Remission of S. marcescens infection was achieved without removing the implant by cleaning, debridement, and use of sensitive antimicrobial agents.
Dr. Shuro Furuichi, Department of Bone and Joint Surgery, Kawasaki Medical School, 577 Matsushima, Kurashiki, Okayama 701-0192, Japan. E-mail: rwjnf672@yahoo.co.jp
Introduction: Recently, Serratia marcescens was reported to cause nosocomial infections.
Case Report: In this study, we report a case of S. marcescens infection occurring after total knee arthroplasty (TKA) in a 72-year-old woman. The patient had undergone TKA for knee osteoarthritis. She had a past medical history of diabetes mellitus, for which she was receiving cefazolin sodium. Six days after surgery, redness and effusion were observed in the wound, and post-operative infection was suspected. Thus, the patient was treated with linezolid, clindamycin, and tazobactam/piperacillin hydrate post-operatively. Twelve days after TKA, reinfection was suspected; hence, washing and debridement were repeated.
Conclusion: In this case, remission of S. marcescens infection was achieved without the need to remove the implant by cleaning, debridement, and the use of sensitive antimicrobial agents.
Keywords: Total knee arthroplasty, Serratia infection, antibiotics, debridement, implant retention.
Infection after total knee arthroplasty (TKA) is a serious complication that is often difficult to treat and can severely affect the subsequent activities of daily living (ADL). In particular, surgical site infection (SSI) is a major cause of unexpected readmission [1, 2], requires prolonged treatment, decreases patient satisfaction, and leads to other complications. In recent years, nosocomial infections caused by Serratia marcescens have become a major problem [3]. Most post-operative infections in orthopedic surgery are caused by gram-positive bacteria, and periarticular infections caused by S. marcescens are extremely rare. We report a valuable and relatively rare case of S. marcescens infection after TKA and its successful management by two rounds of debridement, antibiotics, implant retention (DAIR), and culture-guided antimicrobial therapy.
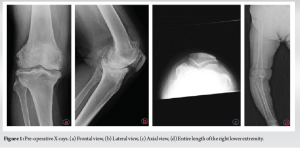
A 72-year-old woman was referred to our hospital for surgery because of severe and progressive left knee pain for the past decade. Her pre-operative ADLs ranged from walking with a single cane to walking with a silver car. Her medical history included diabetes mellitus, with a glycated hemoglobin level of 7.6%. Pre-operative radiographs of the right lower extremity were shown (Fig. 1).
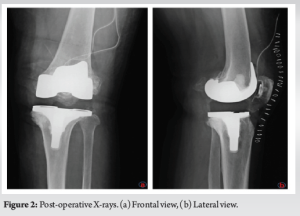
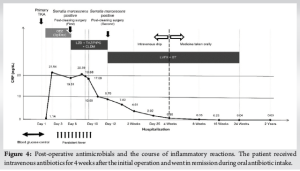
The patient was placed under general anesthesia, and isodine was used to disinfect the knee area during surgery. TKA was performed using a medial parapatellar approach (Fig. 2). The operative time was 1 h and 39 min, and an air tourniquet was used to avoid massive bleeding. Cefazolin sodium was given intra-operatively as a single dose of 2 g intravenously and was continued post-operatively at an infusion dose of 3 g/day for 3 days. On post-operative day 6 (POD), increased exudates and erythema on the wound and fever were noted. Blood tests revealed a normal white blood cell count (7.47 × 103 cells/µL) and neutrophil count (5.93 × 103 cells/µL), but an elevated C-reactive protein (CRP) level at 19.51 mg/dL, indicating an increased inflammatory response. Examination of the joint fluid was positive for α-defensin [4, 5].
Considering the extremely high possibility of infection, the patient underwent an initial cleaning procedure after obtaining samples for culture studies. Surgery was performed by opening the previous skin incision. Intra-operatively, tissue perfusion was poor in some areas, but abscess formation was scant, and contaminated tissues were removed as much as possible. The soft tissue and other replaceable inserts were replaced, and a drain was placed. At our hospital, the antimicrobial regimen for SSIs is an intravenous three-drug combination of linezolid (LZD) to cover MRSA; tazobactam/piperacillin hydrate to cover gram-positive and gram-negative bacteria, especially Pseudomonas aeruginosa; and clindamycin (CLDM) to address the possibility of intracellular transfer of bacteria [6]. Post-operatively, the patient was started on infusions of the following antimicrobials: 600 mg of LZD 2 times daily, 4.5 g of tazobactam/piperacillin hydrate 3 times daily, and 600 mg of CLDM 3 times daily.
The culture results from the initial surgery became available only on POD 12 and revealed S. marcescens. At this time, the drainage increased, and a fever of 38°C appeared (Fig. 3a). In addition, the CRP level was 9.7 mg/dL, and the white blood cell and neutrophil counts increased to 9.11 × 103 cells/μL and 7.95 × 103 cells/μL, respectively. The presence of erythema around the wound and purulent drainage indicated that the TKA infection had not completely subsided and had even worsened. With the identification of the causative organism, retreatment with DAIR was deemed likely to be effective. The same skin incision site was used for the procedure. After obtaining joint fluid for culture examination, further washing and debridement were performed. Considering reinfection, the area was washed with 10 L of saline solution, and hemochromatic tissues were removed as much as possible. The implant was not loosened and was retained, but the insert was replaced, and a drain was placed. Culture-guided antimicrobial treatment with intravenous levofloxacin and sulfamethoxazole was administered. After the second cleaning, the CRP level rapidly decreased.
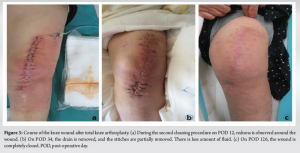
After the detection of S. marcescens, DAIR led to a rapid decrease in the CRP level. Four weeks after the initial TKA, the CRP level decreased to 0.8 mg/dL. Subsequently, all antimicrobials were switched to oral therapy. At 34 days after TKA, the wound (Fig. 3b). At 16 weeks after TKA, the CRP level further decreased to 0.03 mg/dL, and the symptoms of erythema and burning sensation gradually improved. The wound was completely closed (Fig. 3c), and the patient was able to walk with a silver car for short distances. The entire course after TKA is shown in Fig. 4. There was no recurrence of infection at the time of the last follow-up, 2 years after TKA.
S. marcescens is a gram-negative rod bacterium that is widely distributed in water and soil [1] and is characterized by resistance to many antimicrobial agents [7, 8]. It has been reported to cause some nosocomial infections in pregnant women and at neonatal intensive care units [9, 10], but it more commonly causes opportunistic infections in immunocompromised patients [11]. In Japan, more than 110,000 cases of hip replacement are performed annually [12], and the reported incidence of deep SSI after initial arthroplasty was 2.2% (40 of 1837 cases) [13]. Furthermore, culture studies of 50 superficial SSI cases after orthopedic surgery revealed that most of these infections were caused by gram-positive bacteria, with Staphylococcus aureus accounting for 64% [14]. Patient factors, such as body mass index and history of diabetes [15, 16], and environmental factors, such as surgical environment and hygiene techniques, have been considered to increase the risk for periprosthetic infections [17]. In the study by Anagnostakos et al. on 165 cases of periprosthetic infections after total hip arthroplasty and TKA, 2 (1.4%) were caused by S. marcescens [18]. In that report, the choice was a two-stage treatment, but the details of the treatment were not provided, except for the use of ciprofloxacin. There had been only one case report on S. marcescens infection in an artificial knee joint [19]. Although epidural abscesses [20] and osteomyelitis [21] caused by S. marcescens have been previously reported, there have been no reports of S. marcescens infection after TKA in Japan. Because this patient had underlying diabetes mellitus, the risk of infection was presumably high. In addition, this case was resistant to the drugs for gram-positive bacteria, which are commonly targeted during the peri-operative period. S. marcescens is known to be resistant to penicillins and first-generation cephalosporins but has good susceptibility to third- and fourth-generation cephalosporins, carbapenems, quinolones, and tetracyclines [22]. Similarly, in this case, the culture studies revealed resistance to first- and second-generation cephalosporins. If cephalosporins are ineffective, a change in therapy should be considered. One-stage surgery has been reported to yield satisfactory results for post-arthroplasty infections [23]. At our institution, if there is no implant loosening, we employ DAIR to preserve the implant and replace components as necessary. Early cleaning procedures are usually performed, and ineffective pre-operative antimicrobials are changed as appropriate. Long-term administration of antimicrobials has gained positive opinions in terms of effectiveness [24] and, in this patient, resulted in remission and no recurrence. This case was considered valuable to report because it described the early diagnosis of a Serratia infection after TKA in a patient with poor immune status and the successful use of DAIR for remission without implant removal. Considering the physical burden on the patient, our policy is to perform a two-stage surgery after filling the cement bead using antimicrobials if the infection recurs for the 3rd time. In general, repeated DAIR is not recommended because of its low success rate [25], but it may have value if the causative organism can be identified for appropriate changes to the antimicrobial agents.
S. marcescens infection after TKA has not been reported in Japan and is considered rare. In cases of active infection, antimicrobial therapy that targets only gram-positive bacteria is likely ineffective and should include coverage for gram-negative bacteria, including Serratia species. In this case, remission of S. marcescens infection was achieved without the need to remove the implant by cleaning, debridement, and the use of sensitive antimicrobial agents.
S. marcescens infection after TKA is considered rare and has not yet been reported in Japan. Although DAIR is generally not recommended because of its low success rate, it can be useful to determine whether the pathogen can be identified for appropriate antimicrobial treatment.
References
- 1.Shimizu T, Fujibayashi S, Takemoto M, Otsuki B, Kimura H, Ota M, et al. A multi-center study of reoperations within 30 days of spine surgery. Eur Spine J 2016;25:828-35. [Google Scholar]
- 2.Bernatz JT, Tueting JL, Hetzel S, Anderson PA. What are the 30-day readmission rates across orthopaedic subspecialties? Clin Orthop Relat Res 2016;474:838-47. [Google Scholar]
- 3.Samonis G, Vouloumanou EK, Christofaki M, Dimopoulou D, Maraki S, Triantafyllou E, et al. Serratia infections in a general hospital: Characteristics and outcomes. Eur J Clin Microbiol Infect Dis 2011;30:653-60. [Google Scholar]
- 4.Yuan J, Yan Y, Zhang J, Wang B, Feng J. Diagnostic accuracy of alpha-defensin in periprosthetic joint infection: A systematic review and meta-analysis. Int Orthop 2017;41:2447-55. [Google Scholar]
- 5.Lee YS, Koo KH, Kim HJ, Tian S, Kim TY, Maltenfort MG, et al. Synovial fluid biomarkers for the diagnosis of periprosthetic joint infection: A systematic review and meta-analysis. J Bone Joint Surg Am 2017;99:2077-84. [Google Scholar]
- 6.Valour F, Trouillet-Assant S, Riffard N, Tasse J, Flammier S, Rasigade JP, et al. Antimicrobial activity against intraosteoblastic Staphylococcus aureus. Antimicrob Agents Chemother 2015;59:2029-36. [Google Scholar]
- 7.Lin CS, Horng JT, Yang CH, Tsai YH, Su LH, Wei CF, et al. RssAB-FlhDC-ShlBA as a major pathogenesis pathway in Serratia marcescens. Infect Immun 2010;78:4870-81. [Google Scholar]
- 8.Khanna A, Khanna M, Aggarwal A. Serratia marcescens- a rare opportunistic nosocomial pathogen and measures to limit its spread in hospitalized patients. J Clin Diagn Res 2013;7:243-6. [Google Scholar]
- 9.Chai LY, Rauff M, Ong JS, Kee AC, Teo FS. Serratia septicaemia in pregnancy: further evidence of altered immune response to severe bacterial infection in pregnancy. J Infect 2011;63:480-1. [Google Scholar]
- 10.Voelz A, Müller A, Gillen J, Le C, Dresbach T, Engelhart S, et al. Outbreaks of Serratia marcescens in neonatal and pediatric intensive care units: Clinical aspects, risk factors and management. Int J Hyg Environ Health 2010;213:79-87. [Google Scholar]
- 11.Fedrigo GV, Campoy EM, Di Venanzio G, Colombo MI, García Véscovi E. Serratia marcescens is able to survive and proliferate in autophagic-like vacuoles inside non-phagocytic cells. PLoS One 2011;6:e24054. [Google Scholar]
- 12.Akiyama H, Hoshino A, Iida H, Shindo H, Takakura Y, Miura H, et al. A pilot project for the Japan arthroplasty register. J Orthop Sci 2012;17:358-69. [Google Scholar]
- 13.Petrie RS, Hanssen AD, Osmon DR, Ilstrup D. Metal-backed patellar component failure in total knee arthroplasty: A possible risk for late infection. Am J Orthop (Belle Mead NJ) 1998;27:172-6. [Google Scholar]
- 14.Arciola CR, Cervellati M, Pirini V, Gamberini S, Montanaro L. Staphylococci in orthopaedic surgical wounds. New Microbiol 2001;24:365-9. [Google Scholar]
- 15.Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty 2005;20:46-50. [Google Scholar]
- 16.Ata A, Lee J, Bestle SL, Desemone J, Stain SC. Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg 2010;145:858-64. [Google Scholar]
- 17.Lidwell OM. Clean air at operation and subsequent sepsis in the joint. Clin Orthop Relat Res 1986;211:91-102. [Google Scholar]
- 18.Anagnostakos K, Grzega C, Sahan I, Geipel U, Becker SL. Occurrence of rare pathogens at the site of periprosthetic hip and knee joint infections: A retrospective, single-center study. Antibiotics (Basel) 2021;10:882. [Google Scholar]
- 19.Mahmoud SS, Odak S, Qazzafi Z, McNicholas MJ. Primary total knee arthroplasty infected with Serratia marcescens. BMJ Case Rep 2012;2012:bcr2012006179. [Google Scholar]
- 20.Yang CW, Hsu SN, Liu JS, Hueng DY. Serratia marcescens spinal epidural abscess formation following acupuncture. Intern Med 2014;53:1665-8. [Google Scholar]
- 21.Martins HF, Raposo A, Baptista I, Almeida J. Serratia marcescens osteomyelitis in Cushing’s disease. BMJ Case Rep 2015;2015:bcr2015212872. [Google Scholar]
- 22.Dowzicky MJ, Park CH. Update on antimicrobial susceptibility rates among gram-negative and gram-positive organisms in the United States: Results from the Tigecycline evaluation and surveillance trial (TEST) 2005 to 2007. Clin Ther 2008;30:2040-50. [Google Scholar]
- 23.Jackson WO, Schmalzried TP. Limited role of direct exchange arthroplasty in the treatment of infected total hip replacements. Clin Orthop Relat Res 2000;381:101-5. [Google Scholar]
- 24.Marchionni E, Marconi L, Ruinato D, Zamparini E, Gasbarrini A, Viale P. Spondylodiscitis: is really all well defined? Eur Rev Med Pharmacol Sci 2019;23:201-9. [Google Scholar]
- 25.Fehring TK, Odum SM, Berend KR, Jiranek WA, Parvizi J, Bozic KJ, et al. Failure of irrigation and débridement for early postoperative periprosthetic infection. Clin Orthop Relat Res 2013;471:250-7. [Google Scholar]