation was normal. Needle electromyography revealed a neurogenic pattern from bulbar and cervical segments – fasciculations from right flexor digitorum indices (1+), biceps (1+), and tongue muscles. AChR antibodies and MuSK antibodies were negative. The Karnofsky Performance Index was assessed and the patient was evaluated to be able to carry on normal activity and to work; no special care was required. The Karnofsky Performance Index is an assessment tool that helps clinicians to assess the level of functional impairment of the patient and the ability of the patient to carry out day–day activities. It may indirectly signify the prognosis and the likelihood of survival.
Fatigability was noted with drooping of eyelids on sustained elevation. There were brisk reflexes and mild impairment of left palatal movements with increased tone of lower limbs (left more than right) on examination and the patient was mobilizing with the help of walker support. Magnetic resonance imaging of the brain with contrast revealed an ectatic left vertebral artery indenting upon and compressing the left anterolateral aspect of the medulla. Constructive interference in steady state-three-dimensional protocol images showed that the medullary by vertebral artery is minimal only. Nerve conduction velocity suggested of axonal type of sensory-motor neuropathy involving bilateral lower limb nerves – reduced compound muscle action potential(CMAP) amplitude from bilateral peroneal nerves (extensor digitorum brevis pickup) with Achilles tendon pick up normal. Lower limb sensory conduction showed absent sensory nerve action potentials(SNAP) amplitude from bilateral superficial peroneal nerves. Responsive neurostimulation was normal. Needle electromyography revealed a neurogenic pattern from bulbar and cervical segments – fasciculations from right flexor digitorum indices (1+), biceps (1+), and tongue muscles. AChR antibodies and MuSK antibodies were negative. The Karnofsky Performance Index was assessed and the patient was evaluated to be able to carry on normal activity and to work; no special care was required. The Karnofsky Performance Index is an assessment tool that helps clinicians to assess the level of functional impairment of the patient and the ability of the patient to carry out day–day activities. It may indirectly signify the prognosis and the likelihood of survival.
Pre-operative period
The patient on admission underwent the regular pre-operative workup with a routine evaluation of the blood parameters and serology. The patient was assessed with hyponatremia and corrective measures were instituted pre-operatively with advice from the general physician. The patient required oxygen support using nasal prongs in view of desaturation at room air. Pre-operative neurological assessment by neurologists was done for surgical risk assessment and anesthesia requirements in view MND and overlap with myasthenia. On the day of surgery, the patient had appropriately fasted for 8 h, and the patient’s vitals 15 min before anesthesia induction were heart rate of 82/min, blood pressure of 150/80 mmHg, and respiratory rate of 20/min with 96% SpO2 with 3L oxygen support with nasal prongs. After a multidisciplinary approach involving the surgical and anesthesia team, the patient elected to have spinal anesthesia in view of potential complications including post-operative respiratory failure associated with MND.
Intra-operative period
In the operating theater, a 20-gauge intravenous (IV) was secured and the standard anesthetic monitoring was applied with 5-lead electrocardiogram, pulse oximeter, blood pressure monitoring, temperature, and capnography. The patient was administered spinal anesthesia in a sitting midline approach with a 27-gauge Pencan spinal needle in L3-L4 space. 2 ml of 0.5% bupivacaine was given which attained a sensory level of T10 and a complete motor blockade of both lower limbs (modified Bromage scale of IV). Appropriate antibiotics were administered before surgical incision according to the institutional protocol. The surgeon proceeded with left hip bipolar arthroplasty, by direct lateral Hardinge approach. Surgery was uneventful with a total procedure time of 1 h, from the time of incision to completion of surgery. The patient remained hemodynamically stable (heart rate 80–85, respiratory rate 18–22 with 100% SpO2 saturation, skin temperature of 36.3, and blood pressure mean 75–104) during the intraoperative period. While spinal anesthesia is usually preferred in hip surgeries, it is relatively contraindicated in patients having MND. However, since our patient also had MG overlapped on ALS, administration of general anesthesia using a muscle relaxant was more dangerous due to the associated respiratory complications. Hence, after careful consideration of all the associated risks, subarachnoid block was chosen after proper documentation of lower limb weakness before administration.
Post-operative period
In the post-anesthesia care unit, the patient had minimal pain at the surgical site and no nausea or vomiting. Patient vitals were observed to be stable in the post-operative period and the patient was shifted out from the post-anesthesia care unit to the ward for further care. Post-operatively, the patient was able to slowly ambulate using walker support and was provided further rehabilitation and regular wound care. Post-operative X-rays were taken for assessment (Fig. 4). The patient was discharged on the 5th post-operative day after reassessment and evaluation by a neurologist for advice regarding management and continuation of medication on discharge. No neurological complications were noted during this hospitalization. The patient was subsequently followed up to assess the recovery and rehabilitation following the surgery. The patient continued to receive treatment from the neurologist for the pre-existing conditions of MND and MG. Three months following the surgery, the patient was recovering very well and was ambulant independently with the aid of a walker support.
The major concerns faced during the management of this patient were the need to consider anesthetic requirements and complications in view of simultaneously tackling the issues of MND and MG. One of the major issues for most patients with ALS is respiratory insufficiency. There have been many discussions and concerns regarding the usage and ideal anesthetic management in relation to complications with respiratory function. There is a relative contraindication to using regional central neuraxial block in patients with ALS for fear of exacerbating the progression of disease pattern [8]. General anesthesia may cause aspiration and/or fatal respiratory depression ALS patients [9]. Depolarizing muscle relaxants elicit neuromyotonia-like contractions, rhabdomyolysis, and severe hyperkalemia [8]. Non-depolarizing muscle relaxants can be administered but sensitivity to these drugs is altered as in upper and lower motor neuron lesions, immobilization, and burns [8]. The Borg dyspnea scale, a non-invasive test, has been used as a simple marker to predict respiratory muscle weakness in ALS [8]. However, regional anesthesia can be considered a safer option than general anesthesia, in regard to effects on the respiratory system for surgeries of the abdomen or lower extremity, especially when the patient’s pulmonary function is already compromised. The usage of muscle relaxants in patients with MG is a major concern. Severe complications including mortality are more common during surgery and anesthesia in patients suffering from myasthenic gravis. The risk is primarily due to more sensitivity to muscle relaxants observed in these patients, even in periods of complete remission [6]. Reports suggest that patients with MG are sensitive to non-depolarizing neuromuscular blocking agents [7]. These patients show relative resistance to succinylcholine [10]. In general, inhalation anesthesia has the effect of inhibiting neuromuscular transmission, and the inhibitory effects were reported to be more prominent in patients with MG [7]. The most proper approach during anesthesia in patients with MG is to apply deep inhalational anesthesia without muscle relaxing agents [6]. In the pre-operative period, simple evaluating measures such as train of four tests can be used to estimate the required amount of non-depolarizing muscle relaxants in MG [10]. These patients require close monitoring in the post-operative period and may require to be in ICU for recovery and ventilation [6]. Taking into consideration, all the factors and possible associated complications with regard to both spinal and general anesthesia, finally spinal anesthesia was opted for with close monitoring of the vitals intraoperatively and in the post-operative period. Post-operatively, there were no complications in the post-operative anesthesia care unit and during the in-hospital stay with respect to the anesthesia and recovery.
The need and requirements of anesthesia in patients with MND are to be individualized depending upon the other comorbidities of the patient, the type of surgery with an assessment of the risk–benefit ratio, choosing an anesthetic agent and ideal technique which does not exacerbate the pre-existing disease condition while providing adequate analgesia and immobility during the procedure.
Overlap syndrome of MND and MG is a rare presentation. Thorough clinical evaluation for diagnosis and choosing an anesthetic agent with ideal technique along with good surgical expertise can be rewarding.
References
- 1.Walker BR, Colledge NR, Ralston S, Penman ID, Britton R. Neurological Disease. In: Davidson’s Principles and Practice of Medicine. 22nd ed., Ch. 26. Edinburgh: Churchill Livingstone/Elsevier; 2014. [Google Scholar]
- 2.Conti-Fine BM, Milani M, Kaminski HJ. Myasthenia gravis: Past, present, and future. J Clin Invest 2006;116:2843-54. [Google Scholar]
- 3.Onders RP, Carlin AM, Elmo M, Sivashankaran S, Katirji B, Schilz R. Amyotrophic lateral sclerosis: The Midwestern surgical experience with the diaphragm pacing stimulation system shows that general anesthesia can be safely performed. Am J Surg 2009;197:386-90. [Google Scholar]
- 4.Zarei S, Carr K, Reiley L, Diaz K, Guerra O, Altamirano PF, et al. A comprehensive review of amyotrophic lateral sclerosis. Surg Neurol Int 2015;6:171. [Google Scholar]
- 5.Panchamia JK, Gurrieri C, Amundson AW. Spinal anesthesia for amyotrophic lateral sclerosis patient undergoing lower extremity orthopedic surgery: An overview of the anesthetic considerations. Int Med Case Rep J 2020;13:249-54. [Google Scholar]
- 6.Kamath SS, Misquith JC. General anesthesia using supraglottic airway device in a myasthenic patient undergoing reverse shoulder arthroplasty. Anesth Essays Res 2018;12:598-600. [Google Scholar]
- 7.Uchida S, Kudo R, Takekawa D, Hirota K. Anesthetic management of a patient with subclinical myasthenia gravis who underwent a thymectomy: A case report. JA Clin Rep 2022;8:49. [Google Scholar]
- 8.Thampi SM, David D, Chandy TT, Nandhakumar A. Anesthetic management of a patient with amyotrophic lateral sclerosis for transurethral resection of bladder tumor. Indian J Anaesth 2013;57:197-9. [Google Scholar]
- 9.Park KB, Son B, Hwang DY, Jeon Y. Spinal anesthetic management for discectomy in a patient with amyotrophic lateral sclerosis-a case report-. Korean J Anesthesiol 2012;63:547-9. [Google Scholar]
- 10.Schmitt HJ, Muenster T. Anesthesia in patients with neuromuscular disorders. Minerva Anestesiol 2009;75:632-7. [Google Scholar]








