In case of traumatic articular destruction of the second MCP joint, replacing the lost articulation with a prosthesis could be a valid option.
Dr. Aleid C J Ruijs, Department of Orthopaedic Surgery, Centre Hospitalier de Wallonie Picarde, Avenue Delmée 9, 7500 Tournai, Belgium. E-mail: aleidruijs@hotmail.com
Introduction: Traumatic bone loss at the metacarpal phalangeal joint level can be a challenging clinical situation. Not many cases have been described in the literature for this specific articulation.
Case Report: Our patient presented with a work-related accident of his hand with loss of the metacarpophalangeal joint of the index finger. After temporary external fixation and wound closure, a prosthetic joint arthroplasty was chosen to allow a reconstruction of his lost joint.
Conclusion: After traumatic articular bone destruction in the hand, there are several possibilities to reflect on. Taking into consideration the patient’s characteristics and the degree of bone loss, implanting a prosthesis can be a safe option with acceptable results.
Keywords: Metacarpophalangeal joint, bone loss, prosthesis, MCPJ arthroplasty.
Metacarpophalangeal (MCP) joint arthroplasty is a promising and successful technique described for the treatment of post-traumatic metacarpophalangeal joint (MCPJ) arthritis and rheumatoid arthritis. However, this technique could also be considered a valuable treatment option in the setting of acute MCPJ trauma with bone loss. Therefore, we would like to present a case report which reinforces this hypothesis.
A 37-year-old male, worker in a production factory of billiard balls, presented a large dorsal-radial wound over the second MCPJ of the left hand. His skin was severely crushed, after a work-related trauma by a grindstone machine while the MCPJs were flexed. On admission, the X-ray showed bone loss at the dorsal part of P1 and the metacarpal head of the index finger (Fig. 1). There were also important lesions of the second and third extensor digitorum tendons as well as the extensor indicis tendon. There was no soft-tissue loss, and the neurovascular bundles of the index finger were intact. The first stage of treatment consisted of wound debridement and saline irrigation, suture of the extensor tendons of the index and the middle finger, and stabilization by a temporary external fixator to preserve the length and alignment (Fig. 2).
There were also important lesions of the second and third extensor digitorum tendons as well as the extensor indicis tendon. There was no soft-tissue loss, and the neurovascular bundles of the index finger were intact. The first stage of treatment consisted of wound debridement and saline irrigation, suture of the extensor tendons of the index and the middle finger, and stabilization by a temporary external fixator to preserve the length and alignment (Fig. 2).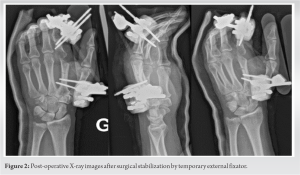 Two weeks later, we performed a second look to clean the wound and verified the integrity of collateral ligaments of the MCPJ. The favorable evolution of the wound allowed us to remove the external fixator and the patient started an active rehabilitation protocol with a physiotherapist. After the initial debridement and stabilization of this injury, we discussed the best therapeutic option for this patient. A decision was made to reconstruct the joint with a MCP prosthesis (TMPR™, MatOrtho Limited, Leatherhead, United Kingdom) using a dorsal approach (Fig. 3).
Two weeks later, we performed a second look to clean the wound and verified the integrity of collateral ligaments of the MCPJ. The favorable evolution of the wound allowed us to remove the external fixator and the patient started an active rehabilitation protocol with a physiotherapist. After the initial debridement and stabilization of this injury, we discussed the best therapeutic option for this patient. A decision was made to reconstruct the joint with a MCP prosthesis (TMPR™, MatOrtho Limited, Leatherhead, United Kingdom) using a dorsal approach (Fig. 3). This operation was performed 38 days following the initial trauma (5 weeks). The patient returned to his job within 6 months following the procedure with the same manual work on the same machine, suitable for his abilities. At this time of follow-up, he was experiencing little pain with a slight lack of grip. Despite loss of finger length, the extension was complete and the flexion of the MCPJ was 15°. The last follow-up was at 3 years postoperatively (Fig. 4) and the patient described occasional pain rated 4/10 on the Visual Analog Scale (EVA), and 5/10 during heavy activities.
This operation was performed 38 days following the initial trauma (5 weeks). The patient returned to his job within 6 months following the procedure with the same manual work on the same machine, suitable for his abilities. At this time of follow-up, he was experiencing little pain with a slight lack of grip. Despite loss of finger length, the extension was complete and the flexion of the MCPJ was 15°. The last follow-up was at 3 years postoperatively (Fig. 4) and the patient described occasional pain rated 4/10 on the Visual Analog Scale (EVA), and 5/10 during heavy activities. The QuickDASH score was 29 (40.91%), and the Patient-Rated Wrist Evaluation Score was 56/150. He scored 90% on the SF-36 physical functioning. X-rays validate the satisfactory stability and position of the implant.
The QuickDASH score was 29 (40.91%), and the Patient-Rated Wrist Evaluation Score was 56/150. He scored 90% on the SF-36 physical functioning. X-rays validate the satisfactory stability and position of the implant.
Traumatic bone loss at the MCP joint is a serious injury, leading in general to a loss of function. Multiple strategies and salvage procedures can be explored to achieve, in acute or delayed settings of trauma, the best functional outcome for the patient with minimal sequels. In most cases, the initial treatment is emergency stabilization by wires or a temporary external fixator. Pomares et al. [1] described an atypical case of a patient treated, in the first step of a two-stage protocol, by an articular spacer designed for MCP comminuted joint fractures, with the fragmentation of the 2nd metacarpal head, before considering a reconstruction of the MCPJ. For our patient, this short-term solution was limited by the large bone loss at the dorsal part of the first phalanx and proved to be difficult to get joint congruency. Regarding the other treatment options sustaining the early mobilization of the injured MCPJ, we find in the literature non-prosthetic arthroplasties such as soft-tissue interposition, especially the use of the volar plate described by Tupper [2], or costal cartilage grafting presented by Zappaterra et al. [3]. These interventions were not suggested in the emergency. The implant arthroplasty, popularized by Swanson’s silicone implants, was used as a well-founded technique in the reconstruction of post-traumatic arthritis and rheumatoid arthritis of MCP and PIP joints, to such an extent that these successful implants were used in primary intention with or without bone grafting in complex traumatic joint fractures with bone defect [4, 5, 6]. After long-term assessment, the literature raised concerns about the high risk of implant fractures, late failure, delayed infections, lack of stability, and loss of strength, leading to loss of function. These complications might be similar to new surface replacement arthroplasties developed recently. However, in the last decade, a few scientific articles have been published with poor follow-up concerning the treatment by MCPJ prosthetic arthroplasty in the acute setting of trauma. Pomares and Jager [7] described their experience in the management of MCPJ destruction with emergency silicone implant arthroplasty in association with grafting of the metacarpal bone in a patient victim of trauma by a circular saw. Results in ROM 8 months after surgery showed 50° of passive and active MCPJ flexion and complete extension. Houdek et al. [8] reported the outcome of 10 pyrocarbon MCPJ implants (6 hemiarthroplasties, 4 total joint replacements) performed within 24 h in seven patients for open MCPJ injuries resulting in soft tissue and bone defects. The mean total arc of motion for MCP was 56° (30°–70°). No authors listed mentioned instability after treatment. The idea of maintaining a rapid mobilization and preserving a good range of motion using implants for MCPJs in single-stage reconstruction seems to be an alternative treatment option, recommended in open trauma wounds with minimal contamination [8]. The other advantages of prosthetic joint replacement are avoiding fusion and authorizing further reconstructions or revisions in the situation of failure. MCPJ arthrodesis stands for another treatment option in conditions of non-salvageable reconstruction joint or associated tissues. Many techniques have been described. This procedure is generally indicated in higher demand and young patients with MCPJ instability. The goal is to provide a stable and painless union. However, joint arthrodesis results in loss of joint motion, limitation, and impairment of hand function, possible non-union with bone shortening, and hardware failure. In the treatment of severely traumatized joints, we can also retain an essential practice with vascular autogenous joint transfer, especially the use of the second toe. Dautel [9] recommends this MCPJ reconstruction in children and young adults with dominant finger joints and high functional demands, aiming to restore ROM and growing capacities for long-running outcomes. Their performance in 11 cases of MCP destruction after trauma showed a mean amplitude of 60° of active ROM (35°–80°) at 50 months of mean follow-up, slightly inferior or similar to the results pulled off by implant arthroplasty in terms of final ROM. Taking this into consideration, this surgical solution remains suitable in cases when fusion and arthroplasty are contraindicated. Our patient refused this intervention. Large defects around MCPJ involving bone, tendons, and soft tissues, after tumor resection or trauma, can also be managed by osteoarticular allograft replacement, which is still a current alternative to prosthetic implantation. The benefit of this technique is restoring at the same time digital length, bone stock, tendon, and soft-tissue integrity. Compared to autogenous joint transfer, banked allograft joints present the advantage of the absence of donor site defect with the corresponding arc of flexion in terms of ROM [10]. In case of complications resulting from this highly demanding surgical technique and possible infection, leading to failed treatment, amputation, or arthrodesis could become a salvageable treatment option [11].
Although amputation seems to be an extreme measure, this solution should be conceived and performed if the injuries occur in the proximal segment of the digit, when there is a combined sensory deficit, and when endless attempts are done to restore normal anatomy but do not meet the expected function. This operation is generally carried out as a secondary procedure, before warning the patient about the development of dysesthesia, impairment, or loss of hand force.
Our satisfactory results show that in patients presenting MCPJ trauma with bone loss, prosthetic arthroplasty should be considered in the acute setting among many alternative strategies and salvage procedures to preserve painless immediate mobilization and provide the best functional outcome.
References
- 1.Pomares G, Pauchard N, Dap F, Dautel G. An articular spacer for metacarpophalangeal fracture: The story of a crocodile bite. Hand Surg Rehabil 2016;35:371-4. [Google Scholar]
- 2.Tupper JW. The metacarpophalangeal volar plate arthroplasty. J Hand Surg Am 1989;14:371-5. [Google Scholar]
- 3.Zappaterra T, Obert L, Pauchot J, Lepage D, Rochet S, Gallinet D, et al. Post-traumatic reconstruction of digital joints by costal cartilage grafting: A preliminary prospective study. Chir Main 2010;29:294-300. [Google Scholar]
- 4.Foucher G, Hoang P, Citron N, Merle M, Dury M. Joint reconstruction following trauma: Comparison of microsurgical transfer and conventional methods: A report of 61 cases. J Hand Surg Br 1986;11:388-93. [Google Scholar]
- 5.Nagle DJ, af Ekenstam FW, Lister GD. Immediate silastic arthroplasty for non-salvageable intraarticular phalangeal fractures. Scand J Plast Reconstr Surg Hand Surg 1989;23:47-50. [Google Scholar]
- 6.Xie F, Lan X, Lin J. Arthroplasty for treating traumatic metacarpophalangeal joint defects: A retrospective study over three years. J Pain Res 2021;14:1457-64. [Google Scholar]
- 7.Pomares G, Jager T. Emergency metacarpophalangeal arthroplasty with bone grafting for traumatic joint destruction: A report on two cases. Hand Surg Rehabil 2021;40:104-8. [Google Scholar]
- 8.Houdek MT, Wagner ER, Rizzo M, Moran SL. Metacarpophalangeal joint arthroplasty in the setting of trauma. J Hand Surg Am 2015;40:2416-20. [Google Scholar]
- 9.Dautel G. Vascularized toe joint transfers to the hand for PIP or MCP reconstruction. Hand Surg Rehabil 2018;37:329-36. [Google Scholar]
- 10.Innocenti M, Adani R, Boyer MI. Nonvascularized osteoarticular allograft replacement of the proximal interphalangeal joint after extensive loss of bone, joint, and extensor tendon. Tech Hand Up Extrem Surg 2007;11:149-55. [Google Scholar]
- 11.Baltzer HL, Moran SL. The biomechanical impact of digital loss and fusion following trauma: Setting the patient up for success. Hand Clin 2016;32:443-63. [Google Scholar]







