Internal mineralization within the joint, significant soft tissue proliferation, and erosive change should raise suspicion of synovial osteochondromatosis.
Dr. Cleofina Furtado, Department of Diagnostic and Interventional Radiology, University Hospitals of North Midlands NHS Trust, Stoke on Trent, ST4 6QG, United Kingdom. E-mail: cleofinafurtado@gmail.com
Introduction: Chondrosarcoma of the synovium is a rare and malignant form of cartilaginous tumor that originates in synovial tissue. There have only been a limited number of reported cases of malignant transformation of synovial chondromatosis (SC) into secondary chondrosarcoma (SCH), primarily in the hip and knee, in patients with resistant illness. The occurrence of chondrosarcoma in SC of the wrist is highly uncommon, as evidenced by only a single previous case study that has been documented in the literature.
Case Report: This study presents a case series of two patients with primary SC who developed SCH at the wrist joint.
Conclusion: Clinicians treating localized swellings of the hand and wrist should be alert to the likelihood of a sarcoma diagnosis to minimize delays to definitive therapy.
Keywords: Secondary chondrosarcoma, synovitis, primary synovial chrondromatosis, secondary synovial chondromatosis, malignant transformation.
The differential diagnosis for a palpable wrist swelling is extensive and encompasses various conditions, including tendon injury and inflammation, inflammatory arthritis, osteoarthritis, mal-union of a fractured distal radius, metabolic bone disease, and both benign and malignant soft tissue and bone tumors [1]. Physical examination alone may not be sufficient to distinguish between these diagnoses, and additional imaging may be necessary to make an accurate determination [2]. Primary synovial chondromatosis (PSC) is a relatively uncommon benign condition characterized by the proliferation of cartilage within the synovial membrane due to subsynovial connective tissue metaplasia. This results in the formation of intra-articular loose bodies, although the exact cause of the condition is unknown [2]. Patients with PSC may experience symptoms such as pain, swelling, and mechanical complaints [3,4]. The diagnosis of PSC should be considered when evaluating a mono-articular intra-articular soft tissue mass, especially if there is evidence of superficial bone erosion and mineralization on radiography [3]. However, it is important to note that calcification may not be visible in the early stages, and nodules may not be discernible [5]. Magnetic resonance imaging (MRI) can help to identify a non-calcified mass, including chondromas or osteochondromas, as well as their relationship with extra-articular structures [6]. The transformation of PSC into secondary chondrosarcoma (SCH) is a rare event. While most reported cases describe malignant transformation in the presence of pre-existing PSC, there have also been a few cases of primary chondrosarcoma documented in the literature [7,8]. On average, malignant transformation occurs 11.2 years after diagnosis, with the knee being the most commonly affected joint (47.7%), followed by the hip (34.3%) and ankle (5.9%) [9]. SCH is extremely uncommon in the elbow and temporomandibular joints, with only a single case reported in the wrist joint [4]. Distinguishing between benign SC and malignant entities may prove challenging through radiology alone. There are no definitive imaging characteristics that differentiate SCH from PSC, which presents a significant diagnostic challenge [3]. Furthermore, the progression of SCH is often focal and its typical histological features may be overlooked with inadequate tissue sampling. There is also overlap in the cytoarchitectural features of PSC and SCH [10]. As a result, a comprehensive evaluation based on a combination of clinical, radiological, and histological findings is necessary for an accurate diagnosis [2,8].
Case 1
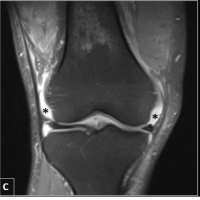
A 78-year-old right-handed male patient presented with a 7-year history of soft-tissue swelling on his right wrist, with a recent progression in size, new neurological symptoms, and functional impairment. He was under the care of the clinical rheumatology team for known bilateral wrist arthritis. Over the years, he had had frequent flare-ups in both his wrists with temporary pain relief provided by oral analgesics and steroid injections. Multiple X-rays of both wrists over the previous years demonstrated bilateral arthritis involving the radiocarpal, distal radio-ulnar, scapho-trapezium-trapezoid, carpo-metacarpal, and metacarpophalangeal joints (MCPJ) more advanced at the second and third MCPJ. The main features were narrowed joint spaces, associated with large subarticular cysts and chondrocalcinosis at the site of triangular fibrocartilage (TFC) disc. These findings were considered as features of crystal arthropathy disease. However, aspiration under US guided was negative for crystals. There was a recent history of neurological symptoms in the hand, that is, tingling and numbness involving median nerve distribution, with a soft-tissue swelling now interfering with his daily living activities associated with significant neurological and functional compromise whereby he was then referred to the orthopedic surgeon. Clinical examination revealed a loss of function at the wrist joint and firm nodular lumps on the radial aspect of the right wrist and the TFC complex. The squeeze test was negative with mild tenderness in the right second MCPJ, but there was no warmth or redness. Up-to-date, plain X-rays demonstrated progressively enlarging periarticular soft-tissue swelling with internal mineralization at the right wrist with larger bone erosions as compared to previous X-rays. A subsequent MRI demonstrated profuse synovial proliferation into large peri-articular soft tissue or synovial masses. The long clinical history and bilateral polyarthopathy with involvement of MCP joints, periarticular soft-tissue mineralization and mild hyperuricaemia on his blood investigations raised the possibility of erosive crystal deposition arthropathy like uncontrolled tophaceous gout. Given the symptoms and significant functional compromise, a decision was made after orthopedic review and discussion at the local soft-tissue tumor meeting to decompress the median nerve, debulk the suspected gouty tophus around the right wrist joint, and take biopsies. During the surgery, however, it was noted that the mass was that of cartilaginous tissue arising from the joint itself. An excision biopsy was done during the surgery where histology confirmed SCH arising on a background of PSC. Following consultation with the patient and given the fact that SCH is not normally radiosensitive, a decision was made to perform a below-elbow amputation.
Case 2
A 67-year-old female patient presented to the musculoskeletal clinic with complaints of pain in the volar aspect of her right wrist. She had an X-ray which did not reveal anything untoward. She was referred for MRI since the pain failed to settle and this demonstrated a fluid-filled structure on the volar surface of the wrist related to radio-scaphoid articulation which was reported to be a ganglion (Fig. 7). Nine months later, she was referred for ultrasound-guided aspiration of her ganglion cyst since she had no benefit from the oral analgesics. The ultrasound however demonstrated a solid lobular lesion on the volar-radial aspect of the wrist, displacing the flexor tendons and showing no evidence of internal vascularity (Fig. 8). Suspicion of malignancy was raised due to its morphology and the significant increase in size since the previous MRI. Subsequent MRI demonstrated a deeply seated lobulated soft-tissue lesion, at the volar/radial side of the wrist extending between the first extensor tendons laterally and the carpal tunnel medially (Fig. 9). It was associated with deeper enhancing soft tissues along the volar surfaces of the scaphoid, lunate, and distal radius with small punched-out erosions of the lunate. The lesion was invaginating itself around the flexor carpi radialis tendon and creeping medially to displace the flexor tendons and the median nerve. There was also mild-to-moderate peri-ulnar synovial thickening and extensor digitorum tenosynovitis. Given the morphology and signal which was unusual for a simple ganglion or inflammatory synovitis, she went on to have an excision biopsy where histology confirmed PSC.
PSC is a benign disorder characterized by the growth of cartilage within the synovial membrane, resulting from metaplasia of the subsynovial connective tissue. Its exact cause is unknown [2]. PSC can cause damage to the joint and result in osteoarthritis as the cartilaginous chondromas can detach from the synovium and become free-floating within the joint [11].  This condition is typically seen in a single joint, most commonly in the knee, but it can also occur in other joints such as the hip, elbow, shoulder, ankle, wrist, and temporomandibular joint [4,5]. Secondary SC (SSC) is a similar condition, but it arises as a result of other joint-related issues such as trauma, osteoarthritis, or neuropathic arthropathy. If a patient presents with a single joint intra-articular soft-tissue mass, it is important to consider the possibility of PSC or SSC, particularly if radiographic evidence of superficial bone erosion and periarticular soft-tissue mineralization is present [3]. Compared to SSC, PSC has a greater propensity for malignant development into SCH [8,9].
This condition is typically seen in a single joint, most commonly in the knee, but it can also occur in other joints such as the hip, elbow, shoulder, ankle, wrist, and temporomandibular joint [4,5]. Secondary SC (SSC) is a similar condition, but it arises as a result of other joint-related issues such as trauma, osteoarthritis, or neuropathic arthropathy. If a patient presents with a single joint intra-articular soft-tissue mass, it is important to consider the possibility of PSC or SSC, particularly if radiographic evidence of superficial bone erosion and periarticular soft-tissue mineralization is present [3]. Compared to SSC, PSC has a greater propensity for malignant development into SCH [8,9]. 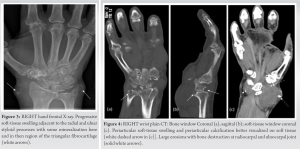 Orthopedic surgeons, radiologists, and pathologists find it challenging differentiating PSC from SCH [3,8]. The diagnosis of SCH can often prove to be a challenge as the clinical and radiological manifestations of this condition are often similar to those of severe PSC [12]. In most cases, it is challenging to diagnose SCH since the clinical and radiological signs of this malignancy are extremely similar to those of severe PSC [12].
Orthopedic surgeons, radiologists, and pathologists find it challenging differentiating PSC from SCH [3,8]. The diagnosis of SCH can often prove to be a challenge as the clinical and radiological manifestations of this condition are often similar to those of severe PSC [12]. In most cases, it is challenging to diagnose SCH since the clinical and radiological signs of this malignancy are extremely similar to those of severe PSC [12].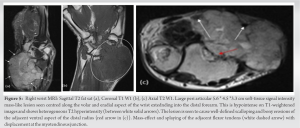 This along with other potential wrist joint pathologies with shared characteristics adds further to the confusion [1]. The two pathologies are treated and prognosed differently. Hence, efforts have been undertaken to uncover clinical, imaging, and histological characteristics that could help distinguish the two entities [9,10].
This along with other potential wrist joint pathologies with shared characteristics adds further to the confusion [1]. The two pathologies are treated and prognosed differently. Hence, efforts have been undertaken to uncover clinical, imaging, and histological characteristics that could help distinguish the two entities [9,10]. 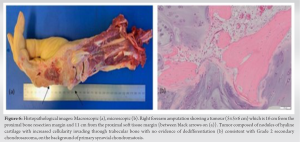 Clinically, both PSC and SCH can have a similar presentation. Many authors believe that sudden rapid deterioration in symptoms or increase in periarticular soft-tissue volume on the background of a long-standing symptoms, multiple relapses, and rapid recurrence following synovectomy may all the clinical signs of malignant transformation [9,11]. In patients presenting with a palpable localized mass in the wrist, ultrasonography is typically the first choice of imaging modality [11].
Clinically, both PSC and SCH can have a similar presentation. Many authors believe that sudden rapid deterioration in symptoms or increase in periarticular soft-tissue volume on the background of a long-standing symptoms, multiple relapses, and rapid recurrence following synovectomy may all the clinical signs of malignant transformation [9,11]. In patients presenting with a palpable localized mass in the wrist, ultrasonography is typically the first choice of imaging modality [11].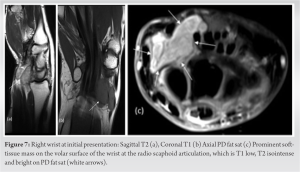 The ultrasound findings for both PSC and SSC may present as well-circumscribed periarticular or intraarticular hypoechoic masses with echogenic foci, thickening of the synovial membrane, expansion of the joint space, and secondary erosions [13]. Conventional X-rays and CT scans may reveal periarticular soft-tissue masses with internal mineralization, erosive changes, and background arthropathy [14].
The ultrasound findings for both PSC and SSC may present as well-circumscribed periarticular or intraarticular hypoechoic masses with echogenic foci, thickening of the synovial membrane, expansion of the joint space, and secondary erosions [13]. Conventional X-rays and CT scans may reveal periarticular soft-tissue masses with internal mineralization, erosive changes, and background arthropathy [14]. MRI is also useful in the evaluation of these lesions. On T1-weighted images, non-mineralized PSC and SSC lesions may appear as hyperintense intraarticular conglomerate masses compared to muscle [5,15]. On pulse sequences, small regions of low signal intensity may be seen within the mass, indicative of mineralized cartilaginous nodules [15]. MRI can also help define the boundaries of the tumor mass and assess possible invasion of the carpal bones, wrist joint, adjacent tendon sheaths, and the carpal tunnel [1]. In patients presenting with a palpable localized mass of the wrist, ultrasonography will often be the first choice of imaging [11].
MRI is also useful in the evaluation of these lesions. On T1-weighted images, non-mineralized PSC and SSC lesions may appear as hyperintense intraarticular conglomerate masses compared to muscle [5,15]. On pulse sequences, small regions of low signal intensity may be seen within the mass, indicative of mineralized cartilaginous nodules [15]. MRI can also help define the boundaries of the tumor mass and assess possible invasion of the carpal bones, wrist joint, adjacent tendon sheaths, and the carpal tunnel [1]. In patients presenting with a palpable localized mass of the wrist, ultrasonography will often be the first choice of imaging [11].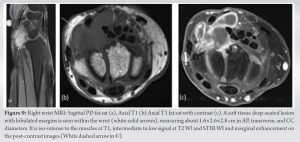 A well-circumscribed periarticular or intraarticular hypoechoic mass with many echogenic foci, thickening of the synovial membrane, expansion of the joint space, and secondary erosions the US characteristics in both PSC and SCC [13]. On conventional X-rays and CT, both PSC and SCH may reveal a periarticular soft-tissue mass with internal mineralization, erosive changes, and background arthropathy [14]. On MRI, T1-weighted images of non-mineralized PSC and SCH-related lesions can demonstrate intraarticular conglomerate masses that are hyperintense compared to muscle [5,15]. On a pulse sequence, small regions of low signal intensity can be seen within the mass denoting mineralized cartilaginous nodules [15]. In addition, MRI of the wrist can help delineate the boundaries of the tumor mass and evaluate possible invasion of the carpal bones, wrist joint, adjacent tendon sheaths, or the carpal tunnel [1]. A permeated, destructive, and infiltrative pattern on imaging rather than an erosive one, if present, can be indicative of malignant transformation [11]. From a histological perspective, cartilage cells in SCH often organize themselves in sheets rather than clustering as seen in PSC [9]. Hypercellularity with round and spindle cell morphology, necrosis, and myxoid alteration in the matrix is more prevalent in SCH, whereas PSC erodes the bone with pushing edges. In contrast, SCH has a permeative behavior and fills up the marrow gaps [16]. Cytogenetic and immunohistochemical data, such as the under-expression of BCL-2 (a cell survival marker) and the presence of a chromosomal translocation between chromosomes 1 and 14, can also provide important diagnostic information [12,17]. It is important to note that prior clinical history, concomitant benign arthropathies, and other professional opinions could create subconscious bias that radiologists must be aware of. For example, in Case 1, the patient had been treated for crystal arthropathy for 7 years, a history of hyperuricemia, a partial response to gout/CPPD therapy and involvement of several additional joints (most likely representing a concomitant pathology). Diagnosing malignant synovial-based tumors can pose a challenge, even for experienced radiologists utilizing the latest diagnostic imaging techniques. To ensure an accurate diagnosis, it is important for clinicians and radiologists to collaborate and regularly re-evaluate the differential diagnosis based on any new information that becomes available. This collaboration helps to distinguish between benign inflammatory synovial pathologies and malignancy. The treatment of SCH is surgical resection, which may include synovectomy, joint replacement, extra-articular excision with broad surgical margins, or amputation. The chosen method depends on the patient’s features, the size and location of the lesion, and the surgeon’s preference [18]. The treatment of low-grade malignant synovial-based tumors has been reported to be effective with synovectomy, which can be performed with or without joint replacement [19]. However, in cases where tumoral involvement of the neurovascular bundle precludes limb salvage, extra-articular excision with broad surgical margins or amputation is recommended [10]. This also highlights the importance of early identification of malignant transformation in PSC to ensure appropriate treatment can be initiated. The critical point when the suspicion of malignancy was significantly escalated was at face-to-face orthopedic consultant review in the first presented case. This emphasizes the paramount importance of early face-to-face surgical review in the suspected sarcoma pathway, ideally even before the patient reaches the sarcoma MDT discussion. In the context of presumed SC, there should be a low threshold for follow-up imaging, consideration of alternate sinister diagnoses and onward referral if the lesion is >5 cm in size at index presentation and/or demonstrates a significant increase in size when compared to previous imaging [20].
A well-circumscribed periarticular or intraarticular hypoechoic mass with many echogenic foci, thickening of the synovial membrane, expansion of the joint space, and secondary erosions the US characteristics in both PSC and SCC [13]. On conventional X-rays and CT, both PSC and SCH may reveal a periarticular soft-tissue mass with internal mineralization, erosive changes, and background arthropathy [14]. On MRI, T1-weighted images of non-mineralized PSC and SCH-related lesions can demonstrate intraarticular conglomerate masses that are hyperintense compared to muscle [5,15]. On a pulse sequence, small regions of low signal intensity can be seen within the mass denoting mineralized cartilaginous nodules [15]. In addition, MRI of the wrist can help delineate the boundaries of the tumor mass and evaluate possible invasion of the carpal bones, wrist joint, adjacent tendon sheaths, or the carpal tunnel [1]. A permeated, destructive, and infiltrative pattern on imaging rather than an erosive one, if present, can be indicative of malignant transformation [11]. From a histological perspective, cartilage cells in SCH often organize themselves in sheets rather than clustering as seen in PSC [9]. Hypercellularity with round and spindle cell morphology, necrosis, and myxoid alteration in the matrix is more prevalent in SCH, whereas PSC erodes the bone with pushing edges. In contrast, SCH has a permeative behavior and fills up the marrow gaps [16]. Cytogenetic and immunohistochemical data, such as the under-expression of BCL-2 (a cell survival marker) and the presence of a chromosomal translocation between chromosomes 1 and 14, can also provide important diagnostic information [12,17]. It is important to note that prior clinical history, concomitant benign arthropathies, and other professional opinions could create subconscious bias that radiologists must be aware of. For example, in Case 1, the patient had been treated for crystal arthropathy for 7 years, a history of hyperuricemia, a partial response to gout/CPPD therapy and involvement of several additional joints (most likely representing a concomitant pathology). Diagnosing malignant synovial-based tumors can pose a challenge, even for experienced radiologists utilizing the latest diagnostic imaging techniques. To ensure an accurate diagnosis, it is important for clinicians and radiologists to collaborate and regularly re-evaluate the differential diagnosis based on any new information that becomes available. This collaboration helps to distinguish between benign inflammatory synovial pathologies and malignancy. The treatment of SCH is surgical resection, which may include synovectomy, joint replacement, extra-articular excision with broad surgical margins, or amputation. The chosen method depends on the patient’s features, the size and location of the lesion, and the surgeon’s preference [18]. The treatment of low-grade malignant synovial-based tumors has been reported to be effective with synovectomy, which can be performed with or without joint replacement [19]. However, in cases where tumoral involvement of the neurovascular bundle precludes limb salvage, extra-articular excision with broad surgical margins or amputation is recommended [10]. This also highlights the importance of early identification of malignant transformation in PSC to ensure appropriate treatment can be initiated. The critical point when the suspicion of malignancy was significantly escalated was at face-to-face orthopedic consultant review in the first presented case. This emphasizes the paramount importance of early face-to-face surgical review in the suspected sarcoma pathway, ideally even before the patient reaches the sarcoma MDT discussion. In the context of presumed SC, there should be a low threshold for follow-up imaging, consideration of alternate sinister diagnoses and onward referral if the lesion is >5 cm in size at index presentation and/or demonstrates a significant increase in size when compared to previous imaging [20].
PSC and SCH are benign and malignant conditions of the synovial membrane and wrist joint, respectively. The diagnosis of SCH can often prove to be a challenge as the clinical and radiological manifestations are similar to those of severe PSC. Radiologists, orthopedic surgeons, and pathologists must work together to accurately diagnose and treat these conditions, using a combination of clinical, imaging, and histological characteristics.
Synovial osteochondromatosis must be considered as a differential for joint-based pathology where there is erosive change and marked soft-tissue proliferation with internal mineralization, even if not fitting the classical pattern for osteochondromatosis or there if there is a background arthropathy. There are currently no conclusive clinical or imaging indicators of malignant transition of PSC into SCH. Thus, it is essential to maintain a vigilant approach, with regular monitoring and evaluation, discussion at multi-disciplinary team meetings, face-to-face orthopedic consultation, and early histopathological diagnosis for accurate treatment and a positive prognosis.
References
- 1.Leung L. Painful swollen wrist: A case study. Aust Fam Physician 2013;42:301-3. [Google Scholar | PubMed]
- 2.Tomasevich KM, Moradi S, Lindsay AD. Chondrosarcoma arising in synovial chondromatosis of the hip: A case report. JBJS Case Connect 2021;11. [Google Scholar | PubMed]
- 3.Wittkop B, Davies AM, Mangham DC. Primary synovial chondromatosis and synovial chondrosarcoma: A pictorial review. Eur Radiol 2002;12:2112-9. [Google Scholar | PubMed]
- 4.McKenzie G, Raby N, Ritchie D. A pictorial review of primary synovial osteochondromatosis. Eur Radiol 2008;18:2662-9. [Google Scholar | PubMed]
- 5.Boninsegna E, Fassio A, Testoni M, Gatti D, Viapiana O, Mansueto G, et al. Radiological features of knee joint synovial chondromatosis. Reumatismo 2019;71:81-4. [Google Scholar | PubMed]
- 6.Liu X, Wan S, Shen P, Qiu Y, Sah MK, Abdelrehem A, et al. Diagnostic accuracy of synovial chondromatosis of the temporomandibular joint on magnetic resonance imaging. PLoS One 2019;14:e0209739. [Google Scholar | PubMed]
- 7.Wenger DE, Sundaram M, Unni KK, Janney CG, Merkel K. Acral synovial chondrosarcoma. Skeletal Radiol 2002;31:125-9. [Google Scholar | PubMed]
- 8.Bertoni F, Unni KK, Beabout JW, Sim FH. Chondrosarcomas of the synovium. Cancer 1991;67:941-6. [Google Scholar | PubMed]
- 9.Biazzo A, Confalonieri N. Systematic review and meta-analysis synovial chondrosarcoma. Ann Transl Med 2016;4:280. [Google Scholar | PubMed]
- 10.Campanacci DA, Matera D, Franchi A, Capanna R. Synovial chondrosarcoma of the hip: Report of two cases and literature review. Chir Organ Mov 2008;92:139-44. [Google Scholar | PubMed]
- 11.Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics 2007;27:1465-88. [Google Scholar | PubMed]
- 12.Sperling BL, Angel S, Stoneham G, Chow V, Mcfadden A, Chibbar R. Synovial chondromatosis and chondrosarcoma: A diagnostic dilemma. Sarcoma 2003;7:69-73. [Google Scholar | PubMed]
- 13.Campeau NG, Lewis BD. Ultrasound appearance of synovial osteochondromatosis of the shoulder. Mayo Clin Proc 1998;73:1079-81. [Google Scholar | PubMed]
- 14.Van der Valk MR, Veltman ES, Assink J, Veen MR. Synovial chondromatosis of the hip, a case report and literature review. J Orthop 2019;16:249-53. [Google Scholar | PubMed]
- 15.Sheldon PJ, Forrester DM, Learch TJ. Imaging of intraarticular masses. Radiographics 2005;25:105-19. [Google Scholar | PubMed]
- 16.Anract P, Katabi M, Forest M, Benoit J, Witvoët J, Tomeno B. Synovial chondromatosis and chondrosarcoma. A study of the relationship between these two diseases. Rev Chir Orthop Reparatrice Appar Mot 1996;82:216-24. [Google Scholar | PubMed]
- 17.Kyriazoglou AI, Rizou H, Dimitriadis E, Arnogiannaki N, Agnantis N, Pandis N. Cytogenetic analysis of a low-grade secondary peripheral chondrosarcoma arising in synovial chondromatosis. In Vivo 2013;27:57-60. [Google Scholar | PubMed]
- 18.Duif C, Von Schulze Pellengahr C, Ali A, Hagen M, Ficklscherer A, Stricker I, et al. Primary synovial chondromatosis of the hip-is arthroscopy sufficient? A review of the literature and a case report. Technol Health Care 2014;22:667-75. [Google Scholar | PubMed]
- 19.Hallam P, Ashwood N, Cobb J, Fazal A, Heatley W. Malignant transformation in synovial chondromatosis of the knee? Knee 2001;8:517-24. [Google Scholar | PubMed]
- 20.Thomas BP, Sasi K, Pallapati SC, Mathew A, Sreekanth R, Thomas M. Malignant tumours of the hand and wrist. Indian J Plast Surg 2011;44:337-47. [Google Scholar | PubMed]