Olecranon fracture fixation involves selecting the treatment plan not only based on the fracture attributes such as pattern, and level but also the condition of the overlying skin and soft tissues.
Dr. Tanmay Avhad, Department of Orthopaedics, B.Y.L Nair Charitable Hospital, Mumbai, Maharashtra, India. E-mail: tanmayavhad@gmail.com
Introduction: Olecranon fractures with compromised overlying skin such as superficial and deep abrasions and puncture wounds pose a challenge to manage as they are at a higher risk of wound and hardware-associated complications such as wound dehiscence, infection, gaping, and prominent hardware. Management of such fractures requires a holistic approach with special attention to the skin and soft tissues.
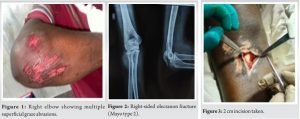
Case Report: This case highlights a 28-year-old male with a history of falls from a bike resulting in the right comminuted displaced olecranon fracture with multiple superficial abrasions which was managed with a thorough wound wash, antibiotics for 3 days after which percutaneous tension band wiring was performed through a 3 cm incision to prevent any wound complications. Rehabilitation and physical therapy were started immediately and the patient restored the complete range of motion at the elbow thus resuming his activities of daily living.
Conclusion: Utilizing a percutaneous technique for fixation in closed olecranon fractures with compromised overlying skin is considered an innovative, secure, dependable, and effective approach.
Keywords: Percutaneous, olecranon, tension-band wiring, wound healing, K-wire.
Fractures of the olecranon account for up to 40% of all fractures around the elbow joint and account for approximately 20% of fractures of the proximal part of the forearm [1,2]. Non-operative approaches might be contemplated for low-demand patients, while surgical fixation is advisable for active individuals with displaced fractures. Classification systems designed for olecranon fractures are descriptive and differentiated based on both the location of the median fracture line and the morphological characteristics. In adherence to the Mayo classification, olecranon fractures are categorized according to factors influencing treatment decisions, such as displacement, comminution, and the presence of dislocation or subluxation in the articular joint surface [3] Tension-band wire (TBW) fixation is a frequently utilized method for managing simple, isolated, stable displaced olecranon fractures [2, 3], while on the contrary plate osteosynthesis also has good outcomes. Biomechanical principles of the TBW construct are based on the hypotheses of absolute fracture stability, exploiting functional limb movement, and converting tensile forces into compression through the actions of the triceps and brachialis. The plan of open reduction and fixation with the above methods often gets complicated with poor skin conditions such as blebs or superficial and deep abrasions this poses a high risk of poor wound healing and infection. Management of such a case warrants the use of minimal incision, restoring articular congruity, providing stable reliable fixation, and allowing early mobilization to minimize joint stiffness.
A 28-year-old male came to the emergency department with a history of falls from a bike. The examination was done as per advanced trauma life support protocol [4], and vitals were found to be within normal limits. On clinical examination, it was found that the patient had a superficial wound over the skin over the left olecranon and proximal ulna (Fig. 1) and radiographs confirmed a right comminuted displaced olecranon fracture (Fig. 2). Further, the wound was thoroughly washed, the limb was immobilized and the patient was started on broad-spectrum antibiotics. Due to the poor skin condition, a Plan for tension band wiring using a minimal incision was planned in due course.
The steps taken are as follows:
- Under anesthesia, the tourniquet was applied above the elbow of the affected arm. The patient is positioned laterally, with the affected elbow placed over a side post. The surgical site was prepared through painting and draping. The elbow joint is maintained in full extension to facilitate the reduction of the olecranon fracture (Fig. 3)
- A 2 cm incision was made on the upper 1/4th of the posterior aspect of the ulna, and retraction was achieved using two Dura retractors. A 3.2 mm drill bit was utilized to create a drill hole (tunnel) in the proximal one-fourth of the olecranon process. A 1 cm loop was fashioned from a 0.8 mm stainless steel wire spool measuring 20 inches long (Fig. 4)

- The wire loop is then passed through the tunnel in the proximal ulna. 2 mm Kirschner wire, 9 inches, is inserted superior to the olecranon under the triceps tendon from lateral to medial, taking care to perform this step only in an extended elbow to protect the ulnar nerve (Fig. 5)

- A 2 mm Kirschner wire is inserted from the incision site on the proximal ulna to the exit site of the horizontal Kirschner wire. A Jamshidi needle or curvilinear wire passer is passed over the Kirschner wire from superior to inferior. The lateral end of the stainless-steel wire is threaded through the needle and brought out superomedially. The wire loop is passed in a similar manner from the superomedial portal to the superolateral portal (Fig. 6)

- A J needle is passed over the Kirschner wire from the superolateral portal to the superomedial portal. The wire loop is passed in a similar manner from the superolateral portal to the incision site using the Kirschner wire and J needle (Fig. 7). Reduction is attempted by pushing the fragment downward and by flexion and extension at the elbow joint

- Both ends of the stainless-steel wire loop are tied around using pliers. Elbow flexion and extension are performed, and the reduction is verified under the c-arm (Fig. 8)

Post-operative radiographs of the olecranon were taken (Fig. 9).
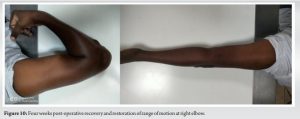
Mobilization begins on the 2nd post-operative day based on the patient’s pain tolerance. Sutures are removed after 2 weeks, and regular follow-ups are conducted. The wound healed over the next 2 weeks and the patient got a complete range of motion at the end of 4 weeks (Fig. 10) following physical therapy and regular follow-ups.
Olecranon fractures can be managed either conservatively or surgically with open reduction and internal fixation with tension band wiring and k wires or plating, as per Ronald, fixation with tension band wiring and plate was associated with various complications such as wound dehiscence, prominent hardware, loss of fixation, infection, and wound gaping [5]. Percutaneous fixation maintains the integrity of soft-tissue biology by avoiding the dissection of soft tissues. This method results in minimal blood loss, reducing overall morbidity and rendering it suitable for patients, including patients with superficial and deep abrasions, namely Grade 2 and 3 (Oestern and Tscherne Classification) [6] and Grade 1 (Gustilo Anderson classification) [7] along with those at high risk for surgery. The risk of infection is also minimized since there is no traditional skin incision. In contrast, the open method, involving the dissection of soft tissues, makes it challenging to align all fragments. Romero et al. have documented various complications associated with olecranon fractures treated using tension band wiring in open procedures such as s wire breakage, skin impingement, wire back out, bursitis, ulcer formation, and infection over the wound [8]. These complications have a higher rate of occurrence as the skin overlying the olecranon and proximal 1/3rd of the ulna is thin and predisposed to superficial injuries. AD Sane et al in this study in 2008 for assessment of patients operated with tension band wiring using mayo elbow performance score provided insight on the good clinical and radiological union rates among sixty-three patients ensuring restoration of elbow range of motion and active rehabilitation [9]. Brink et al conducted a detailed examination of the tension band principle in 2012 to test the compression system being static or dynamic. The researchers utilized six fresh frozen cadaveric upper limbs treated with tension band wiring and subjected them to different loading protocols. Interestingly, none of the six fractures exhibited secondary dislocation with dynamic compression of the tension band principle was only attained when the elbow was actively extended against gravity within the range of 30° to 120° [10]. Thus tension band technique offers advantages in preserving soft tissue, facilitating the alignment of comminuted fragments with ease. This approach results in a shorter hospital stay, reducing overall treatment costs proportionally to the decreased duration of hospitalization. In addition, percutaneous fixation minimizes the risk of post-operative bleeding due to unnecessary soft-tissue dissection, thus lowering post-operative morbidity. It also significantly reduces the likelihood of post-operative infections, promoting early mobilization. Employing K-wires, a Jamshedi needle, and stainless-steel wire in this technique facilitated the creation of a tension band effect. This, in turn, promoted the apposition of fracture ends and encouraged healing through the secondary fracture healing process. The outcome included the restoration of range of motion, allowing a return to daily activities. It is important to note that our report has limitations, including a shorter follow-up period.
Utilizing a percutaneous technique for fixation in closed olecranon fractures with compromised overlying skin is considered an innovative, dependable, and effective approach that aims to restore the native anatomy and elbow function without jeopardizing the overlying skin, thereby facilitating quicker wound healing and minimizing complications associated with hardware. Nevertheless, additional studies are needed to refine and compare this treatment technique further.
Fractures of the olecranon are often associated with compromised overlying skin due to their subcutaneous location. This case highlights the importance of a meticulous approach to tissue manipulation and a well-considered fixation strategy. Close attention to the condition of the skin and soft tissues is emphasized, with factors such as incision length and timing of surgery being crucial considerations in the treatment plan. The choice of hardware and the adaptation of fixation methods to suit the specific case are also vital for achieving optimal outcomes.
References
- 1.Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury 2012;43:343-6. [Google Scholar]
- 2.Chalidis BE, Sachinis NC, Samoladas EP, Dimitriou CG, Pournaras JD. Is tension band wiring technique the “gold standard” for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg Res 2008;3:9. [Google Scholar]
- 3.Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect 1995;44:175-85. [Google Scholar]
- 4.ATLS Subcommittee, American College of Surgeons’ Committee on Trauma, International ATLS working group. Advanced trauma life support (ATLS®): The ninth edition. J Trauma Acute Care Surg 2013;74:1363-6. [Google Scholar]
- 5.Navarro RA, Hsu A, Wu J, Mellano C, Sievers D, Alfaro D, Foroohar A. Complications in olecranon fracture surgery: A comparison of tension band Vs. Plate osteosynthesis. Arch Bone Jt Surg 2022;10:863-70. [Google Scholar]
- 6.Ibrahim DA, Swenson A, Sassoon A, Fernando ND. Classifications in brief: The tscherne classification of soft tissue injury. Clin Orthop Relat Res 2017;475:560-4. [Google Scholar]
- 7.Kim PH, Leopold SS. In brief: Gustilo-Anderson classification. Clin Orthop Relat Res 2012;470:3270-4. Erratum in: Clin Orthop Relat Res 2012;470:3624. Erratum in: Clin Orthop Relat Res 2019;477:2388. [Google Scholar]
- 8.Romero JM, Miran A, Jensen CH. Complications and reoperation rate after tension-band wiring of olecranon fractures. J Orthop Sci 2000;5:318-20. [Google Scholar]
- 9.Sane AD, Lo M, Dieme C, Ndiaye-Coulibaly NF, Bousso A, Ndiaye A, Sy MH, Seye SI. Evaluation du traitement chirurgical par haubanage des fractures de l'olecrane. A propos de 63 cas [Assessment of surgical treatment of olecranon fractures by tension-band wiring. About 63 cases]. Mali Med. 2008;23(1):47-9. French. PMID: 19437816. [Google Scholar]
- 10.Brink PR, Windolf M, de Boer P, et al. Tension band wiring of the olecranon: is it really a dynamic principle of osteosynthesis? Injury. 2013;44(4):518–522. [PubMed] [Google Scholar] [Google Scholar]










