Unusual heterotopic ossification (HO) demonstrated after high-force blunt trauma from a motor vehicle collision can present as an uncommon mechanism of injury resulting in femoroacetabular impingement symptoms, and indicated resection of HO anterior to the proximal femur can yield significant pain relief and return of hip joint function despite disparate traumatic etiology.
Dr. Frank McCormick, Beth Israel Deaconess Medical Center at Signature Healthcare, Brockton, Massachusetts. E-mail: drfrankmccormick@yahoo.com
Introduction: A patient presented for recalcitrant right hip pain secondary to femoroacetabular impingement (FAI) after blunt motor vehicle trauma and following the development of a 12 cm heterotopic ossification (HO). FAI is an increasingly recognized diagnosis where the hip joint is exposed to repeated femoral microtrauma from high-level physical activity or trauma, often causing labral ossification, and perhaps underlying a similar biological mechanism to HO.
Case Report: In this case report, we have an otherwise healthy 49-year-old male who was involved in a high-speed motor vehicle collision who was diagnosed with right hip FAI secondary to HO (Brooker’s Class IV) and indicated for surgical excision of the HO anterior to the right proximal femur. The care team and patient initially trialed non-operative conservative treatment with non-steroidal anti-inflammatories drugs (NSAIDs) and hypothesized therapeutic success using a non-surgical approach. Surgical resection was pursued with the patient after a failure of conservative measures. The patient reported a zero out of ten on a ten-point numerical rating scale for pain, he also stated improved quality of life, satisfaction with the procedure, and subsequent rehabilitation at 1-month post-operative follow-up.
Conclusion: HO with near complete ankylosis of the hip joint may be causative of FAI when untreated. Although this case demonstrates a rarely studied traumatic etiology of impingement secondary to HO, initial standard conservative anti-inflammatory treatment can still be pursued. By analyzing the periarticular impact of HO secondary to non-surgical trauma, we can utilize and make inferential correlations from the literature, studying HO and impingement in the setting of prior hip surgery to guide treatment and prognosis in those presenting with FAI symptoms secondary to blunt force trauma.
Key words: Heterotopic ossification, femoroacetabular impingement, blunt trauma.
Heterotopic ossification (HO) is characterized by the formation of extra-skeletal, normal lamellar bone in soft tissues [1, 2]. The degree of HO is described well in the literature, with the classification of HO first defined by Brooker et al. and summarized in Table 1 [3]. Although HO shares the same lamellar bony structure, the HO lacks the periosteal layer found in natural skeletal bone [1].
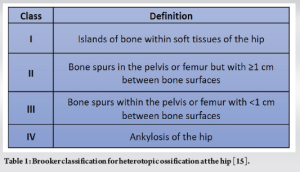
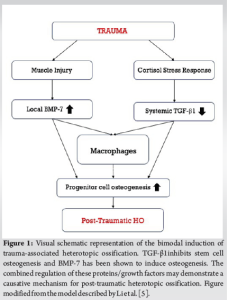
Chalmers et al. state that there are three factors required to induce HO formation on a molecular level: Osteogenic precursor cells, osteoinductive agents, and an osteoconductive environment [4, 5]. At the time of the trauma, there is an inflammation response which is the source of cytokines, chemokines, and other growth factors promoting extraskeletal osteogenesis [4, 6]. A previously proposed model for the pathologic osteogenesis in HO development is demonstrated in Fig. 1. While some HO may be asymptomatic, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroids are still the first line for conservative anti-inflammatory management [1]. HO is typically associated with traumatic or iatrogenic injury. In the setting of trauma, the prevalence of HO has ranged from 15% up to 90% as a result of acetabular fracture or hip arthroplasty [7-8]. The gold standard for traumatic HO treatment is surgical intervention with an excision of the HO [9, 10]. Femoroacetabular impingement (FAI) is an increasingly prevalent diagnosis in trauma, arthroplasty, and sports medicine, but little attention is given to conservative treatment despite a rapid growth in research in recent literature [11, 12]. Pennock et al. also state that the number of hip arthroscopies has increased exponentially following the initial description of FAI by Ganz et al. [12, 13]. To our knowledge, the presence of hip impingement (FAI) symptoms due to blunt trauma associated with HO originating superior to the anterior inferior iliac spine (AIIS) has not been documented in the literature.
Patient data and clinical course
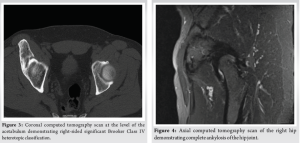
A 49-year-old man suffered a traumatic motor vehicle accident (MVA). The patient stated that he was in the driver’s seat when the incoming vehicle struck the left side of his vehicle. The airbags did not deploy during this accident, and the patient was restrained in his seat by a seatbelt. The patient first presented for medical evaluation regarding his right hip pain 3 months after the MVA. The patient noted at this time the mass was soft in structure, but maintained the same dimensions that were then observed by the care team at the time of surgical excision. A large hematoma, with the exact dimensions undocumented at this time, presented on initial examination at the lateral right hip, anterior to the proximal femoral head. The patient also endorsed a gradual decline in lower extremity mobility since the MVA and was observed with an abnormal gait. At this point, the patient was prescribed Tizanidine and Mobic for the pain and inflammation. In follow-up imaging, the surgeon noted new internal sclerosis of the mass, despite the stable size of the lesion. The patient appraised pain as six out of ten, worsening with activity. At this time, both a computed tomography scan and magnetic resonance imaging were taken and shown in (Fig. 2-4). The pre-operative imaging indicated a large bone density on the right iliac wing extending distally about 12 cm, consistent with Class IV HO. In re-evaluation in the clinic a month later, the patient stated a return of pain after completing prescribed pain medications. He now expressed a pain level of eight out of ten in his anterior hip that worsened with activity but improved with medication. Four months after the initial presentation to the clinic, the surgeon and patient discussed treatment options for the painful lesion, which had hardened significantly since the initial evaluation. Approximately 8 months had elapsed from the inciting trauma to the presentation of a completely ossified mass. During this visit, the patient consented to undergo surgical excision of the HO. The pre-operative assessment was completed before the date of surgery in the outpatient clinic.

Surgical technique
The surgery took place 5 months after the trauma. By the time of surgery, the patient had developed severe FAI of the right hip with overlying myositis ossificans, which significantly impaired the right hip range of motion and function to complete daily recreational and occupational activities. Imaging was taken on the day of the surgery and shown in Fig. 5. This was conducted by the primary surgeon (author F.M.), with the assistance of a vascular surgeon due to the proximity of the femoral artery and vein. The primary surgeon used an anterior Smith–Petersen approach to expose the right hip joint. A 10 cm anterior incision from the lateral curve of the anterior superior iliac spine inferiorly in the direction of the lateral patella was made. The fascial gap between the sartorius and tensor fascia latae was identified, and dissection exposed the ascending branch of the lateral femoral circumflex artery and vein which were cauterized and ligated. Additional deep dissection with retraction of the rectus femoris and gluteus medius exposed the hip capsule and the HO mass is visualized as seen in Fig. 5. The anterior neck of the mass was cut and released from the attached soft tissue. Fluoroscopic guidance was used to confirm the localization of the mass. The rest of the mass was removed in a piecemeal fashion by serial osteotomes and rongeur. Radiofrequency ablation was used for hemostatic control.
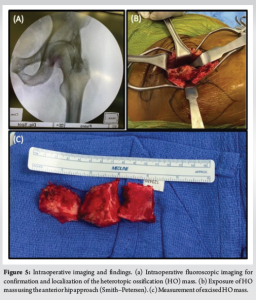
Adequate margins of excision were confirmed by fluoroscopy to reduce the risk of recurrent HO formation, especially as there is an increased incidence of HO following orthopedic surgery [1, 9, 14]. Imaging confirmed excision of the anterior HO lesion, however, imaging also demonstrated additional minimal lateral ossification, not easily accessible through the anterior approach and not affecting the range of motion of the hip. Due to the lack of functional impairment and increased risk of prolonged, unanticipated surgery, this lateral ossification was not removed. The wounds were copiously irrigated, and the hip capsule was reapproximated and tied down. The musculofascial layers were then reapproximated and closed layer by layer with appropriate irrigation and hemostasis. The external wounds were closed, cleaned, and bandaged with clean dressings. Before being taken to the recovery room, an external hip abduction brace was applied to help stabilize the patient’s hip, with hip precautions described to the care team and the patient in post-operative recovery.
Post-operative
The patient was further instructed to continue taking mobic 15 mg daily for 30 days with an initial follow-up in the clinic scheduled for 1 week postoperatively. At the initial follow-up a hematoma, of lesser size than the original, at the same site of the HO was observed on physical examination. An attempt was made to aspirate the hematoma but failed. Two additional short-term follow-up appointments were conducted over the next 3 weeks. In the most recent follow-up, the patient reported a current pain level of zero out of ten and the post-surgical hematoma had resolved. The patient consented to his condition and clinical procedures being published.
While the link between prior trauma and HO has been well-established in the literature, considerations of the clinical impact of periarticular hip HO have largely only been significantly investigated in impingement cases secondary to hip arthroplasty and arthroscopy. Moreover, only a small body of case reports describe impingement symptoms in the setting of other hip operations (e.g., pelvic external fixator placement) or atraumatic injury involving the AIIS (e.g., AIIS avulsion fracture) [15, 16]. None have investigated the relationship between blunt trauma and the etiology of hip HO resulting in impingement symptoms. Traumatic HO of the hip is historically common following orthopedic procedures, and can be approached in three ways based on clinical evaluation; through conservative treatment, surgical intervention, or a combined approach [1, 9, 14]. HO of the magnitude recorded in this case can contribute to several associated sequelae. FAI syndrome is a related pathology to HO, and it is characterized by deformities of the bone creating compression in the hip joint. The connection between HO and FAI can be analyzed further by finding comorbidity rates among patients with HO of the AIIS region and FAI. This patient reported significant impairment in daily life due to the HO which prevented him from his normal level of activity and a change in gait. Certain risk factors can play a role from an onset due to trauma, that are determinants of probability of the HO formation [2]. In our case report, we saw a rapid transformation from soft mass to lamellar bone, despite the usage of NSAIDs, which indicated the associated hyperactivity of osteoinductive agents causative of HO [5, 6]. When discussing treatment, it is also important to identify preventative measures for HO occurring in the first place so that invasive surgical treatment is necessary only for limited and extraordinary cases. Gültekin et al. state that controlling inflammatory response early on in HO development is crucial to stopping its formation altogether, which would ultimately cease the onset of FAI if the correlation is proven [1, 10]. The causative connection points toward a positive correlation between the increasing class of HO and the presence of FAI. As far as first-line treatment for HO during its maturation, Hwang et al. state that although there are many studies on HO, much work is needed to develop targeted robust therapeutics to inhibit HO hypertrophy [18]. After observing the inability of conservative treatment to inhibit the maturation of HO, the outcomes of this case report should provide insight to physicians faced with a similar etiology in HO and FAI, utilizing both older literature regarding HO as a post-operative complication to hip procedures and newer literature with FAI as an increasingly prevalent diagnosis. Further investigation may yield more focus on the risk of HO as a potential complication following blunt hip trauma, with early identification a goal to allow for conservative treatment and avoid surgical intervention. We hope to prompt future research into showing the correlative nature of HO and FAI.
Although rarely reaching the size reported in this case, HO is common following trauma, as well as orthopedic procedures of the hip. MVAs serve as a trauma sufficient to induce HO. HO of this magnitude can severely impair the quality of life for patients, and countermeasures should be taken when trauma is sustained to the hip to prevent HO formation which can lead to further complications such as FAI. Although ultimately unsuccessful, we can reasonably presume that the failure of non-surgical treatment may have been due to especially large size of HO, and conservative measures should not be ruled out entirely when evaluating early-stage prognosis. We found that conservative measures, including NSAIDs and muscle relaxants, did not inhibit HO growth and surgical intervention had to be introduced. The gold standard treatment for Brooker’s class IV HO remains to be surgical excision of the mass. We recommend a further investigation into FAI as comorbidity following the development of HO of the hip.
With FAI as an increasingly prevalent diagnosis, we encourage further investigation into the causative relationship between HO of the hip and FAI syndrome. Given the current classification system, the Class IV HO presented in this case report serves to show an extreme case of HO leading to FAI, and the failure of conservative treatment with an eventual transition to surgical excision.
References
- 1.Gültekin MZ, Dinçel YM, Doğan AH, Ağca E. Massive heterotopic ossification after hip arthroscopy: A case report. Int J Orthop Sci 2022;8:551-4. [Google Scholar]
- 2.Ranganathan K, Loder S, Agarwal S, Wong VW, Forsberg J, Davis TA, et al. Heterotopic ossification: Basic-science principles and clinical correlates. J Bone Joint Surg Am 2015;97:1101-11. Erratum in: J Bone Joint Surg Am 2015;97:e59. [Google Scholar]
- 3.Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 1973;55:1629-32. [Google Scholar]
- 4.Rath E, Sherman H, Sampson TG, Ben Tov T, Maman E, Amar E. The incidence of heterotopic ossification in hip arthroscopy. Arthroscopy 2013;29:427-33. [Google Scholar]
- 5.Li L, Tuan RS. Mechanism of traumatic heterotopic ossification: In search of injury-induced osteogenic factors. J Cell Mol Med 2020;24:11046-55. [Google Scholar]
- 6.Medina A, Ma Z, Varkey M, Liu H, Iwashina T, Ding J, et al. Fibrocytes participate in the development of heterotopic ossification. J Burn Care Res 2015;36:394-404. [Google Scholar]
- 7.Cipriano CA, Pill SG, Keenan MA. Heterotopic ossification following traumatic brain injury and spinal cord injury. J Am Acad Orthop Surg 2009;17:689-97. [Google Scholar]
- 8.Medina A, Ma Z, Varkey M, Liu H, Iwashina T, Ding J, et al. Fibrocytes participate in the development of heterotopic ossification. J Burn Care Res 2015;36:394-404. [Google Scholar]
- 9.Łęgosz P, Otworowski M, Sibilska A, Starszak K, Kotrych D, Kwapisz A, et al. Heterotopic ossification: A challenging complication of total hip arthroplasty: Risk factors, diagnosis, prophylaxis, and treatment. Biomed Res Int 2019;2019:3860142. [Google Scholar]
- 10.Seegenschmiedt MH, Goldmann AR, Wölfel R, Hohmann D, Beck H, Sauer R. Prevention of heterotopic ossification (HO) after total hip replacement: Randomized high versus low dose radiotherapy. Radiother Oncol 1993;26:271-4. [Google Scholar]
- 11.Kemp J, Grimaldi A, Heerey J, Jones D, Scholes M, Lawrenson P, et al. Current trends in sport and exercise hip conditions: Intra-articular and extra-articular hip pain, with detailed focus on femoroacetabular impingement (FAI) syndrome. Best Pract Res Clin Rheumatol 2019;33:66-87. [Google Scholar]
- 12.Pennock AT, Bomar JD, Johnson KP, Randich K, Upasani VV. Nonoperative management of femoroacetabular impingement: A prospective study. Am J Sports Med 2018;46:3415-22. [Google Scholar]
- 13.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res 1999;363:93-9. [Google Scholar]
- 14.Lambrechts MJ, Gray AD, Hoernschemeyer DG, Gupta SK. Hip impingement after anterior inferior iliac spine avulsion fractures: A case report with review of the literature. Case Rep Orthop 2020;2020:8893062. [Google Scholar]
- 15.Sandilands SM, Raudenbush BL, Carreira DS, Cross BJ. Extra-articular hip impingement due to heterotopic ossification formation at the anterior inferior iliac spine following previous pelvic external fixation. BMJ Case Rep 2016;2016:bcr2015213610. [Google Scholar]
- 16.Hwang CD, Pagani CA, Nunez JH, Cherief M, Qin Q, Gomez-Salazar M, et al. Contemporary perspectives on heterotopic ossification. JCI Insight 2022;7:e158996. [Google Scholar]
- 17.Kemp J, Grimaldi A, Heerey J, Jones D, Scholes M, Lawrenson P, et al. Current trends in sport and exercise hip conditions: Intra-articular and extra-articular hip pain, with detailed focus on femoroacetabular impingement (FAI) syndrome. Best Pract Res Clin Rheumatol 2019;33:66-87. [Google Scholar]
- 18.Convente MR, Wang H, Pignolo RJ, Kaplan FS, Shore EM. The immunological contribution to heterotopic ossification disorders. Curr Osteoporos Rep 2015;13:116‐24. [Google Scholar]