Coracoid osteotomy, greater tuberosity takedown and latarjet procedure, combined with early physiotherapy and mobilization appear to achieve good functional results in the short to medium term for operative intervention in chronic bilateral locked anterior shoulder dislocations in the short to medium term.
Dr. Neil Jones, Department of Orthopaedic, East Surrey Hospital, Canada Avenue, Redhill, RH1 5RH, United Kingdom. E-mail: neil.jones11@nhs.net
Introduction: It is rare to see chronic bilateral anterior fracture-dislocations as a result of seizure, and we present a case of this type and review of the literature. Despite the signs and symptoms of shoulder dislocation being well documented, and X-ray imaging being good at identifying such pathology, there are a few cases in the literature of missed or chronic shoulder dislocation (a shoulder that has been dislocated for more than 3 weeks) but these are extremely rare. Our case represents the first example of chronic bilateral locked anterior fracture-dislocations requiring open reduction and coracoid osteotomy with GT takedown to gain adequate exposure and allow soft tissue release to facilitate joint reduction. No other case has used anchors to achieve GT fixation, and our patient is the youngest published case with such pathology.
Case Report: A 16-year-old boy presented to the emergency department with reduced range of movements in both shoulders. Six weeks prior he had suffered an epileptic seizure. X-rays confirmed bilateral anterior shoulder dislocations with displaced greater tuberosity (GT) fractures. Staged open reduction was performed in the right and then left shoulder. Coracoid osteotomy with takedown of the malunited GT fracture was needed to assist with gradual soft tissue contracture release and a successful relocation. Latarjet procedure was then performed and the GTs were fixed using rotator cuff anchors. At 6 months post-operation, on the right side, he achieved forward flexion to 150o and abduction to 120o. On the left side, forward flexion was 110o and abduction was 90o. X rays showed satisfactory maintenance of the reduction without signs of avascular necrosis of the humeral head.
Conclusions: Surgical management of this injury in this way is effective and achieves good results in the first 6 months of follow up. A high index of suspicion should be employed for this injury in post-ictal patients with shoulder pain. Early mobilization and effective physiotherapy is essential post-operatively to achieve good short-term range of motion.
Keyword: Shoulder dislocation, chronic, bilateral surgery.
Although anterior glenohumeral dislocations are the most common joint dislocation in UK Emergency Departments [1,2], they are uncommon to see bilaterally [3]. Usually, they are unilateral and seen as a result of trauma in men aged 16–20 [4]. Bilateral anterior glenohumeral dislocations are also usually due to trauma and it is rare to see a case caused by seizure activity as posterior dislocations are much more common [5]. Despite the signs and symptoms of shoulder dislocation being well documented, and X-ray imaging being good at identifying such pathology, there are a few cases in the literature of “missed” or “chronic” shoulder dislocation (a shoulder that has been dislocated for more than 3 weeks) but these are extremely rare [6,7,8].
Joints that have been dislocated for longer than 3 weeks have specific and significant complications associated with them. Old unreduced shoulder dislocations are difficult to reduce by closed methods because of soft tissue contractures, fibrous tissue in the glenoid cavity, retracted rotator cuff muscles, the risk of causing iatrogenic fractures, and the risk of iatrogenic neurovascular damage. They, therefore, need careful consideration, normally requiring open reduction and assessment of any concurrent fractures for surgical intervention.
The authors present a case of chronic, locked bilateral anterior dislocation in a young patient following seizure. Written informed consent has been obtained from the patient to publish his case electronically and in article.
AK, a seventeen-year-old male presented to East Surrey Hospital Emergency Department on 14th May, 2020 with reduced range of movements in both shoulder joints. Five and a half weeks prior to presentation, on 6th April 2020, he had suffered an epileptic seizure sitting in an office chair, falling off the chair with both arms stuck in the spaces under each arm rest. At this time a paramedic crew attended to him and he was reassured at the scene. The next day, AK’s mother called for Paramedic assistance once more on account of his painful shoulders, and another Ambulance crew examined and reassured the patient.
AK experienced swelling and bruising in both shoulders in the days that followed the seizure, together with pain and reduced range of movement. AK attended a virtual GP appointment with regards to his poor shoulder function. The consultation was virtual due to the ongoing COVID-19 pandemic, and he was reassured by the GP and no further action was taken.
Pain and stiffness in both shoulder joints further continued, and 5 weeks post-seizure AK presented to Hospital, was examined, and found to have bilateral “squared” appearance of both shoulders. Efforts by ED doctors to reduce the joints were unsuccessful with entonox, and the Trauma and Orthopaedic (T+O) team were called. On examination by the T+O on- doctor, AK was unable to flex or abduct each arm higher than 90. AK could internally rotate both shoulders but was unable to externally rotate either shoulder. Sensation in both axillary nerve regions was normal. Plain film X-ray imaging confirmed bilateral anterior shoulder dislocations and bilateral greater tuberosity fractures (Fig. 1).
AK’s case was discussed by the on-call team and consultant and plans made for urgent review at the upper limb clinic that week on the May 19, 2020. AK’s significant medical history included only epilepsy, for which he had been reducing his dosage of sodium valproate from January 2020 and the seizure on the April 6, 2020, was the first he had suffered whilst reducing the medication. After the seizure in April, AK had restarted his anti-epileptic medication and had had no further episodes.
AK was reviewed in the upper limb clinic and CT scan imaging confirmed the diagnosis as it appeared on plain films (Fig. 2 and 3). It was decided that he could be offered surgical management.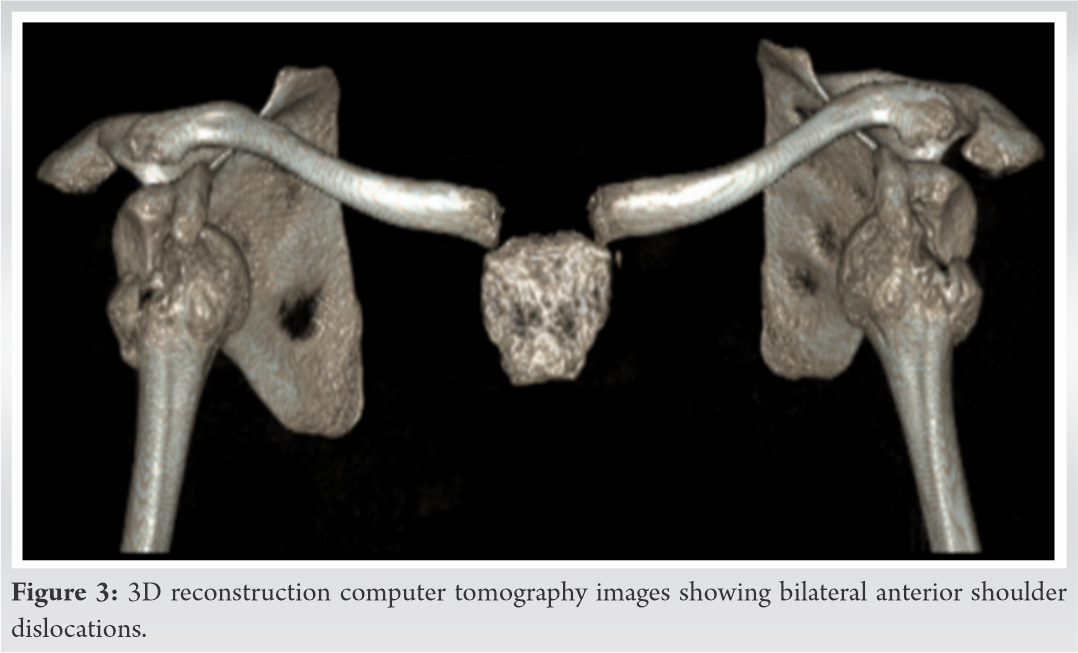
He underwent a successful open reduction and stabilisation with Latarjet procedure of the right humerus on May 28, 2020 (7 weeks post-injury) and the same procedure was performed on the left humerus on June 4, 2020 (8 weeks post-injury).
Intraoperatively for both shoulders, the deltopectoral approach was performed, and the greater tuberosity fracture was released (taken down) to gain access. Coracoid osteotomy followed this, and significant contracture around the anterior glenoid cavity was released. Good access to the humeral head was thus achieved, and we were able to visualise posterior to the head and visualise the subscapularis and medial glenohumeral ligaments. Having relocated the displaced humeral heads, the Latarjet procedure was performed.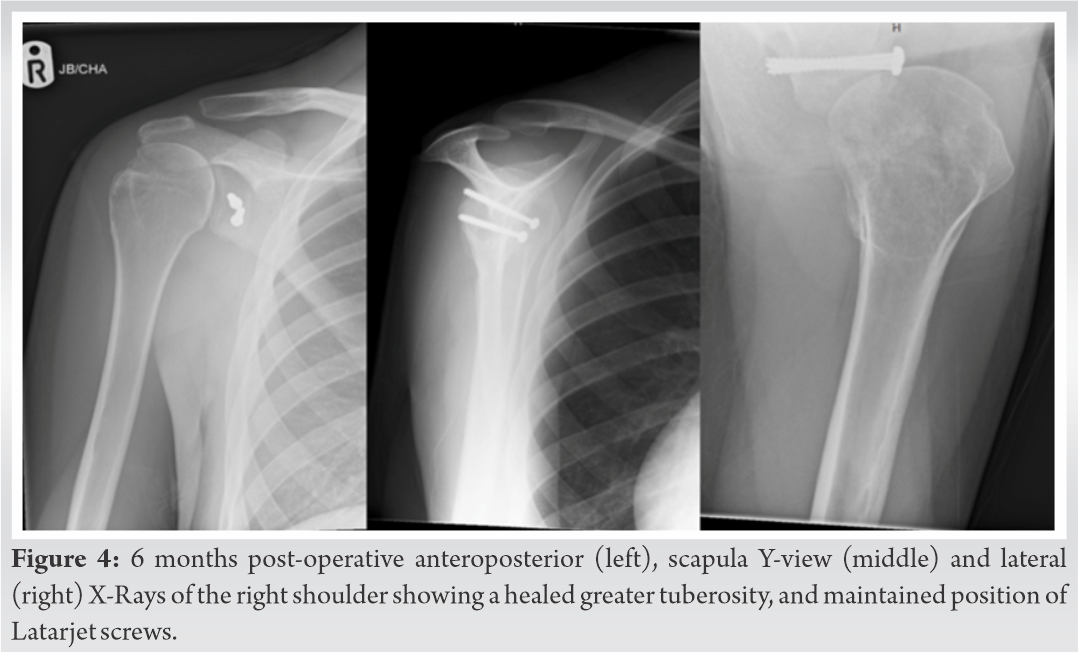
The greater tuberosity fractures were then repaired using rotator cuff anchors in a double row configuration.
Post-operative plan stipulated to remain in a polysling for 2 weeks and to begin passive range of motion of the elbow for 4 weeks before beginning active motion exercises with our Physiotherapists for 6 weeks.
AK was followed up 5 days after the left shoulder procedure for removal of his right shoulder wound clips and bilateral post-operative X-Rays – which both showed both shoulders as being in joint. He remained neurovascularly intact and he was encouraged to start forward bending to assist with indirect mobilisation of the shoulder as well as other exercises to do while waiting for the Letarjet to heal.
He was seen at 3 weeks post-operation where his shoulders were noted to be expectedly stiff, X-rays were satisfactory and he was once again encouraged to engage well with physiotherapy. At 6 weeks post-operation he remained neurovascularly intact, wounds had healed, and he had started range of motion exercises. His sling was discarded and he was reminded of the importance of physiotherapy for his range of motion to improve. At 3 months post-operation he was able to forward flex and abduct bilaterally to 60o. Bilaterally external rotation was achievable to 10o and internal rotation achievable to the buttock. He remained well in himself, and X rays taken were satisfactory.
Six months post-operatively pleasingly saw further improvement in range of motion. On the right side, forward flexion achieved 150o and abduction to 120o On the left side, forward flexion achieved 100o and abduction to 90 degrees. Both shoulders at this stage could externally rotate to 30o and internally rotate to the mid lumbar spine region. Check X rays showed satisfactory maintenance of the reduction and good healing of the latarjet (Fig. 4 and 5). Post-operative range of motion assessments at 3 and 6 months can be seen in Table 1.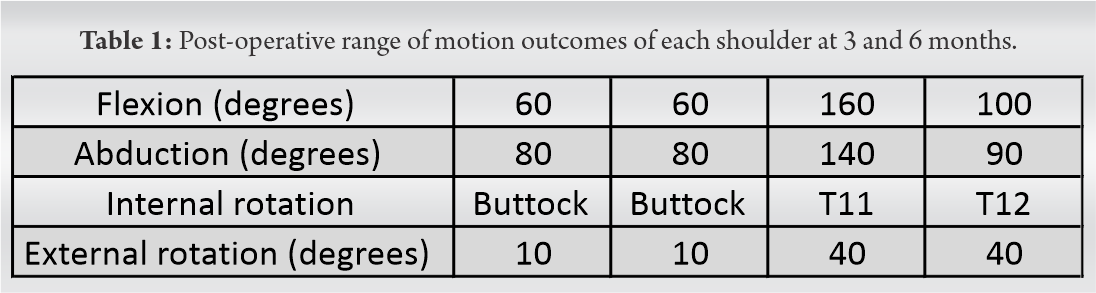
Our case represents the first example of chronic bilateral locked anterior fracture-dislocations requiring open reduction and coracoid osteotomy with GT takedown to gain adequate exposure and allow soft tissue release to facilitate joint reduction. No other case has used anchors to achieve GT fixation, and our patient is the youngest published case with such pathology.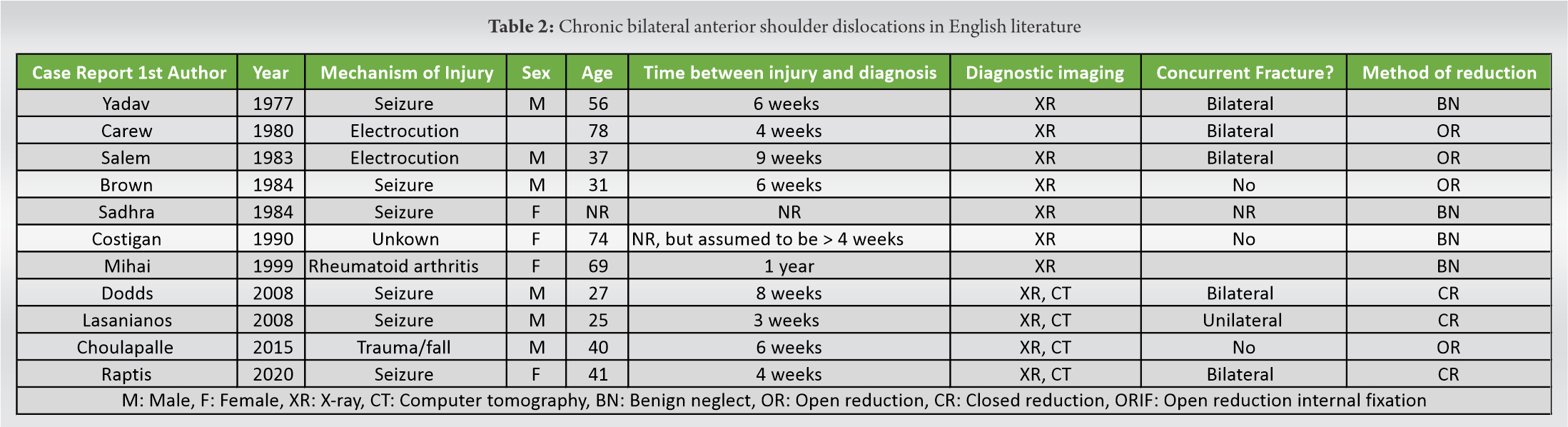
On review of the literature published in the English language there are eleven previous reports of chronic bilateral anterior glenohumeral dislocation (Table 2). Of these eleven, four were treated non-operatively [9,10,11,12] and no closed reduction was attempted, four were treated with open reduction alone [13,14,15,16], two were treated with successful closed reduction and ORIF of the concurrent greater tuberosity fractures [17,18] and one was treated by closed reduction alone [19].
In contrast to the usual aetiology of shoulder dislocations, the most common cause of chronic bilateral anterior glenohumeral dislocation published is seizure which is reported in seven of the eleven cases. Two articles reported the dislocations as a result of electrocution, one as a result of rheumatoid glenoid destruction, and one as a result of trauma.
Six studies reported chronic bilateral anterior glenohumeral dislocations in patients that had suffered a seizure, the first of these being the paper by Yadav et al. in 1977 [9]. With no interventions made, they recorded a function of 70º abduction for both limbs after 6 months. This is the first paper published describing this chronic dislocation pattern, and therefore represents a baseline for what outcomes can be expected should this rare condition be left untreated. Thus, this case demonstrates how much better outcomes can be in these patients, should surgical management in the way described is carried out, particularly in younger patients.
Surgical management of this injury in this way is effective and achieves good results in the first 6 months of follow-up. We will continue to follow-up this patient to assess more long term function.
It is important that we as clinicians are aware of the possibility of missing this diagnosis, and a high index of suspicion should be employed for this injury in post-ictal patients with shoulder pain.
Early mobilization and effective physiotherapy is essential post-operatively to achieve good short term range of motion despite a significant injury and surgical procedure.
Have a high index of suspicion for shoulder dislocation in post-ictal patients with shoulder pain. Latarjet procedure for this injury can achieve good post-operative results when combined with early mobilization and good post-operative exercises.
References
- 1.Kroner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg 1989;108:288-90. [Google Scholar | PubMed]
- 2.Cutts S, Prempeh M, Drew S. Anterior shoulder dislocation. Ann R Coll Surg Engl 2009;91:2-7. [Google Scholar | PubMed]
- 3.Pushpakumara J, Sivathiran S, Roshan L, Gunatilake S. Bilateral posterior fracture-dislocation of the shoulders following epileptic seizures: A case report and review of the literature. BMC Res Notes 2015;8:704. [Google Scholar | PubMed]
- 4.Shah A, Judge A, Delmestri A, Edwards K, Arden NK, Prieto-Alhambra D, et al. Incidence of shoulder dislocations in the UK, 1995-2015: A population-based cohort study. BMJ Open 2017;7:e016112. [Google Scholar | PubMed]
- 5.Kumar YC, Nalini KB, Maini L, Nagaraj P. Bilateral traumatic anterior dislocation of shoulder-a rare entity. J Orthop Case Rep 2013;3:23-5. [Google Scholar | PubMed]
- 6.Rowe CR, Zarins B. Chronic unreduced dislocations of the shoulder. J Bone Joint Surg Am 1982;64:494-505. [Google Scholar | PubMed]
- 7.Pritchett JW, Clark JM. Prosthetic replacement for chronic unreduced dislocations of the shoulder. Clin Orthop Relat Res 1987;216:89-93. [Google Scholar | PubMed]
- 8.Babalola OR, Vrgoc G, Idowu O, Sindik J, Coklo M, Marinovic M, et al. Chronic unreduced shoulder dislocations: Experience in a developing country trauma centre. Injury 2015;46 Suppl 6:S100-2. [Google Scholar | PubMed]
- 9.Yadav SS. Bilateral simultaneous fracture-dislocation of the shoulder due to muscular violence. J Postgrad Med 1977;23:137-9. [Google Scholar | PubMed]
- 10.Sadhra K. Unusual dislocations associated with epileptic fits. Br Med J (Clin Res Ed) 1984;288:681-2. [Google Scholar | PubMed]
- 11.Costigan PS, Binns MS, Wallace WA. Undiagnosed bilateral anterior dislocation of the shoulder. Injury 1990;21:409. [Google Scholar | PubMed]
- 12.Mihai R, Dixon JH. Bilateral atraumatic dislocation of the shoulder. J Accid Emerg Med 1999;16:460. [Google Scholar | PubMed]
- 13.Carew-McColl M. Bilateral shoulder dislocations caused by electric shock. Br J Clin Pract 1980;34:251-4. [Google Scholar | PubMed]
- 14.Salem MI. Bilateral anterior fracture-dislocation of the shoulder joints due to severe electric shock. Injury 1983;14:361-3. [Google Scholar | PubMed]
- 15.Brown RJ. Bilateral dislocation of the shoulders. Injury 1984;15:267-73. [Google Scholar | PubMed]
- 16.Choulapalle R, Chokkarapu R, Kolluri RK, Anne SR, Perumal SR, Avadhanam PK, et al. A case of neglected bilateral anterior shoulder dislocation: A rare entity with unusual mechanism of injury. Case Rep Orthop 2015;2015:461910. [Google Scholar | PubMed]
- 17.Dodds SD, Medvecky MJ. Chronic bilateral locked anterior shoulder fracture-dislocations. Am J Orthop (Belle Mead NJ) 2008;37:364-8. [Google Scholar | PubMed]
- 18.Lasanianos N, Mouzopoulos G. An undiagnosed bilateral anterior shoulder dislocation after a seizure: A case report. Cases J 2008;1:342. [Google Scholar | PubMed]
- 19.Raptis K, Koutserimpas C, Alpantaki K, Kaiafas S, Fandridis E, Bourlos D. Neglected bilateral anterior shoulder dislocation following epileptic seizure: A case report and literature review. Kurume Med J 2020;66:65-70. [Google Scholar | PubMed]