A transposition flap reconstruction is an option for large defects after soft-tissue sarcoma resection in the buttock.
Dr. Akio Sakamoto, Department of Orthopaedic Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan. E-mail: akiosaka@kuhp.kyoto-u.ac.jp
Introduction:Large defects following resection in the gluteal region are challenging. Of note, there are a limited number of fairly morbid options for reconstruction.
Case Report:A 65-year-old female presented with complaints of an enlarging mass in the left buttock over the past several months. A high-grade sarcoma was diagnosed based on a biopsy. The final diagnosis was an undifferentiated pleomorphic sarcoma based on the resected tumor. An 11-cm tumor with surrounding tissues, including the great gluteal muscle, was resected, which resulted in a 17-cm full thickness defect. The defect was reconstructed with a transposition flap elevated from the lateral thorax. A transposition flap can cover large buttock defects without sacrificing other muscles.
Conclusion:Moreover, a transposition flap is esthetically acceptable because most of the operative scar is within the buttock area. A transposition flap reconstruction is one of the several options for large defects after soft-tissue sarcoma resection in the buttock.
Keywords:Buttock, resection, reconstruction, musculocutaneous flap, soft-tissue sarcoma.
The gluteal region is a site of pressure and shear. Local flap reconstruction in the gluteal region is used for pressure sores over bony prominences of the ischium and sacrum so that the reconstruction can withstand resistance of pressure and shear stress [1]. Soft-tissue defects in the buttock region after resection of soft-tissue sarcomas need reconstruction involving flaps; however, especially when the defect is large, there are a limited number of options for reconstruction because of limited donor site availability [2, 3]. A transposition flap is a local flap with a random pattern that does not require use of microsurgical techniques. A transposition flap in the buttock region has been reported for repair of defects following pressure sores and pilonidal sinus resection [4].
In the present case report, a transposition flap was used for reconstruction after resection of an undifferentiated pleomorphic sarcoma in the buttock for a large defect.
A 65-year-old female presented with complaints of a painless mass on the left gluteal region of the buttock that increased in size over several months. Magnetic resonance imaging revealed a subcutaneous tumor with a maximum diameter of 11 cm. The tumor had a cystic appearance and contained liquid with slightly high-signal intensity on the T1-weighted image and high-signal intensity on the T2-weighted image. The periphery of the cystic wall was thick with a solid neoplastic lesion and intermediate signal intensity on T1- and T2-weighted images. The tumor extended to the fascia of the great gluteal muscle and the gluteal muscle was displaced. 18F-fluorodeoxyglucose positron emission tomography/computed tomography (CT) showed a high standardized uptake value maximum at the periphery of the tumor (Fig. 1). 
The histologic evaluation of a needle biopsy was characterized by a proliferation of malignant pleomorphic cells, thus suggesting a high-grade malignancy. No lung metastasis was identified. The tumor resection was planned with the resection of underlying gluteal muscle as well as the surrounding skin and subcutaneous tissues >3 cm from the tumor, resulting in a full thickness defect in the buttock 17 cm in maximum diameter. A transposition flap reconstruction was designed in which tissue was donated from the lateral thorax. The flap had no circulatory impairment after the operation (Fig. 2).
During rehabilitation there were no restrictions for the post-operative sitting and standing protocols, the purpose of which is to protect the flap. Limitation on daily activity was recommended. The majority of the gluteal muscle was resected; however, the patient felt no specific disturbance after the resection of the great gluteus muscle and the patient’s gait was not affected.
The histopathology report confirmed an undifferentiated pleomorphic sarcoma. The surgical margin had no tumor cells and post-operation radiotherapy was not performed. The patient was satisfied with the aesthetics of the flap because most of the surgical scar was covered by underwear.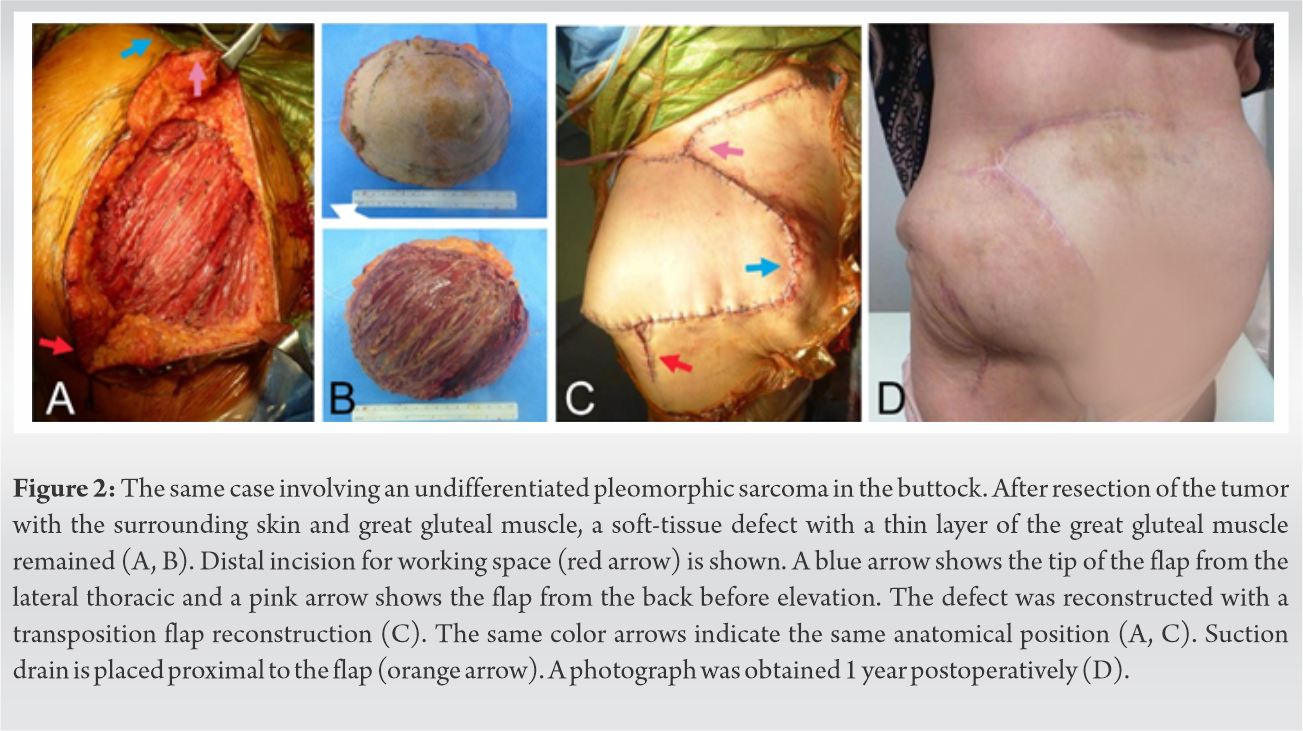
In cases involving large defects in the gluteal region, free flaps are necessary, such as latissimus dorsi flaps [5]. Free flap reconstruction requires a microvascular technique and the gluteal region has limited recipient vessels [6, 7]. It has been reported, however, that free flaps have higher rates of complications (43%), re-operation (13%) than the complications (17%), and re-operation rates (4.3%) for local flaps used for soft-tissue sarcoma defects [8]. Moreover, a transposition flap does not require exposure of donor vessels for free flaps, and thus less exposure of the deep tissue is an advantage in terms of reducing the possibility of tumor spread.
In the present case report, a large defect in the gluteal region was reconstructed with a transposition flap. Transposition flaps have a random pattern blood supply. In reconstruction of defects in the buttock region, superior gluteal artery perforator (SGAP)/inferior gluteal artery perforator (IGAP) flaps are known. These flaps have been applied for sacral and ischial soft-tissue reconstruction of pressure sores involving the sacrum, ischium, and pilonidal sinuses [9]. These flaps are raised based on one or two perforators. In resection of a sarcoma in the buttock, resected tissue could include large tissue, possibly including the great gluteal muscle and the perforators. Therefore, the indication for SGAP/IGAP flaps would be restricted.
During rehabilitation of the present case, there was no restriction for the post-operative sitting protocol because the flap is not covered over the ischial tuberosity where the pressure is exacerbated by sitting. The transposition flap was not affected in the standing position. A lower impact during sitting and standing is a merit of the flap. In terms of function, transposition flaps are fasciocutaneous flaps that do not contain muscle, and are thus different from other muscle flaps. Therefore, functional loss of transposition flaps would occur less often. In addition, the patient was satisfied with the aesthetics of the flap because most surgical wounds were within the buttock region and covered by underwear.
A transposition flap was applied for the defect in the buttock after malignant soft-tissue tumor resection. In comparison to other flaps with perforators or free flaps, a transposition flap requires less operative time, less functional loss, and greater esthetic satisfaction. There is no need for exposure of deep tissue for perforators or donor vessels, contributing to less possibility of spreading tumor. Transposition flaps are an option for reconstructing large gluteal defects after malignant soft-tissue tumor resection.
References
- 1.Bauer J, Phillips LG. MOC-PSSM CME article: Pressure sores. Plast Reconstr Surg 2008;121 Suppl 1:1-10. [Google Scholar]
- 2.Nel CP, Daya M. Buttock reconstruction in sarcoma surgery: An esthetic sigmoidplasty closure for large circular defects using double opposing skin flaps. Plast Reconstr Surg Glob Open 2016;4:e1039. [Google Scholar]
- 3.Pu LL. Reconstruction of a large gluteal soft-tissue defect with the double-opposing V-Y fasciocutaneous advancement flap. Plast Reconstr Surg 2007;119:599-603. [Google Scholar]
- 4.Özcan B, İlkgül Ö. Contralateral Limberg flap reconstruction for pilonidal disease recurrence. Asian J Surg 2019;42:787-91. [Google Scholar]
- 5.Aggarwal S, Pennington D. Reconstruction of gluteal defects using free flaps. J Plast Reconstr Aesthet Surg 2013;66:1149-52. [Google Scholar]
- 6.Hung SJ, Chen HC, Wei FC. Free flaps for reconstruction of the lower back and sacral area. Microsurgery 2000;20:72-6. [Google Scholar]
- 7.Harris GD, Lewis VL, Nagle DJ, Edelson RJ, Kim PS. Free flap reconstruction of the lower back and posterior pelvis: Indications, principles, and techniques. J Reconstr Microsurg 1988;4:169-78. [Google Scholar]
- 8.Eward WC, Lazarides AL, Griffin AM, O’Donnell PW, Sternheim A, O’Neill A, et al. Superficial soft-tissue sarcomas rarely require advanced soft-tissue reconstruction following resection. Plast Reconstr Surg Glob Open 2017;5:e1553. [Google Scholar]
- 9.Korambayil PM, Allalasundaram K, Balakrishnan T. Perforator propeller flaps for sacral and ischial soft tissue reconstruction. Indian J Plast Surg 2010;43:151-7. [Google Scholar]








