Implementing a structured algorithm for managing vascular injuries during total knee replacement surgeries improves the surgical team's responsiveness, efficiency, and patient outcomes, while regular training and ongoing review enhance readiness and patient safety.
Dr. Sanjay Agarwala, Department of Orthopedics, P.D Hinduja Hospital and Medical Research Centre, Mumbai, Maharashtra, India. E-mail: drsa2011@gmail.com
Introduction: Vascular injury during total knee replacement (TKR) is a rare but potentially serious complication. Early recognition and prompt intervention are crucial for managing these injuries effectively. Interdisciplinary collaboration with a vascular surgeon is essential to optimize patient outcomes, minimizing the risk of limb loss and other long-term complications.
Case Report: We present a case of a 68-year-old woman with bilateral knee osteoarthritis who underwent bilateral TKR in a single surgical session with the right knee being the first knee. During left knee replacement, pulsatile bleeding was observed behind the femoral notch, following tourniquet deflation. Hemostasis was achieved and the procedure was completed. The patient’s oxygen saturation in the left lower limb decreased postoperatively. Computed tomography angiography revealed a 4.5 cm long thrombus in the popliteal artery at the knee joint level with adequate distal runoff. Digital subtraction angiography confirmed the blockage again with collateral vessel refilling. A decision was made to undertake an exploration to address the blockage, aiming to prevent further extension of the thrombus to the bifurcation of the popliteal artery. Surgical exploration revealed a laceration and thrombus in the popliteal artery, thrombectomy was done with Fogarty which was followed by end-to-end repair. The patient’s post-operative course was closely monitored. The patient went on to have a successful outcome and recovered well.
Conclusion: This case highlights the importance of early recognition, careful patient assessment, and immediate communication with an interventional radiologist and vascular surgeon in patients with suspected vascular injury during TKR. Interdisciplinary collaboration among orthopedic surgeons, interventional radiologists, and vascular surgeons is essential for optimizing patient outcomes in such cases.
Keywords: Vascular injury, total knee replacement, popliteal artery, thrombus, digital subtraction angiography.
Vascular injury during total knee replacement (TKR) surgery is a rare, but potentially serious, complication. It may occur due to surgical trauma, improper placement of instruments, or anatomical variations [1]. The reported incidence of this complication ranges from 17 to 230 cases per 100,000 [2]. Patients with pre-existing peripheral vascular disease, significant deformities, morbid obesity, renal failure, coagulopathy, and revision surgery are at higher risk of vascular injury during TKR [3-5]. Early recognition and prompt intervention are crucial in managing vascular injuries during TKR [6]. It is crucial to address this rare complication within 6 h, which is considered the “Golden window,” in critical limb ischemia following vascular injuries [7]. This case report highlights the importance of meticulous surgical techniques, careful patient assessment, and immediate communication with a vascular surgeon in cases of suspected vascular injury during TKR. It also emphasizes the significance of interdisciplinary collaboration in optimizing patient outcomes and minimizing the risk of limb loss and other long-term complications.
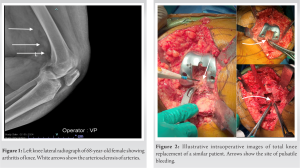
A 68-year-old woman with a body mass index of 37 kg/m2 presented with bilateral knee osteoarthritis and was admitted to our hospital for surgery. The patient had a history of hypertension and type 2 diabetes mellitus and had undergone percutaneous transluminal coronary angiography 6 years prior and on clopidogrel. Physical examination revealed a range of motion in both knees from 0° to 100° with pain. She had varus deformities of 12° on the right side and 20° on the left side. On close examination, her X-rays revealed arteriosclerosis of her arteries (Fig. 1).
Medical fitness was obtained and the patient was advised to discontinue clopidogrel 5 days before the planned surgery. Bilateral TKR in a single sitting proceeded as deemed appropriate for the patient’s overall condition [8]. The decision was made to perform bilateral knee replacement in a single surgical session under tourniquet control.
The right TKR was successfully completed. During left knee replacement, after making final cuts to the tibia and femur, pulsatile bleeding behind the femoral notch was noted following the deflation of the tourniquet (Fig. 2). Attempts were made using cautery but proved unsuccessful; therefore, pressure application using gauze and gel foam packs effectively achieved hemostasis. Distal pulsations were checked and found to be intact with no signs of ischemia. The final components were then implanted.
Immediately after surgery, the dorsalis pedis and posterior tibial arteries were palpable in both lower limbs, and the saturation in the pulse oximeter was 100% in both lower limbs. Thirty minutes later, the saturation in the left lower limb had decreased to 80%, so bedside color Doppler was performed, which showed sluggish blood flow in the distal vessels. One hour after surgery, computed tomography (CT) angiography was conducted (Fig. 3), and the results showed a 4.5 cm long thrombus in the popliteal artery at the knee joint level but good distal runoff, suggesting that the collaterals were functioning.
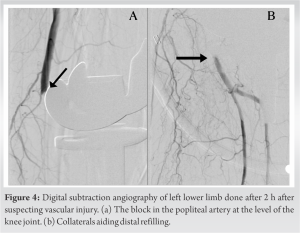
At this point, a vascular surgeon was consulted, and based on his advice, digital subtraction angiography (DSA) was planned. The patient and their relatives were kept informed about the situation, potential complications, and the necessary actions and interventions. DSA was performed within 2 h after surgery, revealing blockage of the popliteal artery and collateral vessels refilling the distal vessels (Fig. 4). The vascular surgery team recommended exploration and repair. This decision was made keeping in mind the possibility of local growth of the thrombus and chances of occlusion of the bifurcation of the artery to the posterior tibial and anterior tibial arteries.
During exploration through a medial approach to the knee, a laceration was discovered in the popliteal artery at the level of the middle genicular artery branch. The thrombus was removed using a Fogarty catheter (Fig. 5). The injured artery was then resected and repaired end-to-end (Fig. 6). After the surgery, the left lower limb was kept in a position of 10–20° of flexion, and mobilization was delayed for a 5 days. The patient’s post-operative course was closely monitored with regular assessments of distal pulses, oxygen saturation, and color Doppler imaging. The patient achieved a positive outcome with both incisions healing successfully (Fig. 7). By the end of 3 weeks, the patient had regained full range of motion and was able to walk comfortably without support or pain.
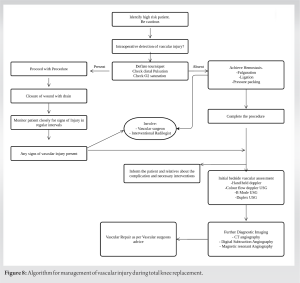
Iatrogenic vascular injury during TKR is rare, with only a few cases per 100,000. The rarity of this complication contributes to the minimal exposure of orthopedic surgeons to vascular injury after TKR, which may lead to delayed diagnosis and intervention. If not addressed in time, it can lead to serious sequelae. Mortality and amputation rates for such injuries are 7% and 42%, respectively [3, 7]. A standard checklist in such situations helps to minimize the consequences of vascular injury. The algorithm for managing vascular injury during TKR helps swiftly respond to this complication and avoid further consequences (Fig. 8). During knee arthroplasty, the popliteal artery can be injured, either directly or indirectly. Direct surgical injury during TKA may lead to bleeding, pseudoaneurysm formation, and/or arteriovenous fistula [9]. Indirect injury may result from the compression or blockage of the artery by retractors, tourniquets, or misplaced screws. It is essential to have a high index of suspicion and rapid response to any potential vascular issues during knee surgery. When dealing with high-risk patients with vascular injury, it is crucial to remain vigilant. If vascular injury is discovered intraoperatively under a tourniquet, the tourniquet should be deflated immediately. A check for distal pulsation and oxygen saturation is performed using pulse oximetry. If the procedure is ongoing, bleeding is controlled by ligation, cautery, or pressure packing. Complete the implantation and cementing before proceeding with further evaluation. Employ non-invasive tools such as handheld Doppler, color flow Doppler ultrasound, B-mode ultrasound, and duplex ultrasound were to assess the situation. At this stage, it is essential to involve an interventional radiologist and vascular surgeon. Keep the patient and family informed about the complications and the necessary interventions. Utilize radiological evaluation procedures such as CT angiography, digital subtraction angiography, and magnetic resonance angiography to further establish the diagnosis. Based on these findings, determine the appropriate intervention, which may include surgical repair, endovascular procedures such as thrombectomy or stent placement, or a combination of both [9, 10]. Post-operative monitoring of distal pulses, oxygen saturation, and color Doppler imaging is necessary. Implementation of immobilization and delayed mobility protocols allow for optimal healing and recovery [11]. Collaboration between orthopedic and vascular surgery teams is crucial in managing vascular injury during TKR to ensure timely intervention, minimize morbidity and mortality, and optimize patient outcomes [10, 12, 13].
The management of vascular injury during TKR requires prompt recognition, collaboration with a vascular surgeon, imaging assessment, informed consent, exploration and repair of the injured artery, diligent post-operative monitoring, and a multidisciplinary approach involving both orthopedic and vascular surgery teams. These checkpoints help ensure early intervention and minimize the risk of complications associated with vascular injury during TKR. This illustrative case demonstrates, how acting on this algorithm promptly, such a situation was successfully salvaged with excellent results.
Implementing an algorithm for managing vascular injuries during TKR surgeries improves the surgical team’s responsiveness and efficiency. This proactive approach enables the team to promptly identify and address vascular injuries, thereby reducing the risk of complications such as excessive blood loss and prolonged ischemia. By utilizing a structured algorithm, the team can ensure better patient outcomes and faster recovery times. Furthermore, regular training and simulations based on the algorithm improve the team’s readiness and confidence, while ongoing review and enhancement of the algorithm contribute to overall surgical practice and patient safety.
References
- 1.Karam JA, Bloomfield MR, Dilorio TM, Irizarry AM, Sharkey PF. Evaluation of the efficacy and safety of tranexamic acid for reducing blood loss in bilateral total knee arthroplasty. J Arthroplasty 2014;29:501-3. [Google Scholar]
- 2.Sundaram K, Udo-Inyang I, Mont MA, Molloy R, Higuera-Rueda C, Piuzzi NS. Vascular injuries in total knee arthroplasty: A systematic review and meta-analysis. JBJS Rev 2020;8:e0051. [Google Scholar]
- 3.Bernhoff K, Rudström H, Gedeborg R, Björck M. Popliteal artery injury during knee replacement: A population-based nationwide study. Bone Joint J 2013;95-B:1645-9. [Google Scholar]
- 4.Ko LJ, DeHart ML, Yoo JU, Huff TW. Popliteal artery injury associated with total knee arthroplasty: Trends, costs and risk factors. J Arthroplasty 2014;29:1181-4. [Google Scholar]
- 5.Parvizi J, Pulido L, Slenker N, Macgibeny M, Purtill JJ, Rothman RH. Vascular injuries after total joint arthroplasty. J Arthroplasty 2008;23:1115-21. [Google Scholar]
- 6.Kolosky M, Spindler KP. A national collegiate athletic association division I athlete’s return to play after traumatic knee dislocation with vascular and nerve injury. J Am Acad Orthop Surg Glob Res Rev 2018;2:e073. [Google Scholar]
- 7.Kumar SN, Chapman JA, Rawlins I. Vascular injuries in total knee arthroplasty: A review of the problem with special reference to the possible effects of the tourniquet. J Arthroplasty 1998;13:211-6. [Google Scholar]
- 8.Agarwala S, Menon A. Safety and efficacy of sequential simultaneous bilateral total knee arthroplasty: A single centre retrospective cohort study. J Clin Orthop Trauma 2020;11:S636-44. [Google Scholar]
- 9.Mathew A, Abraham BJ, Fischer L, Punnoose E. Popliteal artery thrombosis following total knee arthroplasty managed successfully with percutaneous intervention. BMJ Case Rep 2014;2014:bcr2014206936. [Google Scholar]
- 10.Hulse N, Naik P, Dilip N, Nagabhushan KN, Bhat AK. Vascular injuries associated with total knee arthroplasty. Int J Res Orthop 2022;8:722-7. [Google Scholar]
- 11.Kurtoglu T, Durmaz S, Dişçigil B. Endovascular and surgical treatment of acute deep vein thrombosis. Meandros Med Dent J 2020;21:1-11. [Google Scholar]
- 12.Shrikhande GV, McKinsey JF. Use and abuse of atherectomy: Where should it be used? Semin Vasc Surg 2008;21:204-9. [Google Scholar]
- 13.Gosslau Y, Warm TD, Foerch S, Zerwes S, Scheurig-Muenkler C, Hyhlik-Duerr A. Iatrogenic injury of the popliteal artery in orthopedic knee surgery: Clinical results and development of a therapeutic algorithm. Eur J Trauma Emerg Surg 2022;48:4169-79. [Google Scholar]