A multidisciplinary strategy is crucial for the management of vascular abnormalities affecting the peripheral nervous system.
Dr. Aatam Vitrag Shah, Undergraduate Division, Surat Municipal Institute of Medical Education and Research, Surat, Gujarat, India. E-mail: shahaatam123@gmail.com
Introduction: Vascular anomalies, comprising up to 4.5% of the general population, are aberrations occurring during vascular development. Vascular abnormalities are frequently identified in children and frequently exhibit characteristics similar to nerve sheath tumors. We report a case of 16 years old boy with a arterio-venous malformation (AVM) affecting the brachial plexus. We discuss the clinical features, diagnosis, treatment, and histopathological findings in this patient and review the relevant literature.
Case Report: A 16-year-old boy presented with pain, paresthesia, swelling, and reduced grip strength of the hand. Radiological investigations revealed a vascular lesion encasing C5, C6 nerve roots and displacing the C7 root. Near total surgical excision of the lesion was done with preservation of nerve. Histopathology confirmed AVM with distinct features.
Conclusion: High-resolution ultrasound is crucial for diagnosing soft-tissue vascular anomalies. Surgeons well versed in micro surgical skill play a key role in minimizing neural deficits. In the case of vascular malformations of brachial plexus, near total excision is the most favorable option.
Keywords: Vascular anomalies, arterio-venous malformation, brachial plexus.
Vascular anomalies are aberrations that appear during vascular development, may involve any anatomical structure and have a prevalence of up to 4.5% in the general population. They are usually diagnosed in childhood [1]. Vascular anomalies involving the peripheral nervous system are rare, with only a few reports in the literature [2]. They typically present with features similar to a nerve sheath tumor such as pain, swelling, paresthesia, and occasionally weakness [3]. We report a 16-year-old boy that had an arterio-venous (AV) malformation encasing the upper roots of the left brachial plexus and discuss the clinical features, diagnosis, treatment, and review the relevant literature.
A 16-year-old boy presented with a 35 mm × 25 mm mass over the left supra clavicular region of three months duration. He gave no history of trauma before the onset of the masses. The mass was pea sized initially and had gradually progressed to the current size. The mass was painful, and the pain score was 5 on the visual analog scale [4]. The mass was not pulsatile, and thrill or bruit was absent There was no radiation of pain. The patient complained of tingling sensation over tips of all fingers and some loss of grip strength of left hand. Discriminative sensibility remained unaltered. On examination, a single, firm mass was palpable in the left supraclavicular fossa. The mass was tender and not adherent to the overlying skin. He had MRC grade 3 power of left wrist extension There was no tinel in relation to the mass and his brachial, radial, and ulnar pulses were well felt. The patient was advised an magnetic resonance imaging scan and ultrasound (US) Doppler scan to assess the tumor in greater detail, but declined due to financial constraints and only an US Doppler scan was done. A high-resolution ultra-sonography of the neck showed a well-defined, lobulated, and vascular lesion between anterior and middle scalene muscles. It was surrounding the C5 and C6 nerve roots about 10–15 mm after their exit from the neural foramen and displacing the C7 root (Fig. 1).

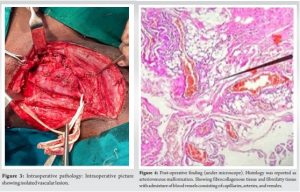
Based on the radiological investigations Gray-scale US combined with color Doppler flow imaging and spectral analysis most probable diagnosis for patient is vascular malformation with risk of future hemorrhage at site and loss of sensory and motor function of nearby nerves due to compression. The patient underwent exploration of the brachial plexus through a standard L-shaped incision in the posterior triangle (Fig. 2).

The phrenic nerve was identified and confirmed with a nerve stimulator. Subsequently, the C5, C6, and C7 nerve roots were identified, and the distal trunks and divisions identified, mobilized, and protected. The vascular tumor encasing the C5, C6, and C7 roots and the upper and middle trunk. All feeder vessels were ligated. Careful dissection of tumor from the involved nerves using the nerve stimulator as a guide was done (Fig. 3). For preservation of involved nerves and their function near total excision of tumor was performed and specimen sent for histology. In the post-operative period, the patient was asked for a strict follow-up to check for recurrence. The histology was reported as AVM and showed fibrocollagenous tissue and fibrofatty tissue with admixture of blood vessels consisting of capillaries, arteries, and venules. Vessels showed endothelial hyperplasia with collagenized thrombus dividing into coarse clumps along with presence of nerve bundles, areas of congestion, and hemorrhage (Fig. 4). At the 9-month follow-up, the patient exhibited asymptomatic status with no neurological deficits detected on examination.
In our case, based on patient’s complaint of decreased grip strength of left hand, it was suspected to be schwannoma of brachial plexus nerve roots. However, based on US findings it was suggestive of a vascular tumor involving C5, C6 roots, and displacing C7 roots. The decrease in grip strength might be due to compression of the lower nerve roots of the brachial plexus. In our patient, near total excision of tumor and ligation of all feeder vessels to prevent recurrence while preserving the underlying nerve roots was done. Histopathology confirmed the diagnosis of an AVM. The terminology for vascular lesions lacks clarity. Biologically, these lesions fall into two main categories: Hemangiomas and vascular malformations. Vascular malformations, such as AVMs, stem from vascular morphogenesis abnormalities, not neoplastic origins. It is crucial to recognize that AVMs, like other vascular malformations, result from developmental errors rather than being neoplastic [5, 6]. The clinical presentation of brachial plexus vascular malformations is contingent on the specific location, size of the swelling, the extent of involvement of the nerve roots, as well as the potential compression of adjacent structures. For radiological investigations, Gray-scale US combined with color Doppler flow imaging and spectral analysis serves as a valuable initial screening tool for patients with soft-tissue lesions suspected to be vascular in nature. It differentiates hemangiomas and vascular malformations with accuracy [7]. Histologically, AVMs are defined by thick-walled arteries and arterialized veins, demonstrating inherent potential for growth and recruitment of new blood vessels [8, 9]. In a specific instance where an iatrogenic AV fistula caused compression of the brachial plexus, notable observations included motor weakness and loss of tendon reflex, while the epicritic sensibility remained unaffected [10]. In a similar case, a brachial plexus venous hemangioma manifested as an enlargement of the soft-tissue mass without any motor or sensory symptoms. However, during the surgical procedure, intraoperative findings revealed hypervascularity and bleeding associated with the lesion [11]. In a retrospective examination of 24 patients who underwent Sclerotherapy for Vascular Malformation, it was observed that four patients encountered nerve palsy as an adverse event [12]. Furthermore, Ney et al. documented a case report detailing sciatic neuropathy following endovascular intervention for a limb vascular malformation [13]. Moreover, in a comprehensive study involving 573 patients undergoing embolo/sclerotherapy procedures, neuropathies manifested in 8.6% of cases [14]. Considering the potential risks outlined in these studies, we chose to avoid these procedures in our case to preserve the functionality of the brachial plexus. The comprehensive US approach plays a crucial role in efficiently distinguishing and classifying different types of soft-tissue vascular lesions [7]. The treatment modality depends on the extent, location, and nature of the mass, as well as the degree of brachial plexus trunk involvement. Near total excision of the tumor was the preferred choice of treatment in our case. Taking a biopsy first and then performing re-exploration was avoided in our case to minimize the chances of complications that lead to functional loss.
Soft-tissue high resolution US is essential for diagnosis. Careful nerve dissection by a surgeon well versed in micro surgical skill plays an important role in removal of tumor with no or minimal neural deficit. In the case of vascular malformations of brachial plexus, near total excision is the most favorable option. Histopathology findings are the final and important step in confirmation of diagnosis which also gives idea about chances of recurrence and time of recovery.
A comprehensive, multidisciplinary approach is essential for effectively managing distinctive cases, as demonstrated in the preceding discussion.
References
- 1.Greene AK. Vascular anomalies: Current overview of the field. Clin Plast Surg 2011;38:1-5. [Google Scholar]
- 2.Rusu GM, Ciuce C, Fodor L, Manole S, Dudea SM. Ultrasonographic and imaging appearance of peripheral intraneural vascular anomalies: Report of two cases and review of the literature. Med Ultrason 2018;20:237-46. [Google Scholar]
- 3.Donnelly LF, Adams DM, Bisset GS 3rd. Vascular malformations and hemangiomas: A practical approach in a multidisciplinary clinic. Am J Roentgenol 2000;174:597‐608. [Google Scholar]
- 4.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: A critical review. Psychol Med 1988;18:1007-19. [Google Scholar]
- 5.Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22. [Google Scholar]
- 6.North PE. Pediatric vascular tumors and malformations. Surg Pathol Clin 2010;3:455-94. [Google Scholar]
- 7.Paltiel HJ, Burrows PE, Kozakewich HP, Zurakowski D, Mulliken JB. Soft-tissue vascular anomalies: Utility of US for diagnosis. Radiology 2000;214:747-54. [Google Scholar]
- 8.Clemens RK, Pfammatter T, Meier TO, Alomari AI, Amann-Vesti BR. Vascular malformations revisited. Vasa 2015;44:5-22. [Google Scholar]
- 9.Uller W, Alomari AI, Richter GT. Arteriovenous malformations. Semin Pediatr Surg 2014;23:203-7. [Google Scholar]
- 10.Tebib JG, Bascoulergue J, Dumontet C, Paupert-Ravault A, Prallet B, Colson F, et al. Brachial plexus compression by an iatrogenic arteriovenous fistula. Clin Rheumatol 1987;6:593-6. [Google Scholar]
- 11.Abdolrazaghi H, Riyahi A, Zamenjany MR. Large venous hemangioma of brachial plexus. Ann Card Anaesth 2020;23:218-20. [Google Scholar]
- 12.Odeyinde SO, Kangesu L, Badran M. Sclerotherapy for vascular malformations: Complications and a review of techniques to avoid them. J Plast Reconstr Aesthet Surg 2013;66:215-23. [Google Scholar]
- 13.Ney JP, Shih W, Landau ME. Sciatic neuropathy following endovascular treatment of a limb vascular malformation. J Brachial Plex Peripher Nerve Inj 2006;1:8. [Google Scholar]
- 14.Lee KB, Kim DI, Oh SK, Do YS, Kim KH, Kim YW. Incidence of soft tissue injury and neuropathy after embolo/sclerotherapy for congenital vascular malformation. J Vasc Surg 2008;48:1286-91. [Google Scholar]










