Severe valgus deformity may rarely occur following high tibial osteotomy and can be treated with joint-sparing surgery.
Dr. Bünyamin Kılıçlı, Department of Orthopedics and Traumatology, Ege University School of Medicine, 35040, Izmir, Turkey. E-mail: kiliclibunyamin@gmail.com
Inroduction: In the treatment of medial gonarthrosis, the high tibial osteotomy (HTO) is recognized as an effective joint-sparing surgical procedure. Severe valgus deformity is not a common complication after HTO. There are no cases in the literature reporting valgus deformity of 10° or more after HTO.
Case Report: An open-wedge HTO was performed on a 57-year-old female patient due to left knee pain and varus deformity. In this case, a progressive and severe valgus deformity occurred during follow-up. The severe valgus deformity was then corrected using an inverted V-shaped (hemi-closing, hemi-opening) HTO.
Conclusion: Valgus deformity after HTO is not common. There are various factors that can lead to post-HTO valgus deformity; although no cases of valgus deformity exceeding 10° have been described. Intra-operative releasing of the superficial medial collateral ligament and associated lateral hinge fracture was a risk factor for overcorrection. This case aims to uncover the factors contributing to the development of severe valgus deformity subsequent to HTO and to present solutions for its management.
Keywords: Case report, high tibial osteotomy, valgus deformity, biplanar osteotomy.
High tibial osteotomy (HTO) is a treatment option with good results in active patients with medial gonarthrosis and varus deformity [1]. In recent years, with the development of implant technology, rigid fixation has become possible, therefore medial open wedge HTO has increased its popularity. The incidence of postoperative complications has increased with the frequent use of medial open wedge osteotomy. The most common complications after HTO are superficial infection (2%), loss of correction (1.2%), nonunion, lateral hinge fracture, and peroneal nerve damage [2]. Lateral hinge fracture may cause loss of correction, non-union, or delayed union of the osteotomy line [3]. The cause of the lateral hinge fracture is unknown. In cases with lateral cortex fractures, bone grafting, the use of another fixation system, or the use of additional lateral fixation is recommended [3]. During open wedge HTO, the superficial medial collateral ligament (sMCL) is cut to facilitate mechanical axis correction and reduce the loading on the medial compartment. Although it is stated that this procedure may cause valgus laxity, there are studies indicating that it will not cause laxity [4-6]. In the case report we will present, intraoperative sMCL was released in a case in which open wedge HTO was performed due to medial gonarthrosis. A stable lateral hinge fracture occurred as an intraoperative complication. A progressive valgus deformity occurred during follow-up, and the deformity was corrected with an inverted V-shaped (hemi-closing-hemi-opening) osteotomy. Through this case, we aim to reveal the causes of severea valgus deformity that occurs after HTO and to illuminate solutions.
A 57-year-old female patient presented to our clinic complaining of pain in the medial aspect of the left knee. The pain is progressive and increases with standing. There is no history of trauma, locking, or wasting of the knee. On physical examination, there is tenderness over the left medial tibial plateau and varus deformity of the left knee. Lachman, anterior drawer test, posterior drawer test, and McMurray tests are negative. Radiographs show medial joint space narrowing and varus deformity of 9.4°, with a medial proximal tibial angle (mMPTA) of 85.1° (Fig. 1). The patient was scheduled for an open-wedge HTO with a diagnosis of medial compartment arthrosis.

First surgical procedure
Under general anesthesia, prophylactic antibiotic was given intravenously and a tourniquet was applied and inflated to 300 mmHg for 120 min. The first stage of the operation was an arthroscopic examination. A degenerative medial meniscus tear was found and debridement was performed. There was Outerbridge Grade 3 chondral damage in the medial compartment. The quality of the lateral compartment cartilage was sufficient for a valgus osteotomy. After diagnostic arthroscopy, a longitudinal incision was made over the proximal tibia, the sMCL was split and an osteotomy was made with a saw from the medial cortex to the proximal tibiofibular joint. The osteotomy was then opened. A 12° correction was performed and the osteotomy was fixed with a locking plate. An autologous bone graft harvested from the left iliac crest was used to fill the gap. Knee flexion exercises using a continuous passive motion device were initiated on the 1st day after surgery. The patient was mobilized with double crutches on the same day. For 6 weeks after the operation, the patient was mobilized without weight-bearing. Post-operative radiographs are shown in Fig. 2.

After the 6th post-operative week, the patient was mobilized with a crutch and partial weight-bearing. The telemetric radiograph in Fig. 3 in the sixth post-operative week showed 1.7° valgus and no union in the osteotomy line.

In the 10th week after the operation, imaging of the patient shows remarkable callus tissue in the lateral hinge of the tibia. A telemetric radiograph taken on the 14th week after the operation shows a 4.9° valgus and callus on the lateral hinge (Fig. 4).

The patient applied with a complaint of inability to walk at the 8th month post-operation. There is no history of trauma, locking, or wasting in the knee. Physical examination revealed negative results for the Lachman, anterior drawer, and McMurray tests. The patient has a 15° flexion contracture. Valgus and varus stress tests were negative. Telemetric images from the 8th month after the first surgery show an 8.3° valgus deformity (Fig. 5).

Callus tissue is present in the lateral hinge of the tibia, and atrophic union has occurred in the osteotomy line. On evaluation in the 1st year after the first surgery, the patient reported difficulty walking. The patient is able to mobilize with the aid of double crutches. Physical examination revealed a 15° flexion contracture and a negative varus/valgus stress test. Telemetric radiographs showed a 19.8° valgus deformity of the mechanical axis and a mMPTA of 97° (Fig. 6). Based on these findings, it was decided that revision surgery was necessary for the patient.

Revision procedure: Biplanar inverted V osteotomy (hemi-closing, hemi-opening)
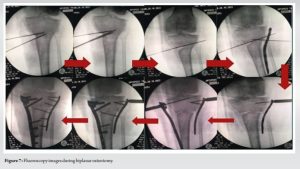
Under general anesthesia, prophylactic antibiotics were administered intravenously, and a tourniquet was applied and inflated to 300 mmHg for 120 min. The left lower extremity was draped appropriately. The plate and screws were removed using the old posteromedial incision. An oblique osteotomy was performed from the diaphysis, approximately 18 cm proximal to the left fibula type. A butterfly fragment occurred as a complication during the oblique osteotomy. The proximal tibiofibular joint was targeted, and appropriate Kirschner wires were inserted under fluoroscopy guidance. A hemi-osteotomy was then performed by targeting the proximal tibiofibular joint from the medial aspect of the proximal tibia using a suitable saw. The osteotomy was terminated in the middle of the tibial metaphysis. A triangular bone fragment was removed from the osteotomy line. The lateral osteotomy was planned to join the medial osteotomy and form an inverted V shape. Kirschner wires were applied and the lateral osteotomy was performed. The opening gap of the lateral osteotomy line was checked and opened laterally with an osteotomy angle ruler. A correction of approximately 13° was made, resulting in an improvement of the leg’s mechanical axis. The bone block taken from the medial side was inserted into the lateral osteotomy opening. A proximal lateral tibia anatomical plate was then placed on the lateral side, and a HTO plate was placed on the medial side (Fig. 7).
The layers were properly sealed, and a drain was inserted. The patient was mobilized using an immobilizer and double crutches without weight-bearing for 6 weeks. Partial loading was permitted at the end of the 6th week. The telemetric radiograph taken 6 weeks after the second operation showed a mechanical axis of 3.7° valgus and an mMTPA angle of 87.6° (Fig. 8).

No flexion contracture was observed during examination. Union had not yet occurred in the osteotomy line. Mobilization with a single crutch was allowed after the sixth post-operative week. At the 6th week after surgery, X-rays revealed that the fibula had not yet healed, hypertrophic callus tissue was visible, but the patient did not exhibit any symptoms. Our patient exhibited complete union of the osteotomy line during the 3rd month after the second surgery (12th post-operative week). In the first post-operative year, the telemetric radiographs show a 2.1° valgus. The fibula osteotomy healed with hypertrophic callus during this period and the patient did not experience any related symptoms. There is no flexion contracture, and the joint range of motion is full and painless. The patient can be mobilized without any external support. The mMTPA was measured at 89.6° (Fig. 9).

HTO stands out as a joint-preserving surgery in the treatment of medial gonarthrosis. Appropriate patient selection is very important in HTO. With developing of implant technologies, complication rates have decreased. The most common complications are correction problems, wound site problems, and lateral hinge fractures [2, 3]. Valgus deformity is not a common problem after open wedge HTO. Many reasons are given for overcorrection after HTO [7-9]. For some authors, overcorrection may occur due to existing soft-tissue laxity [7-11]. The most common method for quantifying soft-tissue laxity is evaluating the joint line convergence angle (JLCA) [9]. Lee et al. [9] evaluated medial laxity preoperatively with JLCA change and reported that large JLCA change was associated with overcorrection. In addition, the release of the superficial MCL may also affect JLCA change. Park et al. [11] that the likelihood of overcorrection is high for JLCA changes of ≥4°. In our case, the JLCA was 6.0° varus on the pre-operative loading knee radiograph, and the JLCA was 2.3° valgus on the pre-operative valgus stress radiograph. The change is 8.3° (Fig. 10).

This is a risk factor for overcorrection. The lateral cortex is important for the primary stability of the osteotomy line [12]. Lateral cortex fracture, an intraoperative complication, is thought to be a risk factor for incorrect correction [13]. In addition, since lateral cortex fracture reduces the stability of the osteotomy line, it may delay the healing of the osteotomy line as well as the correction defect [14]. In our case, a stable lateral hinge fracture occurred intraoperatively. Callus tissue formed in the lateral cortex of the tibia due to micromotion in the osteotomy line is seen (Fig. 4 and 7). A progressive valgus deformity occurred in our patient as the lateral cortex fracture accompanied the large JLCA change. Inverted V-shaped HTO is an advantageous technique compared to closed wedge high tibial osteotomies used in medial compartment osteoarthritis with varus deformity [15]. It is frequently used in high varus deformities and does not require additional grafting [15]. In our patient with Mmpta: 97° after the first operation, biplanar osteotomy (medial hemi-closing, lateral hemi-opening) was performed for newly developed tibial valgus deformity. After the second operation, mMTPA was 87.6°. Successful union and proper mechanical axis were achieved in the post-operative follow-up. As a limitation, complications during fibular osteotomy also led to the risk of nonunion. Otherwise, the presence of an intact fibula will not allow making appropriate degrees of corrections [16]. Union was achieved within the first post-operative year. Our case is a leading case in terms of the use of biplanar inverted V osteotomy for valgus deformity, which is used for varus deformity in the treatment of severe valgus deformity after open wedge osteotomy.
HTO is a joint-sparing surgery with appropriate patient selection. However, complications can be difficult to manage. Valgus deformity of 10° or more is not a common complication after HTO. Although cutting the superficial MCL facilitates proper alignment, it may result in a medial laxity of the knee. In addition, a stable lateral hinge fracture has been associated with a progressive tibial valgus deformity. Our case is of interest in this respect.
High JLCA change and intraoperative lateral hinge fracture are risk factors for overcorrection in high tibial osteotomies performed at high varus degrees. The occurrence of more than one complication may increase the degree of overcorrection.
References
- 1.Loia MC, Vanni S, Rosso F, Bonasia DE, Bruzzone M, Dettoni F, et al. High tibial osteotomy in varus knees: Indications and limits. Joints 2016;4:98-110. [Google Scholar]
- 2.Miltenberg B, Puzzitiello RN, Ruelos VC, Masood R, Pagani NR, Moverman MA, et al. Incidence of complications and revision surgery after high tibial osteotomy: A systematic review. Am J Sports Med 2023;52:258-68. [Google Scholar]
- 3.Dexel J, Fritzsche H, Beyer F, Harman MK, Lützner J. Open-wedge high tibial osteotomy: Incidence of lateral cortex fractures and influence of fixation device on osteotomy healing. Knee Surg Sports Traumatol Arthrosc 2017;25:832-7. [Google Scholar]
- 4.Pape D, Duchow J, Rupp S, Seil R, Kohn D. Partial release of the superficial medial collateral ligament for open-wedge high tibial osteotomy. A human cadaver study evaluating medial joint opening by stress radiography. Knee Surg Sports Traumatol Arthrosc 2006;14:141-8. [Google Scholar]
- 5.van Egmond N, Hannink G, Janssen D, Vrancken AC, Verdonschot N, van Kampen A. Relaxation of the MCL after an open-wedge high tibial osteotomy results in decreasing contact pressures of the knee over time. Knee Surg Sports Traumatol Arthrosc 2017;25:800-7. Erratum in: Knee Surg Sports Traumatol Arthrosc 2017. [Google Scholar]
- 6.Seitz AM, Nelitz M, Ignatius A, Dürselen L. Release of the medial collateral ligament is mandatory in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2019;27:2917-26. [Google Scholar]
- 7.Kyung BS, Kim JG, Jang KM, Chang M, Moon YW, Ahn JH, et al. Are navigation systems accurate enough to predict the correction angle during high tibial osteotomy? Comparison of navigation systems with 3-dimensional computed tomography and standing radiographs. Am J Sports Med 2013;41:2368-74. [Google Scholar]
- 8.Böhle S, Bischoff L, Ehrenmann K, Layher F, Sander K, Matziolis G, et al. Forgivingness of an anteromedially positioned small locked plate for high tibial osteotomy in case of overcorrection and lateral hinge fracture. Life (Basel) 2022;12:1265. [Google Scholar]
- 9.Lee DK, Wang JH, Won Y, Min YK, Jaiswal S, Lee BH, et al. Preoperative latent medial laxity and correction angle are crucial factors for overcorrection in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2020;28:1411-8. [Google Scholar]
- 10.Heijens E, Kornherr P, Meister C. The coronal hypomochlion: A tipping point of clinical relevance when planning valgus producing high tibial osteotomies. Bone Joint J 2016;98-B:628-33. [Google Scholar]
- 11.Park JG, Kim JM, Lee BS, Lee SM, Kwon OJ, Bin SI. Increased preoperative medial and lateral laxity is a predictor of overcorrection in open wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2020;28:3164-72. [Google Scholar]
- 12.Meidinger G, Imhoff AB, Paul J, Kirchhoff C, Sauerschnig M, Hinterwimmer S. May smokers and overweight patients be treated with a medial open-wedge HTO? Risk factors for non-union. Knee Surg Sports Traumatol Arthrosc 2011;19:333-9. [Google Scholar]
- 13.Song JH, Bin SI, Kim JM, Lee BS. Unstable lateral hinge fracture or occult complete osteotomy adversely affects correction accuracy in open-wedge high tibial osteotomy. Arthroscopy 2021;37:3297-306. [Google Scholar]
- 14.Miller BS, Downie B, McDonough EB, Wojtys EM. Complications after medial opening wedge high tibial osteotomy. Arthroscopy 2009;25:639-46. [Google Scholar]
- 15.Kondo E, Yasuda K, Yabuuchi K, Aoki Y, Inoue M, Iwasaki N, et al. Inverted V-shaped high tibial osteotomy for medial osteoarthritic knees with severe varus deformity. Arthrosc Tech 2018;7:e999-1012. [Google Scholar]
- 16.Bicer EK, Basa CD, Gunay H, Aydogdu S, Sur H. The fate of fibular osteotomies performed during high tibial osteotomy. Arch Orthop Trauma Surg 2016;136:1085-90. [Google Scholar]
- 17.Ramanoudjame M, Vandenbussche E, Baring T, Solignac N, Augereau B, Gregory T. Fibular nonunion after closed-wedge high tibial osteotomy. Orthop Traumatol Surg Res 2012;98:863-7. [Google Scholar]







