Open intra-articular fractures require immediate internal fixation and restoration of joint congruity due to potential risk for chondrocyte damage when exposed to blood for prolonged period. The heightened risk for infection due to early internal fixation can be mitigated by thorough debridement and the use of antibiotic loaded calcium sulfate beads.
Dr. N Nizaj, Department of Orthopaedics, Apollo Adlux Hospital, Kochi, Kerala 683576, India. E-mail: drnizaj239@gmail.com
Introduction: Open fractures with massive bone defect presents as challenging clinical scenario in clinical practice. If neglected, this can result in infection, non-union or severe limb length discrepancy. Autogenous vascularized fibula grafting along with stable fixation in the form of internal fixation is a viable option in such situations. Synthetic calcium sulfate is a suitable antibiotic carrier to deliver antibiotics locally to prevent infection. We report the case of an adult male who had an open fracture of the distal femur with segmental bone loss of 21 cm, managed with autogenous vascularized fibula graft and locking plates. We used antibiotic-loaded absorbable synthetic calcium sulfate beads locally during the procedure.
Case Report: A 52-year-old male, a known case of uncontrolled diabetes mellitus, presented to the emergency department with a comminuted open intra-articular fracture of the left distal femur with bone loss of 21 cm (arbeitsgemeinschaft fur osteosynthesefragen 33C3) following a road traffic accident. He was initially treated with meticulous debridement and internal fixation with locking compression plate. Considering the massive bone defect of 21 cm, he was planned for fibula grafting at a later stage. After 6 weeks, he underwent vascularized fibula grafting from opposite leg and an additional medial plate to stabilize the graft and augment the initial fixation. He was on regular follow-up in the outpatient department. The fracture united with no signs of infection or residual limb length discrepancy. At the latest follow-up at 7 months, he is walking independently without support and is having a functional range of knee movements. There were no post-operative complications in the right leg from where fibula was harvested.
Conclusion: Autogenous vascularized fibula graft together with a locking compression plate is a practical choice in managing open fractures with segmental bone loss. The high concentration of local antibiotic delivery with the help of synthetic calcium sulfate beads helped prevent infection, which is the most dreaded complication associated with open fractures. In addition, the calcium sulfate beads promote endochondral ossification resulting in early bone union.
Keywords: Distal femur fracture, vascularized fibula graft, bone loss, synthetic calcium sulfate beads, open fracture.
Distal femur fractures account for 7% of all femur fractures [1]. The high velocity impact can cause significant morbidity to the affected limb. The most common mechanism is an indirect trauma on a bend knee and rarely can due to direct trauma by crush injury. Open fractures with massive bone defect present as challenging clinical scenario in clinical practice. If neglected, this can result in osteomyelitis, non-union or severe limb length discrepancy. Autogenous fibula grafting along with stable fixation in the form of internal fixation devices maintains the limb length, stabilizes the fractures, and fastens the union [2]. Open fractures result in severe soft-tissue damage that disrupts the vascular architecture, which lowers the local tissue concentration of intravenously delivered antibiotics. A good antibiotic carrier to deliver antibiotics locally can resolve this. Synthetic calcium sulfate is such a suitable antibiotic carrier, which has specific advantage that is mentioned in this report. We report the case of an adult male who had open fracture of distal femur with segmental bone loss of 21 cm, managed with autogenous vascularized fibula graft and locking plates. We used antibiotic loaded absorbable synthetic calcium sulfate beads locally during the procedure.
A 52-year-old male, a known case of poorly controlled diabetes mellitus (HbA1C – 8.2%) and hypertension, presented to the emergency department with pain and deformity over his left thigh following a road traffic accident. On arrival, his Glasgow coma scale was full, blood pressure: 90/60 mm of Hg, and pulse rate: 122 beats/min. On examination, a 5 × 3 cm lacerated wound was found over distal thigh with bone exposed (Fig. 1).  There was local tenderness with abnormal mobility at distal thigh. There were no other injuries pertaining to chest, abdomen, pelvis or spine, which was confirmed with computerized tomography (CT) scans. Radiographs revealed comminuted displaced fracture left distal femur with intra-articular extension and bone loss (Fig. 2). The fracture can be classified as open type IIIA Gustilo-Anderson and arbeitsgemeinschaft fur osteosynthesefragen 33C3. His injury severity score was 9. The patient was resuscitated and intravenous antibiotics were started. A CT with 3D reconstruction of knee was taken which showed multifragmentary articular fragments (Fig. 3). He was taken up for immediate wound debridement and internal fixation of the fracture. Surgery was performed under spinal anesthesia in supine position. Wound over distal thigh debrided. There was no skin loss. Skin edges freshened and necrotic soft tissues excised. Loose bone fragments were thoroughly washed with normal saline and betadine and kept aside, to be inserted at the end of fixation to act as a graft. Distal femur fracture was approached through lateral approach. There was around 21 cm bone loss at the metaphyseodiaphyseal area. Anatomical fixation was done for the articular fragments and fixed using a distal femur LCP (Fig. 4). Vancomycin impregnated absorbable calcium sulfate beads were used at the fracture site. Wound was closed and intravenous antibiotics were continued. The post-operative period was uneventful. He got discharged after 5 days with oral antibiotics. Our plan was to do vascularized fibula grafting and a medial plate stabilization after 6 weeks. We faced many challenges during the management, type IIIA open fracture with massive bone defect, comminution of the articular fragments, and uncontrolled diabetes. He had weekly follow-up in the outpatient department. The patient was advised with isometric exercise and non-weight-bearing mobilization. As a pre-operative planning, we performed a CT angiography of his lower limb to assess the vascularity and blood supply pattern of the fibula, and to rule out peripheral occlusive vascular diseases (POVD) and malformations. Angiography was normal. Under general anesthesia, harvesting of free vascularized fibula was performed by plastic surgery team from the opposite leg. Skin incision made posterolaterally, and further, dissection was done between peroneus longus and soleus muscle. Fibula osteotomized proximally and distally leaving at least 8 cm of bone from either ends. The recipient area at anterior thigh prepared. The harvested 23 cm of fibula along with the peroneal vessel pedicle transferred (Fig. 5).
There was local tenderness with abnormal mobility at distal thigh. There were no other injuries pertaining to chest, abdomen, pelvis or spine, which was confirmed with computerized tomography (CT) scans. Radiographs revealed comminuted displaced fracture left distal femur with intra-articular extension and bone loss (Fig. 2). The fracture can be classified as open type IIIA Gustilo-Anderson and arbeitsgemeinschaft fur osteosynthesefragen 33C3. His injury severity score was 9. The patient was resuscitated and intravenous antibiotics were started. A CT with 3D reconstruction of knee was taken which showed multifragmentary articular fragments (Fig. 3). He was taken up for immediate wound debridement and internal fixation of the fracture. Surgery was performed under spinal anesthesia in supine position. Wound over distal thigh debrided. There was no skin loss. Skin edges freshened and necrotic soft tissues excised. Loose bone fragments were thoroughly washed with normal saline and betadine and kept aside, to be inserted at the end of fixation to act as a graft. Distal femur fracture was approached through lateral approach. There was around 21 cm bone loss at the metaphyseodiaphyseal area. Anatomical fixation was done for the articular fragments and fixed using a distal femur LCP (Fig. 4). Vancomycin impregnated absorbable calcium sulfate beads were used at the fracture site. Wound was closed and intravenous antibiotics were continued. The post-operative period was uneventful. He got discharged after 5 days with oral antibiotics. Our plan was to do vascularized fibula grafting and a medial plate stabilization after 6 weeks. We faced many challenges during the management, type IIIA open fracture with massive bone defect, comminution of the articular fragments, and uncontrolled diabetes. He had weekly follow-up in the outpatient department. The patient was advised with isometric exercise and non-weight-bearing mobilization. As a pre-operative planning, we performed a CT angiography of his lower limb to assess the vascularity and blood supply pattern of the fibula, and to rule out peripheral occlusive vascular diseases (POVD) and malformations. Angiography was normal. Under general anesthesia, harvesting of free vascularized fibula was performed by plastic surgery team from the opposite leg. Skin incision made posterolaterally, and further, dissection was done between peroneus longus and soleus muscle. Fibula osteotomized proximally and distally leaving at least 8 cm of bone from either ends. The recipient area at anterior thigh prepared. The harvested 23 cm of fibula along with the peroneal vessel pedicle transferred (Fig. 5). The fibula shaft was introduced into the defect and inserted into the medullary canal of femur proximally and distally. A distal femur LCP was used on the medial side to stabilize the fibula graft and to augment the initial distal femoral fixation. Microvascular anastomosis was performed with the descending branch of lateral circumflex femoral artery (Fig. 6).
The fibula shaft was introduced into the defect and inserted into the medullary canal of femur proximally and distally. A distal femur LCP was used on the medial side to stabilize the fibula graft and to augment the initial distal femoral fixation. Microvascular anastomosis was performed with the descending branch of lateral circumflex femoral artery (Fig. 6).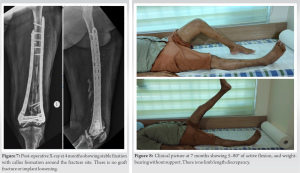 Vancomycin-loaded absorbable calcium sulfate beads were used at bone defect. Wounds over thigh and leg closed primarily. Postoperatively, the flap vascularity were monitored serially with Doppler scan and showed satisfactory flow. The patient was discharged after 7 days with oral antibiotics. He had regular follow-ups in outpatient departments. Radiographic union with callus formation was found at 4 months (Fig. 7). At 4 months, partial weight-bearing was initiated, and at 5 months, he started walking independently without support. At the latest follow-up at 7 months, he has good functional range of movements of his affected knee; active flexion of 5°–80° (Figs. 8 and 9). There were no signs of infection or limb length discrepancy. There were no post-operative complications in the right leg from where fibula was harvested (Fig. 10).
Vancomycin-loaded absorbable calcium sulfate beads were used at bone defect. Wounds over thigh and leg closed primarily. Postoperatively, the flap vascularity were monitored serially with Doppler scan and showed satisfactory flow. The patient was discharged after 7 days with oral antibiotics. He had regular follow-ups in outpatient departments. Radiographic union with callus formation was found at 4 months (Fig. 7). At 4 months, partial weight-bearing was initiated, and at 5 months, he started walking independently without support. At the latest follow-up at 7 months, he has good functional range of movements of his affected knee; active flexion of 5°–80° (Figs. 8 and 9). There were no signs of infection or limb length discrepancy. There were no post-operative complications in the right leg from where fibula was harvested (Fig. 10).
The incidence of fracture-related infections is as high as 30% in open fractures, hence having a very significant socioeconomic impact on the patient [3]. Bone defects in open fracture should be addressed early to avoid non-union and significant limb length discrepancy. The severe soft-tissue damage, periosteal stripping, and contamination associated with open fractures pose a great threat to their management. The altered vascular anatomy at the fracture site makes treatment more difficult because it makes it harder for host immune cells to reach the fracture site and makes it impossible to deliver sufficient antibiotics when given systemically [4]. The surgeon should be very careful when attempting a primary fixation in such fractures because the bacteria adheres to the implant surface and forms a biofilm over it. In the biofilm, the bacteria proliferate and protect themselves from antibiotics and the human immune system [5, 6]. The defects more than 6 cm most often fail with conventional bone grafting. Management of such bone defects needs specialized techniques such as Masquelet technique, Ilizarov distraction osteogenesis, or vascularized fibula grafting. However, filling massive bone defects with masquelet requires huge amount of cancellous bone grafts that may cause significant donor site morbidity and has a prolonged recovery period. With Ilizarov fixation, the patient can be mobilized early. However, it may take a long time to fill such a huge defect and can have pin tract infection, adjacent joint stiffness, and soft-tissue tethering [7]. Only a few studies discuss the significance of early fracture fixation, hemostasis, and dead space control in managing open intra-articular fractures. The chondrocyte apoptosis occurs when the cartilage is exposed to 10% (v/v) blood for more than 2 days. This may result in irreversible damage, eventually causes joint destruction [8, 9]. Furthermore, with a delayed closure of the wound, the cartilage desiccates and necroses. Hence, the aim of the treatment should be early anatomical fixation to restore the articular congruity and early wound closure. The selection of the graft for reconstruction depends on multiple factors, including the extent of bone loss, the need for augmented blood supply to the donor bone segment, the integrity of the bone, and the consideration of a separate incision. Given these considerations, the optimal choice for the bone graft in our case was found to be the fibula. The fibula graft provides good biomechanical stability for the massive defects when used in conjunction with internal fixation devices. Allografts are the other option for grafting. However, the risk of transmission of infection, limited availability, and risk of immunogenicity make them secondary to autografts [10, 11]. The pre-operative angiography played a critical role in assessing the vascularity and blood supply pattern of the fibula and hence, determining the feasibility of utilizing a vascularized bone graft. It also helped identify potential issues such as POVD, congenital hypoplasia, or malformations of the fibular vessel that could compromise vascularity and result in a poor outcome. Although an uncontrolled diabetic, our patient was not suffering from coexistent peripheral occlusive disease that could render poor outcomes to the procedure [12, 13]. Vascularized bone grafts offer several advantages over non-vascularized grafts. One significant benefit is their ability to remodel bone, promoting better incorporation, and aiding in normal biological healing. This remodeling capacity enhances the graft’s long-term stability and durability, facilitating functional recovery. In our case, the use of a vascularized bone graft allowed for improved bone remodeling and integration, contributing to a successful outcome with a single barreled fibular graft. However, the use of vascularized grafting is surgically demanding and requires microsurgical techniques [14]. Despite the successful surgical intervention, several complications could arise during the postoperative period and has to be anticipated. Anastomotic blood leaks, thrombosed anastomotic vessels, inadequate graft hypertrophy, and graft fractures are some examples. Meticulous microvascular anastomosis and vigilant postoperative monitoring with ultrasonography were performed, to detect any signs of compromised vascularity [15]. Antibiotic-loaded calcium sulfate beads are found superior to PMMA beads, as the latter are non-biodegradable and require a second surgery for their removal. PMMA beads release a sub-inhibitory concentration of antibiotics, and hence, the bacteria acquire resistance against those drugs. Moreover, the PMMA has a very short period of drug release and is not amenable to thermosensitive antibiotics [16]. However, the calcium sulfate beads degrade completely and elude the whole of their antibiotic load, causing very high local concentrations with less systemic toxicity [17]. Calcium sulfate also stimulates growth factors such as vascular endothelial cell growth factor, transforming growth factor-1, and bone morphogenetic protein-2 and also promotes endochondral ossification at the broken bone ends [18]. The use of these absorbable antibiotic delivery systems decreases the need for prolonged intravenous antibiotics, a long hospital stay, and multiple surgeries.
Autogenous vascularized fibula graft together with locking compression plate is a practical choice in managing open fractures with segmental bone loss. The high concentration of local antibiotic delivery with the help of synthetic calcium sulfate beads helped prevent infection, which is the most dreaded complication associated with open fractures. In addition, the calcium sulfate beads promote endochondral ossification resulting in early bone union.
Meticulous debridement, early fracture fixation, vascularized bone grafting, and the local use of antibiotic-loaded calcium sulfate beads are the most effective steps for managing open intra-articular distal femur fractures with bone loss. Our technique can serve as a useful option for the prevention of infection, non-union, and limb length discrepancy in massive bone defects. This has also reduced the need for a prolonged hospital stay and, hence, lessened the financial burden on the patient.
References
- 1.Arneson TJ, Melton LJ 3rd, Lewallen DG, O’Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965-1984. Clin Orthop Relat Res 1988;234:188-94. [Google Scholar]
- 2.Kumar S, Sachdev T, Ratanpal A, Thakur A, Singh BP, Ekka AK. Bone defects following trauma, managed by non-vascularized fibular strut graft: A single centre study. Int J Innov Res Med Sci 2022;7:628-33. [Google Scholar]
- 3.Dugan TR, Hubert MG, Siska PA, Pape HC, Tarkin IS. Open supracondylar femur fractures with bone loss in the polytraumatized patient-timing is everything! Injury 2013;44:1826-31. [Google Scholar]
- 4.Ito K, Perren SM. Biology and biomechanics in bone healing. In: Rüedi TP, Buckley RE, Moran CG, editors. AO Principles of Fracture Management. Davos Platz: AO Publishing; 2007. p. 9e31. [Google Scholar]
- 5.Metsemakers WJ, Kuehl R, Moriarty TF, Richards RG, Verhofstad MH, Borens O, et al. Infection after fracture fixation: Current surgical and microbiological concepts. Injury 2018;49:511-22. [Google Scholar]
- 6.Busscher HJ, Van der Mei HC, Subbiahdoss G, Jutte PC, Van den Dungen JJ, Zaat SA, et al. Biomaterial-associated infection: Locating the finish line in the race for the surface. Sci Transl Med 2012;4(153). [Google Scholar]
- 7.Ma CH, Chiu YC, Wu CH, Tsai KL, Wen TK, Tu YK. Ipsilateral vascularised fibula with external locking plate for treatment of massive tibial bone defects. Injury 2021;52:1629-34. [Google Scholar]
- 8.Jansen NW, Roosendaal G, Bijlsma JW, Degroot J, Lafeber FP. Exposure of human cartilage tissue to low concentrations of blood for a short period of time leads to prolonged cartilage damage: An in vitro study. Arthritis Rheum 2007;56:199-207. [Google Scholar]
- 9.Hooiveld M, Roosendaal G, Wenting M, Van den Berg M, Bijlsma J, Lafeber F. Short-term exposure of cartilage to blood results in chondrocyte apoptosis. Am J Pathol 2003;162:943-51. [Google Scholar]
- 10.Lawal YZ, Garba ES, Ogirima MO, Dahiru IL, Maitama MI, Abubakar K, et al. Use of non-vascularized autologous fibula strut graft in the treatment of segmental bone loss. Ann Afr Med 2011;10:25-8. [Google Scholar]
- 11.Barbour SA, King W. The safe and effective use of allograft tissue--an update. Am J Sports Med 2003;31:791-7. [Google Scholar]
- 12.Al Deek NF, Kao HK, Wei FC. The fibula osteoseptocutaneous flap: Concise review, goal-oriented surgical technique, and tips and tricks. Plast Reconstr Surg 2018;142:913e-23. [Google Scholar]
- 13.Lee EH, Goh JC, Helm R, Pho RW. Donor site morbidity following resection of the fibula. J Bone Joint Surg Br 1990;72:129-31. [Google Scholar]
- 14.Bumbasirevic M, Stevanovic M, Bumbasirevic V, Lesic A, Atkinson HD. Free vascularised fibular grafts in orthopaedics. Int Orthop 2014;38:1277-82. [Google Scholar]
- 15.Pliefke J, Rademacher G, Zach A, Bauwens K, Ekkernkamp A, Eisenschenk A. Postoperative monitoring of free vascularized bone grafts in reconstruction of bone defects. Microsurgery 2009;29:401-7. [Google Scholar]
- 16.Aiken SS, Cooper JJ, Florance H, Robinson MT, Michell S. Local release of antibiotics for surgical site infection management using high-purity calcium sulfate: An in vitro elution study. Surg Infect (Larchmt) 2015;16:54-61. [Google Scholar]
- 17.Kallala R, Harris WE, Ibrahim M, Dipane M, McPherson E. Use of stimulan absorbable calcium sulphate beads in revision lower limb arthroplasty: Safety profile and complication rates. Bone Joint Res 2018;7:570-9. [Google Scholar]
- 18.Ma YF, Jiang N, Zhang X, Qin CH, Wang L, Hu YJ, et al. Calcium sulfate induced versus PMMA-induced membrane in a critical-sized femoral defect in a rat model. Sci Rep 2018;8:637. [Google Scholar]










